Chapter 11 Pericardial, Myocardial, and Pulmonary Syndromes
A wide variety of major disease processes may affect the ECG. Particularly important are conditions affecting the pericardium (acute pericarditis, pericardial effusion, and chronic constrictive pericarditis), the myocardium itself (not including ischemia and infarction, which are discussed in Chapters 8 and 9), and the lungs (acute pulmonary embolism and chronic obstructive pulmonary disease).
Acute Pericarditis, Pericardial Effusion, and Chronic Constrictive Pericarditis
Acute Pericarditis
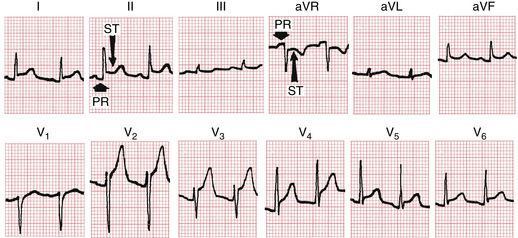
As mentioned in Chapter 8, the ECG patterns of pericarditis resemble those seen with acute MI. The early phase of acute pericarditis is usually characterized by ST segment elevations. This type of current of injury pattern results from inflammation of the heart’s surface (epicardium), which often accompanies inflammation of the overlying pericardium (Fig. 11-1).
A major difference between these elevations and the ones occurring with acute MI is their distribution. The ST segment elevations with acute MI are characteristically limited to the anterior or inferior leads because of the localized area of the infarct. The pericardium envelops the heart, and the ST-T changes occurring with pericarditis are therefore usually more generalized. ST segment elevations are typically seen in both anterior and inferior leads. For example, in Figure 11-1 notice the elevations in leads I, II, aVL, aVF, and V2 to V6.
Not only does acute pericarditis affect ventricular repolarization (the ST segment), it also affects repolarization of the atria, which starts during the PR segment (the end of the P wave to the beginning of the QRS complex) (see Fig. 11-1). In particular, pericardial inflammation often causes an atrial current of injury, reflected by elevation of the PR segment in lead aVR and depression of the PR segment in other extremity leads and the left chest leads (V5 and V6).
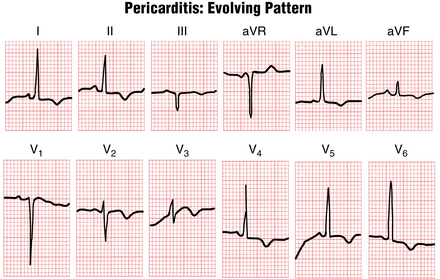
The ST segment elevations seen with acute pericarditis are sometimes followed (after a variable time) by T wave inversions (Fig. 11-2). This sequence of elevations and inversions is the same as that described for MI. In some cases the T wave inversions caused by pericarditis resolve completely with time and the ECG returns to normal. In other cases the T wave inversions persist for long periods.
The similarity between the ECG patterns of acute pericarditis and acute MI has been emphasized because both conditions may produce ST segment elevations followed by T wave inversions. As noted, however, the ST-T changes with pericarditis tend to be more diffuse than the localized changes of MI. Another major difference is that pericarditis does not produce abnormal Q waves, such as those seen with certain infarcts. With MI, abnormal Q waves occur because of the death of heart muscle and the consequent loss of positive depolarization voltages (see Chapter 8). Pericarditis, on the other hand, generally causes only a superficial inflammation and does not produce actual myocardial necrosis. Thus, abnormal Q waves never result from pericarditis alone.
Pericardial Effusion
Pericardial effusion refers to an abnormal accumulation of fluid in the pericardial sac. In most cases this fluid accumulates as the result of pericarditis. In some cases, however, such as myxedema (hypothyroidism) or rupture of the heart, pericardial effusion may occur in the absence of pericarditis. The major clinical significance of pericardial effusion is the danger of cardiac tamponade, in which the fluid actually “chokes off” the heart, leading to a drop in blood pressure and sometimes to cardiac arrest with pulseless electrical activity (see Chapter 19).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree