PATENT DUCTUS ARTERIOSUS
The ductus arteriosus is a normal fetal cardiac structure that connects the pulmonary artery to the descending aorta. Normally, the ductus arteriosus develops embryologically from the distal left sixth arch. It functionally closes within the first day of life. However, it may remain patent either in isolation or in association with other congenital cardiac malformations. In premature infants, continued patency of the ductus arteriosus is common after birth and closure is dependent on maturation. The clinical significance of a patent ductus arteriosus (PDA) is determined by the magnitude and direction of shunting across it. Echocardiography is useful in defining the morphologic features of the PDA, the shunt flow dynamics across it, and its hemodynamic effects on the heart.
Two-Dimensional Echocardiography
As an isolated lesion, a PDA is seen as a tubular structure connecting the superior junction of the main pulmonary artery and left pulmonary artery to the ventral aspect of the proximal descending aorta just beyond the origin of left subclavian artery. A PDA can be best visualized from the parasternal short-axis, high-left parasternal short-axis, and suprasternal long-axis views.
In the parasternal short-axis view, the PDA is seen arising from the main pulmonary artery and connecting to the descending aorta. Angulating the transducer superiorly and leftward toward the pulmonary artery bifurcation provides images of the PDA (Fig. 19.1, Video 19.1). A dropout between the main pulmonary artery and the descending aorta may occur in standard parasternal short-axis views. For optimal imaging of the PDA, avoiding any foreshortening or dropout, a high-parasternal view, also called the “ductal view,” is used. To obtain this view, the transducer is positioned between the suprasternal notch and the standard parasternal region in the left infraclavicular region. The plane of transducer is directed similar to the suprasternal long-axis views through the left pulmonary artery. In this view, the PDA can be seen between the origin of left pulmonary artery and the descending aorta (Fig. 19.2, Video 19.2). With slight rotation of the transducer to obtain the long-axis view of the aorta, the entire length of the PDA can be visualized. However, a small PDA may not be apparent in this view as it is positioned vertically within the scan plane and therefore imaged with the lateral resolution of the transducer. If the ductus is right-sided, similar views can be obtained by scanning from a right parasternal approach.
In the suprasternal long-axis views, a PDA is seen connecting the main pulmonary artery and the descending aorta, beyond the origin of the left subclavian artery. In this view, better imaging of the PDA can be obtained by tilting the imaging plane anteriorly toward the left pulmonary artery. The PDA is seen in this view, between the origin of the left pulmonary artery and the descending aorta (Video 19.3).
Direct visualization of a PDA in the parasternal long-axis view is difficult. The transducer is angled leftward and superiorly toward the right ventricular outflow tract and main pulmonary artery, and the color flow from the PDA toward the transducer can be seen from a left-to-right shunt across the PDA.

Figure 19.1. Parasternal short-axis view of the patent ductus arteriosus (PDA) (arrow) connection between the main pulmonary artery (MPA) and descending aorta (DAo). Ao, aorta; LA, left atrium; RV, right ventricle.
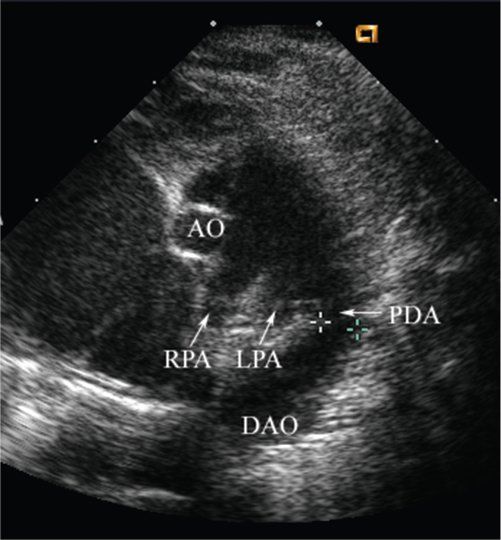
Figure 19.2. A high-left parasternal short-axis view (ductal view) of a large patent ductus arteriosus (PDA) between the origin of left pulmonary artery (LPA) and descending aorta (DAo), in a patient with hypoplastic left heart syndrome. In this view, the right pulmonary artery (RPA), left pulmonary artery, and PDA (arrows) are demonstrated from right to left of the image. Notice the small aorta (Ao).
Morphologic Variations in Patent Ductus Arteriosus
A PDA with a left aortic arch connects the aortic isthmus with the proximal left pulmonary artery. A PDA with a right aortic arch can be either right-sided (between the descending aorta and the right pulmonary artery), left-sided (between the innominate artery or left subclavian artery and the left pulmonary artery), or bilateral. To image the PDA arising from the base of innominate artery, the transducer is rotated from the suprasternal or high-parasternal view into a frontal plane such that the aorta is seen in its short axis and the right pulmonary artery is seen in its long axis. From this position, the innominate artery can be visualized by angulating the transducer toward the right or left depending on the side of the aortic arch. The bifurcation of the innominate artery into the subclavian and carotid arteries along with the origin of the PDA at its base can be seen in this view. In the rare instance when there are bilateral PDAs, one ductus is seen in the usual position and the other may arise from the base of either the subclavian artery or the innominate artery on the contralateral side (Video 19.4). The PDA in a normal heart runs in an oblique course, forming an obtuse angle with the descending aorta. This normal course of a PDA is altered in congenital heart diseases associated with right ventricular outflow tract obstruction, such as tetralogy of Fallot and pulmonary atresia. In these cases, the PDA has a nearly vertical orientation between distal aortic arch and the pulmonary artery and therefore is at an acute angle to the descending aorta and is often referred to as a reverse-oriented ductus. Such PDAs are often long and tortuous (Fig. 19.3, Video 19.5) and may be difficult to visualize in a single imaging plane. In hypoplastic left heart syndrome as well as with an interrupted aortic arch, the PDA is almost always large when imaged soon after birth and is at an obtuse angle to the descending aorta (Video 19.6). In the presence of an interrupted aortic arch, one should remember that the true aortic arch is superior to the continuum formed by the pulmonary artery, the PDA, and the descending aorta.
Hemodynamic Consequences of a Patent Ductus Arteriosus
The hemodynamic consequence of a large left-to-right shunt across a PDA is volume overload of the left heart and hence dilatation of the left atrium and left ventricle. Historically, the left atrium–to–aortic root (LA/Ao) ratio on M-mode examination has been used for indirect quantification of PDA size. This ratio was popular before the introduction of two-dimensional and Doppler echocardiography. The LA/Ao ratio has been reported to be greater than 1.15 (mean, 1.38 ± 0.19) in neonates with a large left-to-right shunt across a PDA, requiring surgical ligation. This M-mode assessment is obtained from the parasternal short-axis view measuring the anterior-posterior dimensions of the left atrium. Using this single dimension, measurement of the left atrium may result in inaccurate estimation of the left atrial size. If the LA/Ao ratio is used in isolation, it has a low specificity for diagnosing a significant-sized PDA. Thus, the usefulness of this ratio has decreased with the advent of two-dimensional and Doppler echocardiography, where one not only can assess the size and flow across the PDA but also can determine left heart enlargement through direct visualization. In addition to the finding of a dilated left atrium and left ventricle, the atrial septum can be seen bulging toward the right atrium. The left ventricular systolic function is often hyperdynamic. In the subcostal views, increased pulsatility of the descending aorta can be seen as a result of large diastolic runoff to the pulmonary arteries resulting in a widened pulse pressure.

Figure 19.3. Suprasternal long-axis view of the aortic arch of a tortuous patent ductus arteriosus (PDA) in a patient with pulmonary atresia. AAo, ascending aorta.
Doppler Examination
Color Doppler echocardiography provides information regarding the direction and amount of shunt flow across a PDA. Color Doppler has markedly improved the ability of echocardiography to identify a PDA, especially if it is small. Color Doppler also guides optimal alignment of the spectral Doppler beam. In addition, spectral Doppler interrogation of the PDA provides useful information regarding the shunt direction and pressure gradients throughout the cardiac cycle.
With an isolated large PDA with normal pulmonary artery pressure and a large left-to-right shunt, continuous red flow from the aorta into the pulmonary arteries will be seen with color Doppler (Fig. 19.4, Videos 19.1 and 19.7). A small isolated PDA with normal pulmonary artery pressure will have a high-velocity turbulent jet across it extending to the lateral wall of the pulmonary artery with a color mosaic caused by aliasing (Fig. 19.5). A pulsed Doppler signal of the main pulmonary artery close to the pulmonary valve shows that the systolic part of the left-to-right ductal shunt is directed away from the sample volume by the dominant forward flow across the pulmonary valve. However, during diastole as the pulmonary valve is closed, the left-to-right signal from ductal shunt is seen above the baseline. A pulsed Doppler signal of the mid-portion of main pulmonary artery may show antegrade diastolic flow below the baseline as the jet of a PDA strikes the closed pulmonary valve and deflects back along the medial wall of pulmonary artery (Fig 19.6). When the ductus is very large, the left-to-right shunt across it may completely fill the pulmonary artery, resulting in loss of secondary flow patterns in the pulmonary artery as described above. A variety of other conditions can produce diastolic flow in the pulmonary arteries that can be confused with a PDA. These include pulmonary insufficiency, a coronary fistula, anomalous origin of coronary artery from pulmonary artery, an aortopulmonary window, and surgically created systemic–to–pulmonary artery shunts.
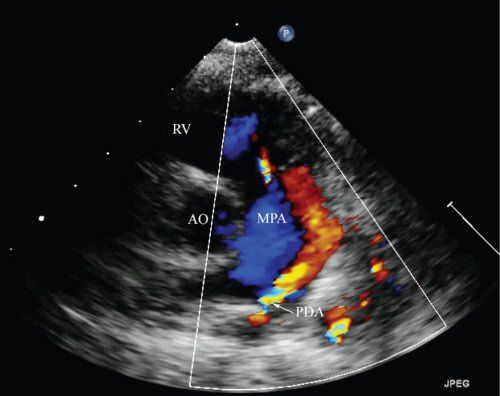
Figure 19.4. Parasternal short-axis view with color Doppler showing continuous flow (red) from the patent ductus arteriosus (PDA) into the main pulmonary artery (MPA). Ao, aorta; RV, right ventricle.
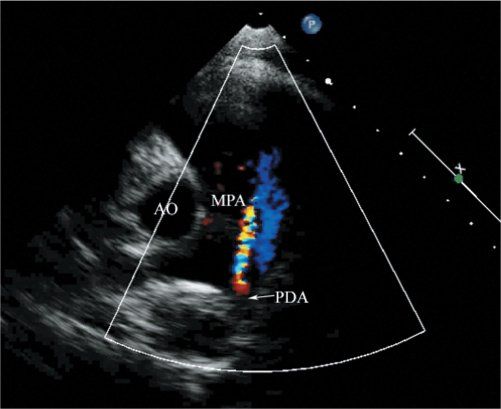
Figure 19.5. Color Doppler imaging in the parasternal short-axis view showing a high-velocity, turbulent jet across a small patent ductus arteriosus (PDA) into the main pulmonary artery (MPA) in a patient with normal pulmonary artery pressure. This high-velocity Doppler flow is indicative of a large pressure gradient between the aorta and the pulmonary artery. Ao, aorta.
Spectral Doppler interrogation of a restrictive PDA with left-to-right flow and normal pulmonary artery pressure will demonstrate continuous flow above the Doppler baseline with a peak in late systole (Fig. 19.7). Spectral Doppler of a large PDA with an unrestricted left-to-right shunt will have a pulsatile flow pattern with the highest velocity at end-systole and a very low peak velocity at end-diastole. This is because the relative pulmonary and aortic pressures are equal at end-diastole in large PDAs (Fig 19.8).
Using the modified Bernoulli equation, one can calculate the peak gradient across the PDA using the late systolic peak velocity. This measurement has been shown to closely correlate with the peak instantaneous gradient between the aorta and pulmonary artery at catheterization. If the systemic arterial systolic blood pressure is obtained simultaneous to Doppler interrogation across the PDA, one can derive the pulmonary artery systolic pressure by subtracting the peak gradient across the PDA from the systolic blood pressure. In assessing peak Doppler velocities across a PDA to obtain pressure gradients, it is important to remember that for a left-to-right shunt the sample volume should be positioned at the pulmonary end of the PDA. Conversely, for a right-to-left shunt, the sample volume should be positioned at the aortic end of the PDA. Doppler estimation of pulmonary artery pressure using the PDA velocity may not always be accurate and can be limited by the position of the sample volume, interference from signals from adjacent structures such as the left pulmonary artery, and the unusual shape, tortuosity, and size of the PDA.

Figure 19.6. Continuous-wave Doppler of the main pulmonary artery. A continuous antegrade flow during diastole is seen as the jet of the patent ductus arteriosus deflects back from the closed pulmonary valve into the main pulmonary artery.
In the presence of severe pulmonary hypertension or in congenital cardiac malformations in which the systemic circulation is dependent on the PDA (i.e., critical aortic stenosis, critical coarctation, hypoplastic left heart syndrome, and interrupted aortic arch), there is a right-to-left shunt across the PDA. Color Doppler will demonstrate blue color flow in the PDA representing blood flow from the pulmonary artery into the descending aorta (Video 19.8). A spectral Doppler interrogation of such a PDA shows continuous flow below the Doppler baseline with a peak Doppler velocity in early systole.
In normal neonates, a bidirectional shunt across the PDA is present for the first few hours of life but rapidly changes to a continuous left-to-right shunt before functional closure. In pulmonary hypertension, a bidirectional shunt is present across the PDA. Color Doppler demonstrates a right-to-left shunt in systole (blue color flow) and a left-to-right shunt in diastole (red color flow) (Video 19.9). On spectral Doppler, a negative deflection arising from the right-to-left shunt signifies flow from the pulmonary artery to aorta in mid-to-late systole, whereas a positive deflection arising from left-to-right shunt represents flow from the aorta to pulmonary artery in late systole with extension into late diastole (Fig. 19.9). One should be cautious to differentiate the negative deflection from a right-to-left ductal shunt from a negative deflection caused by flow within the left pulmonary artery. Spectral Doppler from the left pulmonary artery begins at the onset of systole and peaks early, while the right-to-left shunt across a PDA begins later in systole and peaks in mid to late systole.
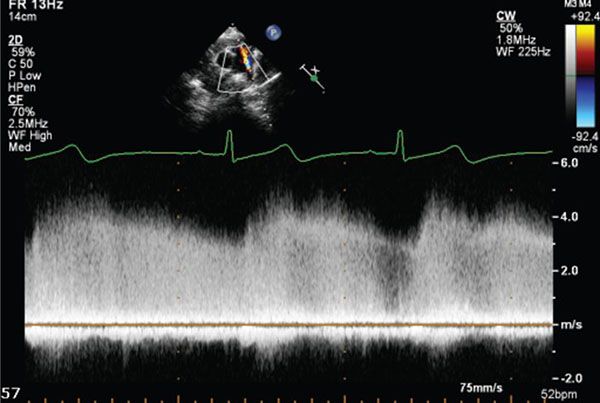
Figure 19.7. Continuous-wave Doppler tracing obtained from the parasternal short-axis view in a patient with a small patent ductus arteriosus (PDA) and normal pulmonary artery pressure. There is continuous left-to-right shunting across the PDA in systole and diastole, with a peak Doppler velocity obtained in late systole. The high-velocity of the jet (4 m/s) across the PDA indicates normal pulmonary artery pressure.

Figure 19.8. Doppler of a large PDA with an unrestricted left-to-right shunt. The highest velocity is noted at end-systole with a very low peak velocity at end-diastole due to nearly equal pulmonary and aortic pressures at end-diastole in large PDAs.
Pulsed-wave Doppler allows assessment of flow disturbances on either side of the PDA. In a PDA with large left-to-right shunt, there is increased diastolic forward flow in the left pulmonary artery and retrograde diastolic flow in the postductal descending aorta. These retrograde diastolic flow signals are M-shaped, with peaks in early diastole and with atrial systole (Fig. 19.10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


