The most favored strategy for bifurcation lesion is stenting main vessel with provisional side branch (SB) stenting. This study was performed to elucidate predictors for SB failure during this provisional strategy. The study population was patients from 16 centers in Korea who underwent drug-eluting stent implantation for bifurcation lesions with provisional strategy (1,219 patients and 1,236 lesions). On multivariate analysis, the independent predictors for SB jailing after main vessel stenting were SB calcification, large SB reference diameter, severe stenosis of SB, and not taking clopidogrel. Regarding SB compromise, however, the independent predictors were true bifurcation lesion and small SB reference diameter, whereas possible predictors were parent vessel thrombus and parent vessel total occlusion. In addition, SB predilation helps us to get favorable SB outcome. The diameter of SB ostium after main vessel stenting became similar between severe SB lesions treated with predilation and mild SB lesions not treated with predilation. In conclusion, SB calcification, less clopidogrel use, large SB reference diameter, and high SB diameter stenosis are independent predictors for SB jailing, and true bifurcation and small SB reference diameter are independent predictors for SB compromise after main vessel stenting.
Coronary bifurcation lesion is not infrequent during percutaneous coronary interventions (PCIs), occurring in ∼15%. Since introduction of PCI in clinical field, it has been challenging. Although there has been much progress in PCI technique and device, PCI of bifurcation is still problematic. Owing to anatomic structure, there could be several problems including plaque shift, carina shift, jailing or compromise of side branch (SB), the protruded stent strut in the lumen, and so on during PCI of bifurcation lesion. For now, the favored strategy is provisional stenting strategy. Nevertheless, there exist certain situations in which the 2-stent strategy needs to be considered, and there have been high crossover rates from 1- to 2-stent strategy. However, there is a paucity of data regarding important predictors for SB failure during provisional strategy. In the present study, we sought to elucidate these predictors from the Korean multicenter coronary bifurcation stenting registry.
Methods
This registry was introduced elsewhere. The Coronary Bifurcation registry (COBIS) is a registry that included bifurcation lesions treated with drug-eluting stent (DES) from 17 hospitals in Republic of Korea. The data of consecutive patients treated with DES for coronary bifurcation lesions from January 2004 to June 2006 were included in this registry. All data were controlled by independent managers in a fundamental center, Samsung medical center. The study fully complied with the Declaration of Helsinki and was approved by the institutional review board of each participating center, and the requirement for informed consent was waived ( Clinicaltrials.gov number: NCT00851526 ).
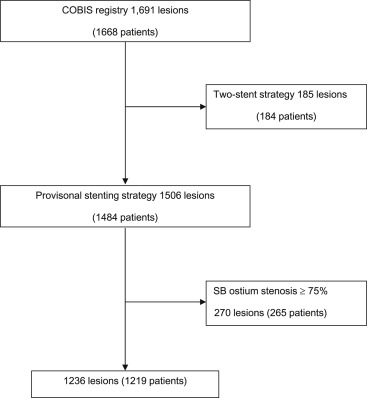
The COBIS registry included the patients meeting following criteria from January 2004 to June 2006: (1) age ≥18 years, (2) any type of de novo bifurcation lesion with a parent vessel and SB diameter ≥2.5 and ≥2.0 mm, respectively, by visual estimation, and (3) treated with DES. Exclusion criteria were cardiogenic shock, ST-segment elevation acute myocardial infarction (MI) within 48 hours, expected survival <1 year, left main bifurcation, or allergy to the antiplatelet drugs. Among the patients included in the COBIS registry, those patients who were treated with provisional stenting approach were included regardless of whether finally the lesion was treated with 1-stent stenting. Moreover, the lesions of which SB ostium stenosis ≥75% were excluded. As such, final cohort for analysis in this study was defined.
The patients were treated with aspirin and clopidogrel before procedure. Those received oral 300 to 600 mg loading dose of clopidogrel before the index PCI if the patient was not taking clopidogrel within 24 hours before procedure. Aspirin was prescribed indefinitely, and clopidogrel was continued for at least 6 months according to respective institutional practice. Other medications, techniques and devices were left to the operator’s preference, such as anticoagulation therapy during the procedure, co-use of glycoprotein GPIIb/IIIa inhibitors, access site, type of DES, stenting techniques, use of intravascular ultrasound, and intra-aortic balloon pump.
At least 2 projections of the lesion were obtained in orthogonal views. After getting angiogram, the operator decided which strategy would be used, that is to say, provisional approach or SB stenting first. This study cohort encompassed only the bifurcation lesion treated with provisional strategy. During provisional strategy, a DES was implanted at main vessel, and then, the angiogram was obtained to evaluate main vessel and SB state. It was decided by the operator whether the additional intervention for SB including balloon angioplasty or bailout stenting would be done. The procedure was considered complete when the patient was transferred out of the catheterization laboratory table.
Lesion and procedural characteristics were analyzed, and quantitative analysis for coronary angiography performed at baseline and at the completion of the provisional stenting was done. SB failure includes SB compromise and SB jailing. SB compromise is defined as SB acute closure or Thrombolysis In Myocardial Infarction flow ≤2, whereas SB jailing is defined as SB stenosis ≥75% after main vessel stenting.
All categorical variables were expressed as proportions and were compared with the chi-square test or Fisher’s exact test. All continuous variables were described as mean value ± SD and compared with the Student’s t test. Univariate analyses along with multivariate analyses using a stepwise logistic regression were conducted to identify predictors for SB jailing or compromise. All statistical analyses were performed using SPSS 12.0 (SPSS Inc., Chicago, Illinois), and a p value <0.05 was considered statistically significant.
Results
From January 2004 to June 2006, 1,691 bifurcation lesions in 1,668 patients were enrolled into the registry and 1,506 lesions in 1,484 patients were treated with provisional strategies. The final cohort included in this study was composed of 1,236 lesions from 1,219 patients ( Figure 1 ).
The baseline patient characteristics are listed in Table 1 and the baseline angiographic and procedural characteristics of lesion are listed in Table 2 . In total, the incidence of SB jailing and compromise after main vessel stenting were 9.6% (119 of 1,236 lesions) and 5.4% (67 of 1,236 lesions), respectively. Tables 1 and 2 also summarize baseline clinical, angiographic, and procedural findings in jailed SB group and non-jailed SB group. Regarding baseline clinical profiles, the jailed SB patients were less likely to take periprocedural clopidogrel. The jailed SB group showed higher mean serum creatinine level than non-jailed SB group. But the frequency of chronic renal failure was not different between the groups. The frequency of hypertension, diabetes, and dyslipidemia was marginally lower in the jailed SB group (p = 0.076, 0.066, and 0.064, respectively). However, there were no significant differences in the frequency of female gender, current smokers, and history of MI or stroke between the groups. As for baseline angiographic characteristics, jailed SB group showed higher frequency of true bifurcation and calcification in SB, larger SB reference diameter, more severe diameter stenosis of main branch (MB) ostium, more severe diameter stenosis of SB and SB ostium, and longer SB lesion that are described in Table 3 .
| Variable | Total (n = 1219) | Jailed SB (n = 118) | Non-Jailed SB (n = 1101) | p Value | Compromised SB (n = 66) | Non-compromised SB (n = 1153) | p Value |
|---|---|---|---|---|---|---|---|
| Women | 406 (33.3%) | 35(30%) | 371(33.7%) | 0.377 | 25(38%) | 381(33.0%) | 0.418 |
| Age (years) | 62.17 ± 10.29 | 62.27 ± 9.93 | 62.16 ± 10.33 | 0.908 | 63.45 ± 9.23 | 62.09 ± 10.35 | 0.296 |
| Current smoking | 295 (24.2%) | 29(25%) | 266(24.2%) | 0.920 | 15(23%) | 280(24.3%) | 0.774 |
| Acute coronary syndrome at the index procedure | 682 (55.9%) | 70(59%) | 612(55.6%) | 0.437 | 41(62%) | 641(55.6%) | 0.299 |
| Previous MI | 98 (8.0%) | 9(8%) | 89(8.1%) | 0.862 | 3(5%) | 95(8.2%) | 0.283 |
| History of stroke | 65 (5.3%) | 6(5%) | 59(5.4%) | 0.900 | 3(5%) | 62(5.4%) | 1.000 |
| Hypertension | 723 (59.3%) | 61(52%) | 662(60.1%) | 0.076 | 35(53%) | 688(59.7%) | 0.286 |
| Diabetes mellitus | 380 (31.2%) | 28(24%) | 352(32.0%) | 0.066 | 17(26%) | 363(31.5%) | 0.329 |
| Dyslipidemia ∗ | 382 (31.3%) | 28(24%) | 354(32.2%) | 0.061 | 21(32%) | 361(31.3%) | 0.931 |
| Chronic renal insufficiency | 45 (3.7%) | 2(2%) | 43(3.9%) | 0.307 | 2(3%) | 43(3.7%) | 1.000 |
| Creatinine (mg/dl) | 1.14 ± 1.37 | 1.00 ± 0.52 | 1.16 ± 1.43 | 0.016 | 1.12 ± 0.93 | 1.14 ± 1.39 | 0.874 |
| Total cholesterol (mg/dl) | 175.66 ± 39.78 | 176.57 ± 42.65 | 175.56 ± 39.47 | 0.793 | 174.89 ± 34.71 | 175.70 ± 40.07 | 0.873 |
| Low-density lipoprotein cholesterol (mg/dl) | 113.08 ± 36.10 | 111.32 ± 36.56 | 113.27 ± 36.07 | 0.598 | 117.90 ± 32.74 | 112.80 ± 36.29 | 0.287 |
| High-density lipoprotein cholesterol (mg/dl) | 42.98 ± 11.71 | 41.70 ± 10.29 | 43.12 ± 11.85 | 0.234 | 43.62 ± 11.16 | 42.94 ± 11.75 | 0.657 |
| Ejection fraction (%) | 59.65 ± 11.25 | 60.71 ± 10.16 | 59.54 ± 11.37 | 0.362 | 59.59 ± 11.58 | 59.65 ± 11.24 | 0.972 |
| Periprocedural aspirin † | 1052 (86.3%) | 97(82%) | 955(86.7%) | 0.173 | 60(91%) | 992(86.0%) | 0.263 |
| Periprocedural clopidogrel † | 1021 (83.8%) | 89(75%) | 932(84.7%) | 0.010 | 57(86%) | 964(83.6%) | 0.555 |
| Periprocedural cliostazol † | 113 (9.3%) | 11(9%) | 102(9.3%) | 0.984 | 5(8%) | 108(9.4%) | 0.626 |
| Periprocedural abciximab † | 39 (3.2%) | 2(2%) | 37(3.4%) | 0.577 | 4(6%) | 35(3.0%) | 0.156 |
∗ Dyslipidemia was defined by total cholesterol > 200 mg/dl, LDL > 130 mg/dl, HDL < 30 mg/dl, triglycerides > 150 mg/dl, or use of lipid-lowering agents for the history of dyslipidemia.
| Variable | Total (n = 1236) | Jailed SB (n = 119) | Non-jailed SB (n = 1117) | p Value | Compromised SB (n = 67) | Non-compromised SB (n = 1169) | p Value |
|---|---|---|---|---|---|---|---|
| Location of diseased vessels | 0.130 | 0.240 | |||||
| Left anterior descending coronary artery | 923 (74.7%) | 95(80%) | 828(74.1%) | 44 (66%) | 879 (75.2%) | ||
| Left circumflex coronary artery | 245 (19.8%) | 22(18%) | 223(20.0%) | 227(19%) | 18 (26.9%) | ||
| Right coronary artery | 68 (5.5%) | 2(2%) | 66(5.9%) | 5 (7%) | 63 (5.4%) | ||
| Medina classification | 0.012 | 0.020 | |||||
| 001 | 8 (0.6%) | 1(1%) | 7(0.6%) | 0 (0%) | 8 (0.7%) | ||
| 010 | 153 (12.4%) | 7(6%) | 146(13.1%) | 5 (7%) | 148 (12.7%) | ||
| 011 | 131 (10.6%) | 14(12%) | 117(10.5%) | 4 (6%) | 127 (10.9%) | ||
| 100 | 101 (8.2%) | 5(4%) | 96(8.6%) | 3 (4%) | 98 (8.4%) | ||
| 101 | 80 (6.5%) | 10(8%) | 70(6.3%) | 5 (7%) | 75 (6.4%) | ||
| 110 | 168 (13.6%) | 10(8%) | 158(14.1%) | 4 (6%) | 164 (14.0%) | ||
| 111 | 595 (48.1%) | 72(61%) | 523(46.8%) | 46 (69%) | 549 (47.0%) | ||
| True bifurcation (011, 101, 111) | 806 (65.2%) | 96(81%) | 710(63.6%) | 0.000 | 55 (82%) | 751 (64.2%) | 0.003 |
| Total occlusion of MV ∗ | 96 (7.8%) | 7(6%) | 89(8.0%) | 0.419 | 11 (6%) | 85 (7.3%) | 0.007 |
| Thrombus in MV † | 49 (4.0%) | 2(2%) | 47(4.2%) | 0.222 | 7 (10%) | 42 (3.6%) | 0.014 |
| Total occlusion of SB | 39 (3.2%) | 3(3%) | 36(3.2%) | 1.000 | 4 (6%) | 35 (3.0%) | 0.156 |
| Thrombus in SB | 7 (0.6%) | 1(1%) | 6(0.5%) | 0.509 | 0 (0%) | 7 (0.6%) | 1.000 |
| Calcification in MV ‡ | 289 (23.4%) | 29(24%) | 260(23.3%) | 0.789 | 22 (33%) | 267 (22.8%) | 0.060 |
| Calcification in SB | 103 (8.3%) | 19(16%) | 84(7.5%) | 0.002 | 6 (9%) | 97 (8.3%) | 0.850 |
| Intravascular ultrasound guidance | 379 (30.7%) | 36(30%) | 343(30.7%) | 0.918 | 20 (30%) | 359 (30.7%) | 0.882 |
| Main vessel stent type | 0.013 | 0.660 | |||||
| Sirolimus-eluting stent | 771 (62.4%) | 85 (72.0%) | 686 (63.3%) | 38 (58.5%) | 733 (64.5%) | ||
| Paclitaxel-eluting stent | 426 (34.5%) | 31 (26.3%) | 395 (36.4%) | 27 (41.5%) | 399 (35.1%) | ||
| Bare-metal stent § | 2 (0.2%) | 0 (0%) | 2 (0.2%) | 0 (0%) | 2 (0.2%) | ||
| Other stent | 3(0.2%) | 2 (1.7%) | 1 (0.1%) | 0 (0%) | 3 (0.3%) | ||
| No. of stents in MV | 1.20 ± 0.45 | 1.24 ± 0.45 | 1.20 ± 0.45 | 0.425 | 1.18 ± 0.42 | 1.21 ± 0.45 | 0.640 |
| No. of stents in SB | 0.07 ± 0.26 | 0.06 ± 0.24 | 0.08 ± 0.26 | 0.514 | 0.16 ± 0.37 | 0.07 ± 0.25 | 0.042 |
| SB predilation | 173 (14.0%) | 21 (18%) | 152 (13.6%) | 0.227 | 11 (16%) | 162 (13.9%) | 0.557 |
| Final kissing inflation | 417 (33.7%) | 62(52%) | 355(31.8%) | 0.000 | 22 (33%) | 395 (33.8%) | 0.872 |
§ Implanted along with drug-eluting stents for the bifurcation lesions.
| Variable | Total (n = 1236) | Jailed SB (n = 119) | Non-jailed SB (n = 1117) | p Value | Compromised SB (n = 67) | Non-compromised SB (n = 1169) | p Value |
|---|---|---|---|---|---|---|---|
| Baseline | |||||||
| Main vessel angle ∗ | 148.3 ± 17.7 | 146.3 ± 16.0 | 148.5 ± 17.8 | 0.193 | 150.7 ± 17.7 | 148.2 ± 17.6 | 0.252 |
| Bifurcation angle † | 53.0 ± 18.0 | 51.8 ± 18.3 | 53.1 ± 18.0 | 0.449 | 51.7 ± 18.3 | 53.1 ± 18.0 | 0.529 |
| PV reference diameter | 3.08 ± 0.52 | 3.14 ± 0.43 | 3.08 ± 0.53 | 0.151 | 3.03 ± 0.46 | 3.09 ± 0.53 | 0.396 |
| MB reference diameter | 2.46 ± 0.47 | 2.48 ± 0.46 | 2.45 ± 0.48 | 0.506 | 2.39 ± 0.42 | 2.46 ± 0.48 | 0.280 |
| SB reference diameter | 2.09 ± 0.42 | 2.20 ± 0.43 | 2.08 ± 0.41 | 0.002 | 1.92 ± 0.38 | 2.10 ± 0.42 | 0.001 |
| Minimal luminal diameter of PV | 1.48 ± 0.82 | 1.44 ± 0.74 | 1.48 ± 0.83 | 0.593 | 1.32 ± 0.71 | 1.49 ± 0.83 | 0.102 |
| Diameter stenosis of PV | 51.9 ± 24.7 | 54.3 ± 22.0 | 51.6 ± 24.9 | 0.208 | 55.9 ± 23.7 | 51.7 ± 24.7 | 0.169 |
| Minimal luminal diameter of MB ostium | 1.31 ± 18.02 | 1.20 ± 0.57 | 1.32 ± 0.63 | 0.048 | 1.28 ± 0.62 | 1.31 ± 0.62 | 0.669 |
| Diameter stenosis of MB ostium | 46.5 ± 23.6 | 52.2 ± 21.6 | 45.9 ± 23.7 | 0.006 | 46.7 ± 25.6 | 46.5 ± 23.5 | 0.952 |
| Minimal luminal diameter of MB | 1.58 ± 0.70 | 1.59 ± 0.72 | 1.58 ± 0.70 | 0.912 | 1.49 ± 0.68 | 1.59 ± 0.71 | 0.273 |
| Diameter stenosis of MB | 36.1 ± 24.9 | 37.7 ± 24.6 | 36.0 ± 24.9 | 0.478 | 38.2 ± 25.8 | 36.0 ± 24.8 | 0.484 |
| Minimal luminal diameter of SB ostium | 1.32 ± 0.53 | 1.11 ± 0.49 | 1.34 ± 0.53 | 0.000 | 1.09 ± 0.39 | 1.33 ± 0.53 | 0.000 |
| Diameter stenosis of SB ostium | 37.1 ± 21.0 | 49.9 ± 18.4 | 35.7 ± 20.8 | 0.000 | 42.7 ± 18.9 | 36.7 ± 21.1 | 0.024 |
| Minimal luminal diameter of SB | 1.58 ± 0.54 | 1.59 ± 0.60 | 1.58 ± 0.53 | 0.834 | 1.40 ± 0.49 | 1.59 ± 0.54 | 0.006 |
| Diameter stenosis of SB | 24.8 ± 18.9 | 28.3 ± 20.4 | 24.5 ± 18.7 | 0.037 | 26.7 ± 20.9 | 24.7 ± 18.8 | 0.409 |
| MV lesion length | 18.6 ± 10.9 | 20.4 ± 10.4 | 18.4 ± 10.9 | 0.062 | 19.1 ± 9.9 | 18.6 ± 10.9 | 0.710 |
| SB lesion length | 4.64 ± 5.88 | 6.19 ± 5.97 | 4.47 ± 5.85 | 0.002 | 6.50 ± 6.62 | 4.53 ± 5.82 | 0.008 |
| Difference between PV and MB reference diameters (PV-MB) | 0.63 ± 0.48 | 0.65 ± 0.43 | 0.62 ± 0.49 | 0.503 | 0.63 ± 0.51 | 0.63 ± 0.48 | 0.890 |
| Post-MV stenting | |||||||
| Minimal luminal diameter of PV | 2.75 ± 0.50 | 2.64 ± 0.45 | 2.76 ± 0.50 | 0.018 | 2.72 ± 0.42 | 2.75 ± 0.50 | 0.612 |
| Diameter stenosis of PV | 11.7 ± 13.0 | 15.9 ± 12.3 | 11.2 ± 13.0 | 0.000 | 11.6 ± 14.0 | 11.7 ± 13.0 | 0.959 |
| Minimal luminal diameter of MB ostium | 2.60 ± 0.47 | 2.53 ± 0.41 | 2.61 ± 0.48 | 0.042 | 2.64 ± 0.49 | 2.60 ± 0.47 | 0.461 |
| Diameter stenosis of MB ostium | -3.41 ± 17.7 | -1.05 ± 15.5 | -3.66 ± 17.9 | 0.126 | -8.46 ± 19.7 | -3.12 ± 17.7 | 0.016 |
| Minimal luminal diameter of MB | 2.51 ± 0.51 | 2.50 ± 0.45 | 2.51 ± 0.52 | 0.821 | 2.48 ± 0.54 | 2.51 ± 0.51 | 0.707 |
| Diameter stenosis of MB | 0.65 ± 18.0 | 0.45 ± 15.1 | 0.67 ± 18.3 | 0.899 | -1.46 ± 19.0 | 0.77 ± 18.0 | 0.325 |
| Minimal luminal diameter of SB ostium | 1.10 ± 0.56 | 0.35 ± 0.20 | 1.18 ± 0.52 | 0.000 | 0.83 ± 0.51 | 1.12 ± 0.55 | 0.000 |
| Diameter stenosis of SB ostium | 47.5 ± 23.7 | 84.4 ± 8.27 | 43.5 ± 21.2 | 0.000 | 55.3 ± 26.8 | 47.0 ± 23.4 | 0.005 |
| Minimal luminal diameter of SB | 1.57 ± 0.56 | 1.35 ± 0.78 | 1.60 ± 0.53 | 0.001 | 1.27 ± 0.72 | 1.59 ± 0.55 | 0.001 |
| Diameter stenosis of SB | 25.3 ± 21.6 | 40.3 ± 31.3 | 23.7 ± 19.6 | 0.000 | 32.5 ± 35.7 | 24.9 ± 20.4 | 0.091 |
| SB jailing | 119 (9.6%) | 119 (100%) | 0 (0%) | 0.000 | 12 (18%) | 107 (9.2%) | 0.072 |
| SB acute closure during procedure | 67 (5.4%) | 12(10%) | 55(4.9%) | 0.018 | 67 (100%) | 0 (0%) | 0.000 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


