Introduction
A sedentary lifestyle has been established as a major modifiable coronary risk factor by the American Heart Association.1 Unfortunately, approximately 70% of adults in the United States are sedentary or underactive, and almost one-half of America’s young people aged 12–21 years are not physically active on a regular basis.2 The reasons for this observation are closely related to industrialization, automation, and the resultant decreased requirement for occupational, household, and leisure-time physical activity in the past several decades. The need to walk, climb stairs, perform energy-requiring tasks around the home or engage in physical activity in the workplace has dramatically decreased for the vast majority of people. In the 21st century, individuals must make a conscious choice to be physically active.
The definitions of physical activity, exercise and cardiore-spiratory fitness are important to the understanding of this chapter. The 1996 National Institutes of Health Consensus Conference on Physical Activity and Cardiovascular Health defined physical activity as “bodily movement produced by skeletal muscles that requires energy expenditure and produces health benefits”.3 Physical activity is informal in nature and structure and includes everyday activities such as walking or bicycling or stair climbing for transportation, as well as household or yard tasks, occupational tasks and low-intensity sports such as golf. Physical activity occurs within the structure of the requirements of usual daily living. Recently, energy expenditure due to changes in posture and movement associated with the routines of daily life, termed non-exercise activity thermogenesis (NEAT), was compared in lean and obese subjects.4 Lean subjects expended an average of 350 kilocalories more each day in NEAT than did obese subjects, underscoring the importance of physical activity in coronary risk.
Exercise, also called exercise training, was defined as “planned, structured, and repetitive bodily movement done to improve or maintain one or more components of physical fitness”.3 It is characterized by periodic formal workouts involving sustained moderate-to high-intensity effort. It usually involves specific clothing, such as footwear, and equipment, as is present in fitness facilities, but is not an absolutely necessary part of the daily routine. It may involve sporting activities, such as basketball, racquet sports or soccer (non-American football).
Cardiorespiratory fitness (peak exercise oxygen uptake) is defined as the capacity to take in and process oxygen for the production of energy via aerobic metabolism for physical activity or exercise. This component of physical fitness is most closely associated with coronary risk. Cardiorespi-ratory fitness is directly influenced by the performance of habitual exercise training, but is also influenced by genetic potential,5 age and gender, as well as by underlying chronic diseases that affect the cardiorespiratory systems, nervous system, blood and musculoskeletal system.
The goal of this chapter is to discuss the roles of physical activity and formal exercise in the prevention and rehabilitation (secondary prevention) of coronary heart disease (CHD). The following topics are included for this purpose:
- observational data concerning the relationship of occupational and leisure-time physical activity and exercise to coronary risk
- studies evaluating the relationship of cardiorespiratory fitness or change in cardiorespiratory fitness and coronary risk
- data addressing the results of exercise training in persons with established CHD with regard to disease progression and coronary events
- the risks of acute exercise
- potential mechanisms for the observed cardioprotective effects of physical activity and exercise training
- recommendations for physical activity and exercise training.
Observational studies in the prevention of coronary heart disease
Due to methodologic and ethical issues, there are no randomized trials of physical activity and exercise on clinical cardiovascular outcomes. Observational studies have been performed, however. An inherent limitation of observational data is selection bias. For example, individuals may be sedentary because of undetected pathology or physically active because of superior general health. However, investigations of either occupational or leisure time physical activity, exercise and coronary risk provide valuable information if the studies include large numbers of subjects.
Studies of occupational physical activity attempt to quantify the amount of physical activity that occurs during the performance of job duties. Most studies of this type report occupational physical activity by category, i.e. most active, moderately active, and least active. Because the requirement for occupational physical activity has decreased precipitously in the last several decades in developed countries, investigators have more recently turned attention to the relationship of leisure-time physical activity and exercise to coronary risk. This type of exercise is undertaken by people during discretionary time outside work, domestic tasks, and other routine activities of daily living.
Occupational physical activity
Multiple investigators have demonstrated an inverse relationship between the amount and intensity of job-related physical activity and coronary risk. The following three studies are illustrative of this finding.
A large population of US railroad workers (191 609 men, age range 30–64 years) was evaluated by Taylor and associates.6 Occupational physical activity was determined by job class: sedentary clerks, more active switchmen, and most active section men. Potential confounding variables were not controlled. Death caused by atherosclerosis was more frequent for clerks (relative risk 2.03) and switchmen (relative risk 1.46) when compared with the more physically active section men.
Morris and colleagues studied 667 male London bus drivers and conductors (age range 30–69 years) for five years.7 Physical activity on the job was assessed by specific work duties: drivers were sedentary whereas conductors moved about the double-decker buses collecting fares. The incidence of CHD was much lower for the more active conductors than for the drivers (age-adjusted relative risk 1.8).
Paffenbarger et al followed 6351 San Francisco longshoremen (35–74 years of age) for 22 years.8 Physical activity was defined by specific job requirements and categorized as light (1.5 –2.0kcal/min, 1.3–1.8 metabolic equivalents (METs) for a 70kg person), moderate (2.4–5.0kcal/min, 2.0–4.3METs) or heavy (5.2–7.5kcal/min, 4.4–6.4METs). Death attributable to CHD was inversely related with job energy expenditure (relative risk (RR) 1.8 for light and 1.7 for moderate, compared with heavy physical activity).
Leisure-time physical activity and exercise
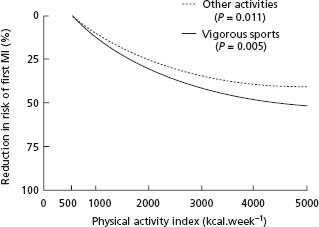
Several studies have investigated the association between the amount and intensity of leisure-time physical activity or exercise and CHD endpoints. The most prominent investigation in this group is the Harvard Alumni Study of Paffenbarger and associates.9 Beginning in 1962 and continuing until 1978, 16 936 men were followed for a variety of endpoints including first myocardial infarction (MI), cardiovascular death, and CHD death. An index of energy expenditure for physical activity and exercise in kcal/week was estimated for each subject based on self-reported physical activity, including number of blocks walked, stairs climbed, and participation in vigorous exercise. Among the findings of the study was an inverse relationship between the amount of habitual physical activity and/or exercise and first MI (age-adjusted relative risk 1.64 for men with < 2000 kcal/week versus men with >2000kcal/week). Interestingly, having participated in athletics as a young person was not associated with a lower risk unless there was evidence of current physical activity or exercise. After adjustment for age, smoking and hypertension, there remained a significant dose–response relationship. Figure 15.1 illustrates this dose–response relationship, as well as the cardioprotective advantage of vigorous exercise over less vigorous physical activity.
Figure 15.1 Exercise and physical activity and the reduction in risk of first myocardial infarction: the Harvard Alumni Study. (From Paffenbarger & Hyde9.)
In 1977, a second physical activity and exercise questionnaire was administered to the Harvard Alumni Study cohort. A subgroup of 12 516 survivors without documented CHD were followed until the end of 1993.10 After adjustment for age and multiple well-established coronary risk factors, subjects who expended more than 1000 kcal/ week experienced an approximately 20% lower coronary event rate than subjects who expended less than 1000 kcal/ week. A third questionnaire was given to 7307 Harvard Alumni Study subjects in 1988, and included questions regarding the frequency and duration of each episode of physical activity and exercise.11 Follow-up concluded at the end of 1993 and revealed that after adjustment for total energy expenditure, the duration of each episode of physical activity or exercise had no independent effect on coronary risk. As long as the total energy expenditure was similar, longer sessions of physical activity or exercise did not result in a greater risk reduction.
Morris and colleagues studied 17 944 British male civil servants, aged 40–64 years, for an average of 8.5 years.12 Baseline levels of physical activity and exercise were assessed by a unique 48-hour recall of leisure-time activities. Vigorous exercise was defined as an energy expenditure of at least 7.5 kcal/minute (6.4 METs for a 70 kg person). During follow-up, there were 1138 coronary events (fatal and non-fatal first MI). The age-adjusted relative risk of a coronary event for men reporting non-vigorous physical activity versus those reporting vigorous exercise was 2.2.
The Nurses’ Health Study enrolled 72 488 women, aged 40–65 years, who were initially free from CHD.13 Habitual patterns of physical activity and exercise, including walking, cycling, jogging, swimming, racquet sports, calisthenics, aerobics, stairs climbed, and walking pace were collected in 1986 and subsequently updated in 1988 and again in 1992. After eight years of follow-up, 645 coronary events (MI, CHD death) occurred. There was a graded, inverse relationship between amount of physical activity or exercise and coronary events. The multivariate adjusted relative risk for the most physically active versus the least physically active quintile of the population was 0.66. Walking distance was inversely associated with risk. Vigorous exercise was associated with a 30–40% reduction in coronary events. Subjects who were initially sedentary and became more active during follow-up enjoyed a lower coronary risk than sedentary subjects who remained inactive.
The Women’s Health Study included 39 372 health professionals who were at least 45 years of age and free of CHD at enrollment.14 Habitual levels of physical activity and exercise, including walking, pace of walking, flights of stairs climbed, and sporting pursuits were assessed. After an average follow-up interval of 5 years, 244 cases of CHD occurred (MI, coronary revascularization, CHD death). The multivariate adjusted relative risk for the most active (> 1500 kcal/week) versus the least active (<200kcal/week) quartiles was 0.75. The time spent walking was more important in coronary risk reduction than was the pace of walking. For women with coronary risk factors such as obesity, cigarette smoking and dyslipidemia, physical activity and exercise were protective. Subjects who walked one hour per week experienced one half of the risk of subjects who did not walk.
Cardiorespiratory fitness and coronary death
When estimated with maximal graded exercise testing, cardiorespiratory fitness has been shown to be inversely related with cardiovascular risk. The following are examples of investigations, some that included both genders as well as younger and older subjects. An important limitation of these studies is that genetic potential plays a central role in cardiorespiratory fitness, independent of habitual exercise.5
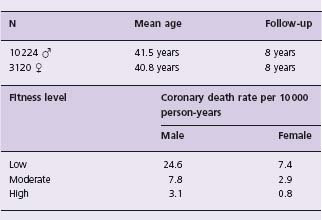
Blair and associates studied patients of the Aerobics Center in Dallas, Texas, who had an initial evaluation including a maximal treadmill exercise test. Men (n = 10 224) and women (n = 3120) were categorized by fitness level (low, moderate, high), based on treadmill exercise performance, and followed for an average of eight years.15 The coronary death rate decreased dramatically with increasing fitness level for both genders (Table 15.1). However, there were relatively few coronary deaths in this population of rather young subjects (66 deaths in men, seven deaths in women). Blair also assessed the effects of improvement in cardiorespiratory fitness on coronary risk with subjects at the Aerobics Center.16 A large cohort of men (n = 9777, age range 20–82 years) underwent two maximal treadmill exercise tests at a mean interval of 4.9 years. The subjects were followed for an average of 5.1 years. There were 87 cardiovascular deaths during follow-up. Relative to subjects who remained unfit, subjects who improved their fitness category experienced an age-adjusted relative risk of 0.48 (95% confidence interval (CI) 0.31–0.74).
Table 15.1 Rates of coronary death by fitness level: the Aerobics Center Study (from Blair et al.15)
A cohort of 1960 Norwegian men (age range 40–59 years) underwent maximal graded exercise testing and were followed for an average of 16 years.17 Eighty-seven cardiovascular deaths occurred. After extensive statistical control of potential confounding factors, a strong inverse relationship between cardiorespiratory fitness and coronary risk was found. Compared with men in the lowest fitness quartile, the relative risks for quartiles 2, 3, and 4 were 0.59, 0.45, and 0.41, respectively.
Two studies involving all residents of Olmsted County, Minnesota, who underwent maximal treadmill exercise testing in the late 1980s provide additional insight into the relationship of cardiorespiratory fitness and coronary risk. Roger and colleagues followed 1452 men and 741 women who had treadmill exercise tests in 1987 and 1988 for approximately six years.18 Cardiovascular endpoints included cardiac death, non-fatal myocardial infarction, and congestive heart failure. A total of 160 cardiovascular endpoints occurred during follow-up (106 in men, 54 in women). After multivariate adjustment, peak treadmill workload in METs was the only variable associated with the outcome measures. For each 1 MET increment in cardiorespiratory fitness, cardiac events were reduced by 25%, with a similar effect for both genders. Using similar methods, Goraya and associates followed 3107 Olmsted County residents who underwent maximal treadmill exercise testing in 1987 to 1989 and were followed for a median of six years.19 Both genders were included and 514 of the subjects were over 65 years of age. For each 1 MET increase in cardiorespiratory fitness, cardiovascular events were reduced by 14% and 18% for younger and older (>65 years) subjects, respectively.
Exercise training in established coronary disease
For patients with coronary heart disease, exercise training improves exercise capacity and symptoms. After three months of aerobic exercise training, peak oxygen uptake improves by 15–20%.20 Symptoms of angina pectoris may be markedly improved by exercise training. Resistance training results in improvements in muscle strength and maintains muscle mass. There are also data available to demonstrate that physical activity and exercise training improve important clinical outcomes for patients with coronary heart disease. These data are the result of both observational and randomized controlled trials.
Observational data
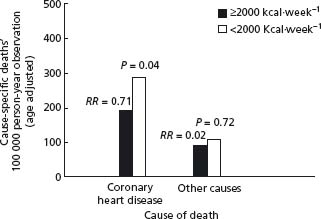
In the Harvard Alumni Study, reviewed previously in this chapter, a subset of 782 subjects of the entire 16 936-person cohort had documented coronary heart disease at the beginning of the study.9 Over a follow-up interval of approximately 12 years, the more physically active subjects (those who expended more than 2000 kcal/week in leisure-time physical activity and exercise) experienced a 30% lower coronary event rate than less active subjects (Fig. 15.2). The beneficial effect of exercise persisted after statistical adjustment for smoking, blood pressure, body weight, family history of coronary heart disease and age.
Figure 15.2 Physical activity and death rates in patients with coronary artery disease in the Harvard Alumni Study. (From Paffenbarger & Hyde9.)
In the British Regional Heart Study, 772 of the 5934 men in the cohort had documented coronary heart disease at the onset of the trial.21 A baseline assessment of habitual physical activity, including intensity of activity, was performed. After five years of follow-up, 131 deaths had occurred (94 from cardiovascular disease). Compared with inactive subjects, persons who performed light, moderate or vigorous exercise experienced a substantially lower all-cause and cardiovascular mortality (Table 15.2). These results were similar for younger and older (> 65 years of age) subjects.
Table 15.2 Cardiovascular mortality by activity level in the British Regional Heart Study (from Wannamethee et al.21)
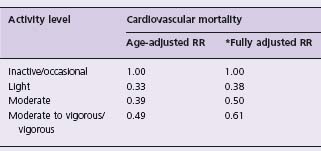
* Adjusted for age, smoking, social class, self-rated health status, diabetes, and history of myocardial infarction and stroke.
Randomized trials
Kallio and colleagues randomized 301 men and 74 women with a history of myocardial infarction to a comprehensive rehabilitation program (exercise training, dietary and smoking cessation advice, psychosocial counseling) or to a control group.22 Compared with the control group, the intervention group experienced an improvement in habitual physical activity, blood lipids and blood pressure. The three-year cumulative mortality was 18.6% in the intervention group versus 29.4% in the control group (P = 0.02). The difference was primarily the result of a reduction in the incidence of sudden cardiac death in the intervention group (5.8% versus 14.4%, P < 0.01). The rate of non-fatal reinfarction was similar for both groups.
Hamalainen and associates reported 10-year follow-up data for the same subjects.23 No organized intervention occurred after the first three years of the study. At 10 years, the incidence of sudden cardiac death was less for the intervention group (12.8% versus 23.0%, P = 0.01). Cardiac mortality was also lower for intervention subjects (35.1% versus 47.1%, P = 0.02). The largest difference in mortality was observed during the first year of the investigation when beta-blocker use was similar for both groups.
Hambrecht et al
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


