Percutaneous Mitral Valve Repair
D. Scott Lim
Gorav Ailawadi
INTRODUCTION
As the preceding decades have witnessed the maturity of surgical therapies for valve and coronary artery disease, the next decade will witness a tremendous change in our approach to percutaneous therapies for heart valve disease. Recently, we have seen a remarkably explosive growth of percutaneously implanted heart valves in Europe, and a myriad of novel devices being developed for repair or replacement of diseased heart valves from a transcatheter approach. This chapter will focus on novel percutaneous options for repair of mitral valve regurgitation.
PERSPECTIVE ON MITRAL REGURGITATION
Mitral regurgitation (MR), from nonrheumatic etiology, may be due to either degenerative valve disease, such as prolapse, chordal rupture, or myxomatous degeneration, or functional etiologies such as ischemic cardiomyopathy and secondary MR. Additionally, as transcatheter therapies focus on functional etiologies of MR, our knowledge base of how the disease of the ventricle affects the mitral apparatus. Significant MR (3 or 4+) occurs in 0.5% of the population, with approximately 250,000 new cases annually in the United States. For patients with significant MR, medical therapy has been shown to be ineffective in treating the underlying pathophysiology and is unable to retard disease progression. Surgical repair or replacement is the standard of care, as it is efficacious and low risk. However, it has been estimated that only ˜20% of patients with significant MR undergo surgery. Therefore, there is a significant unmet therapeutic need for patients with mitral valve regurgitation, and particularly for patients at high surgical risk, a significant opportunity for novel catheterbased therapies.
HISTORICAL PERSPECTIVE ON PERCUTANEOUS THERAPIES FOR MITRAL VALVE DISEASE
The very first percutaneous therapy for mitral valve disease was the balloon mitral commissurotomy for rheumatic mitral stenosis. Since then, the technique has matured with the use of specific shaped balloons, and a better understanding of the types of rheumatic valve disease amenable to this therapy, as well as the long-term outcomes from this percutaneous approach. However, it is also important to note that the skills and techniques involved with this procedure are complex and involve a transseptal puncture, which is not commonly performed by most physicians trained today (Fig. 45.1).
Adapted from a Surgical Approach to Mitral Regurgitation
Currently, surgery for MR has become a mature therapy, with a wide range of different techniques involving leaflet, chordal, and annular approaches. Concepts behind each of these approaches have been utilized by novel transcatheter approaches to repair of MR. Additionally, work continues to create a transcatheter replacement option for mitral valve disease.
Indirect Annular Approaches to Mitral Regurgitation Therapy
The concept of a percutaneous annular approach mimics the surgical concepts of annular diameter reduction and bringing the posterior part of the annulus anteriorly, thereby pushing the posterior leaflet forward to create a better coaptation with the anterior leaflet.
While later percutaneous devices have focused on direct approaches to the annulus, early designs have attempted to follow the course of the coronary sinus. However, they have been limited by the anatomic fact that the coronary sinus does not run in the same plane as the mitral annulus, as well as the incidence of circumflex artery crossing the coronary sinus.
The coronary sinus devices were introduced from a percutaneous, transjugular approach. One of the first such devices tested was the Edwards Lifesciences MONARC system—it was implanted in the coronary sinus with distal and proximal self-expanding stent anchors, and had a variable length connecting bridge. The connecting bridge had dissolvable polymers that would foreshorten over a period of weeks, changing the radius of curvature of the coronary sinus and bringing the posterior portion more anterior. It was studied in 72 patients—mainly with moderate degrees of MR, but with limited efficacy (able to be implanted in 82%, and a sustained reduction of mitral regurgitaiton by 1 grade in ˜40%) and an incidence of complications of 28% at 2 years. Likely due to the inability to study the affects and risks of this device acutely, further study on this device was stopped.
Other coronary sinus devices such as Cardiac Dimensions’ Carillon device has had more success. It too is implanted with proximal and distal coronary sinus anchors, but with acutely observable affects on MR and is retrievable if needed due to inadequate efficacy or complication. It was studied in the European AMADEUS and TITAN trials in small numbers of patients also with mainly moderate degrees of functional MR. It was able to be implanted in ˜66% of intended patients, and an ultimately low incidence of complications (˜13% in the early AMADEUS trial and decreasing to ˜2% in the later TITAN trial). Its efficacy was limited (˜1 grade improvement in indices of MR) but promising in the appropriately selected patients. It has recently been awarded regulatory approval in Europe.
Similarly, Viacor’s PTMA coronary sinus device was studied in the PTOLEMY 1&2 trials, demonstrating in a small number of
patients low adverse events and an average of 1 grade MR reduction. It remains at present in early clinical study.
patients low adverse events and an average of 1 grade MR reduction. It remains at present in early clinical study.
Direct Annular approaches to Mitral Regurgitation Therapy
Other percutaneous therapies have utilized sutures to plicate or wires to cinch the annulus directly, with catheters coming at the annulus from both the left atrium and left ventricle. However, these therapies remain in early research stages. A potentially promising approach uses radiofrequency energy to cause scarring and contraction of the collagen in the annulus. While this technology has remained in relatively early preclinical trials, it holds promise in that no hardware is implanted and the therapy may be applied to the annulus repeatedly.
Leaflet Approaches
One approach, which ultimately matured into a catheter-based therapy, is the edge-to-edge approach as described by Alfieri’s group. In this surgical leaflet therapy, the central edges of the anterior and posterior leaflets are anastomosed creating a doubleorifice mitral inflow. The concepts of this edge-to-edge approach were used by both the Edwards Lifescience’s Mobius device and Abbott Vascular’s MitraClip to create some of the first novel catheter-based therapies for MR. The Mobius device utilized a 17F delivery system from a percutaneous, transvenous, and transseptal approach. Its therapy catheter contained a vacuum port which was used to grab the leaflets, through which it would then throw a stitch, secured with a nitinol clip, mimicing the Alfieri edge-to-edge approach. This device was evaluated in the Milano II trial, which demonstrated limited efficacy both acutely and at 30 days, ultimately leading to its abandonment.
The MitraClip’s early design iterations attempted to duplicate this same suturebased approach to leaflet apposition, and involved using hollow needles to pierce the central portions of the anterior and posterior leaflets to deliver pledgeted sutures (Fig. 45.2). This technique worked on the open, nonbeating heart but it was soon realized that an independent mechanism to grasp the leaflets while they were in motion was needed to be incorporated into the design concept.
MITRACLIP SYSTEM
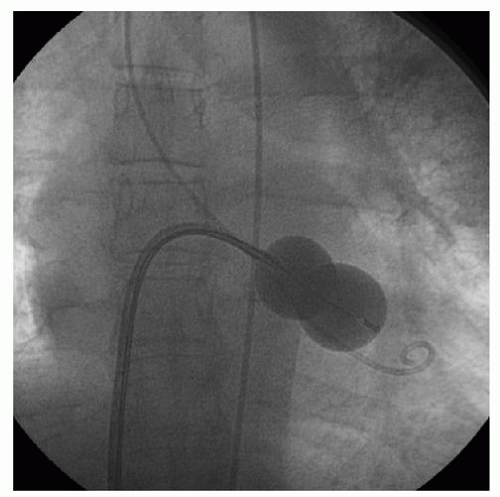
This novel percutaneous approach was the first achieving success in prehuman and clinical trials for treatment of patients with nonrheumatic MR. The concept of leaflet grasping by a clip mechanism on the regurgitant portions of the mitral valve became the hallmark of the final design freeze of the MitraClip (Fig. 45.3; Abbott Vascular, Santa Clara, CA). The MitraClip is introduced from a percutaneous, transvenous, and transseptal approach to the mitral valve (Fig. 45.4). The traditional imaging modality in the catheterization laboratory of fluoroscopy is of limited utility in this procedure, as it cannot visualize the mitral leaflets. Therefore, the procedure is guided by simultaneous transesophageal imaging, ideally using both two- and three-dimensional echocardiography (see Figs. 45.5 and 45.6




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree