Fig. 22.2 Twenty-four hour ECG, in a patient with brief bursts of regular palpitations. Initially sinus rhythm, then a fast regular narrow complex tachycardia, with ST segment depression, becoming more pronounced over the next 30–40 beats. A few beats into the arrhythmia there is a bold line, the patient activated marker, confirming when symptoms occur. This ECG looks like atrioventricular nodal re-entrant tachycardia (AVNRT).
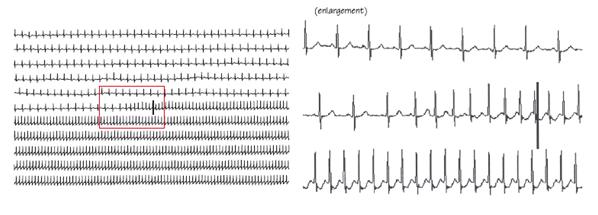
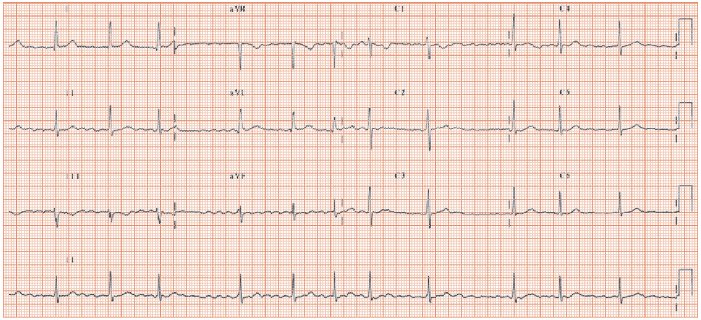
Fig. 22.3 This patient had infrequent prolonged irregular palpitations. ECG recorded during an attack. Atrial fibrillation (AF) – no discernible P wave, irregular baseline, especially in lead II, fine fibrillatory f waves, and an irregular QRS response. Well-controlled QRS rate of 75 b/min; unusual, as most patients have a high heart rate at AF onset, around 120–150 b/min. A lower heart rate suggests: (i) atrial fibrillation has been present longer than realised; (ii) underlying atrioventricular (AV) conduction disease; (iii) the patient is taking drugs to slow AV conduction; or (iv) high vagal tone, e.g. physical fitness. The underling QRST complexes are normal.
Palpitations are an abnormal appreciation of the heartbeat. The key to diagnosis is to obtain an ECG during an attack; which method is best depends on the frequency and duration of the symptoms (Table 22.1). The history provides a reasonable diagnostic guide:
- Appreciation of the normal heartbeat (e.g. almost always relating to emotional stress, rarely relating to thyrotoxicosis, and very rarely to phaeochromocytoma). Palpitations in this situation have a slow onset/offset over many minutes, ill-defined duration, usually last many hours, and have no response to vagotonic manoeuvres (Valsalva, neck pressure, cold drinks). They usually occur in the context of emotional stress.
- Arrhythmia. Palpitations due to arryhythmias usually are of sudden (instantaneous) onset, sudden/slow offset, duration well-defined and remembered by the patient, and they may have identified a response to vagotonic manoeuvres. Patients may have noticed post-event polyuria, although this is a relatively rare phenomenon. Bradyarrhythmias do not cause palpitations, tachycardias can:
- Ventricular extrasystoles (VEs) cause brief symptoms (lasting only a few seconds’) from the:
Symptoms are commoner at slow heart rates, e.g. at night time. This is because some extrasystoles are more likely to occur when the cardiac action potential is prolonged. This occurs with low heart rates, and when vagal tone is high, conditions both found at night (Chapter 17). Atrial extrasystoles cause fewer symptoms than VEs (Fig. 22.1).
- Re-entrant supraventricular tachycardia (SVT) (atrioventricular re-entrant tachycardia [AVRT] and atrioventricular nodal re-entrant tachycardia [AVNRT]) give rise to sudden onset fast (patients taps out a heart rate of 150–200 b/min) regular palpitations, of well-defined duration, usually (not always) with symptoms stopping as suddenly as the arrhythmia does. Symptoms other than palpitations are rare, unless there is associated heart disease (e.g. coronary disease, left ventricular dysfunction, etc.). Associated heart disease is relatively rare, as the common age of presentation for many SVTs is 20–50, whereas most structural heart disease occurs in an older age group.
- Atrial fibrillation (AF) results in sudden onset fast palpitations, differentiated from re-entrant SVTs by their irregularity (‘all over the place’) and from VEs by the heart rate (fast in AF, normal in VES). Atrial fibrillation is associated with structural heart disease, so breathlessness and (rarely) angina may occur. Atrial fibrillation terminates abruptly, so symptoms usually stop suddenly. Many reentrant tachyarrhythmias (e.g. AVNRT or AVRT) last only a number of minutes, only relatively rarely lasting many hours, whereas AF, while it certainly can last only a number of minutes, not infrequently lasts many hours or even days. Occasionally sinus disease underlies AF. If so, when AF terminates the sinus node takes 3–5 s to restart, when sinus arrest occurs and cardiac output ceases, some patients may feel faint or actually blackout.
- Ventricular tachycardia (VT) gives rise to three distinct syndromes: (i) sudden onset fast regular palpitations, ± near blackouts; (ii) blackouts, which maybe preceded by fast regular palpitations; (iii) sudden cardiac death, when VT degenerates to ventricular fibrillation. The clue to VT being the diagnosis is knowing or finding structural heart disease, or finding an abnormal inter-attack ECG. Though most such ECGs show obvious abnormalities, be aware that there are a few conditions where the ECG signs can be quite subtle, and these include right ventricular cardiomyopathy (where subtle repolarization changes in leads V1 to 3 may occur, though this is not a universal finding at all), and Brugada syndrome (whose ECG appearance can come and go).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


