Peripheral Vascular Disease with Claudication (Open Femoral Popliteal Bypass)
SUKGU M. HAN and CHRISTOPHER D. OWENS
Presentation
A 65-year-old male with a history of diabetes mellitus, hypertension, and a 30-pack-year history of smoking presents with pain in his left leg with walking. The patient describes the pain as dull aches, localized to the calf, and relieved with rest. He denies pain at rest or ulcers on his legs or feet. The pain started 8 months ago and has progressed in severity. During this time, walking distance at which the calf pain starts has progressively decreased to less than one block. On physical exam, he has normal bilateral femoral pulses, and faintly palpable right popliteal, dorsalis pedis, and posterior tibial pulses. On the left, pulses at the popliteal artery and below are absent. Only faint monophasic Doppler signals are detectable at his feet.
Differential Diagnosis
This patient presents with a classic description of lower extremity claudication from peripheral vascular disease (PVD): pain in the calf, reproducibly provoked by walking, and relieved with rest. Patients with claudication typically describe a sense of heaviness, weakness, or fatigue accompanying the pain. Occasionally, the exact cause of lower extremity pain becomes difficult to determine in patients with PVD, who also have neuropathy or radiculopathy from concomitant diabetes and spinal stenosis, respectively. Neuropathic pain is often described as a sharp, shooting, or burning sensation, while radiculopathy is worsened with prolonged sitting and is associated with particular position.
Workup
This patient’s history and physical examination suggest arterial insufficiency as the most likely cause of his leg pain. Physical examination does not reveal lower back pain, or any maneuvers that elicit pain, which makes radiculopathy associated with spinal stenosis a less likely etiology.
The patient undergoes bilateral lower extremity arterial duplex ultrasound. His ankle-brachial indices (ABIs) are 0.9 and 0.75 on right and left, respectively. Noninvasive vascular laboratory studies allow dynamic quantitative assessment of lower extremity perfusion. Normal ABIs are greater than 1.0, while values less than 0.9 often correlate with claudication, and less than 0.7 with critical limb ischemia. In patients with long-standing diabetes mellitus or renal failure, where medial calcific sclerosis may be present in pedal arteries, their ABI values can be falsely elevated due to noncompressible vessels. In these instances, toe-brachial index (TBI) or percutaneous oxygen tension (tcPO2) is used as a more reliable indicator of leg perfusion. In cases where claudication is strongly suspected with normal resting ABIs, exercise can induce a drop in ABIs by increasing flow across a given lesion. The abnormal ABIs in the setting of this patient’s vascular examination suggest PVD as the most likely cause of pain. In addition to ABIs, duplex ultrasound can further characterize the stenosis by directly visualizing the plaque on gray-scale B-mode image and assessing the pulse wave form across the lesion on color-flow Doppler mode (Fig. 1). The degree of stenosis can be quantified by the elevation of peak systolic velocity (PSV) and broadening of the velocity waveforms across the lesion in the arterial segment. Typically, doubling of PSV compared to adjacent nondiseased arterial segment or PSV above 200 cm/s corresponds to greater than 50% luminal stenosis. Reconstituted arterial flow downstream to a complete occlusion shows blunted, monophasic waveforms with low PSV.
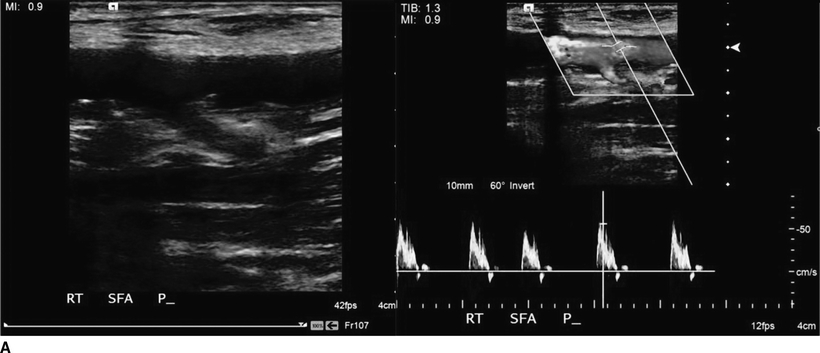

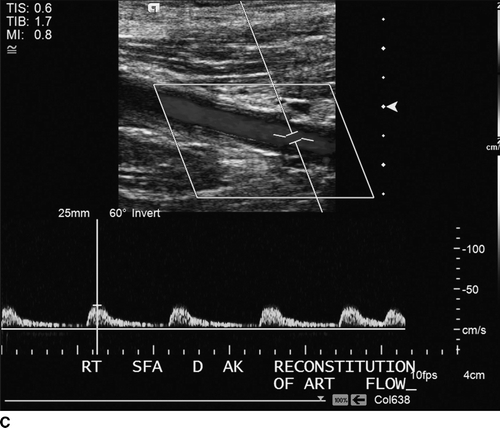
FIGURE 1 A: Proximal superficial femoral artery with non–flow-limiting stenosis with normal pulse wave form. B: Complete occlusion of mid SFA. C: Monophasic flow seen in the distal SFA.
Anatomical evaluation of this patient’s disease is traditionally done by angiography, with arterial access obtained typically at the contralateral groin. This patient’s angiography (Fig. 2) shows chronic total occlusion of the superficial femoral artery with extensive collateral circulation arising from the profunda femoris reconstituting the popliteal artery below the knee. The popliteal artery gives branches to anterior and posterior tibial arteries. Some centers utilize CT angiogram (CTA) as the initial imaging study of choice. While CTA has the advantage of not requiring an arterial puncture, a detailed evaluation of infrapopliteal lesions is limited due to artifacts from calcification. In addition, formal angiography allows one to treat the lesion with balloon angioplasty or stenting in the same setting when appropriate.

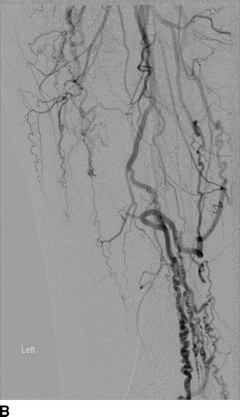

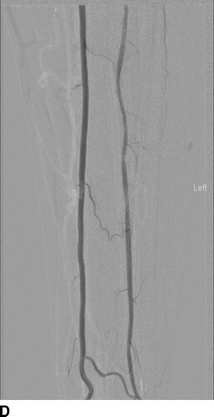
FIGURE 2 A: Femoral angiography showing undiseased profunda femoris and heavily calcified superficial femoral artery with occlusion at the mid-thigh. B: Angiography of the left thigh showing extensive collateralization from branches of the profundafemoris. C: Angiography of the left knee, showing reconstitution of the above-knee popliteal artery. D: Angiography of the left calf showing patent anterior and posterior tibial arteries supplying the foot.



