Chapter 37 Pacemaker Follow-up
Introduction
Since the implantation of the first human pacemaker in 1958, electrical myocardial stimulation against various types of rhythm disorders of the heart has become available. Pacemakers were initially introduced for the treatment of heart block and later on for sinus node disease. Currently, they are used for a variety of conditions, including tri-fascicular block and syncope related to a variety of pathologic reflexes. This implies that pacemakers now have an important role as lifesaving devices.1 They are important tools for improving quality of life in several of the cited conditions; thus pacemaker therapy has become one of the most effective medical treatments. The recent innovation of cardiac resynchronization added another dimension to pacing because combined left and right ventricular stimulation is a useful tool in improving heart function by restoring synchronous ventricular activation and contraction.
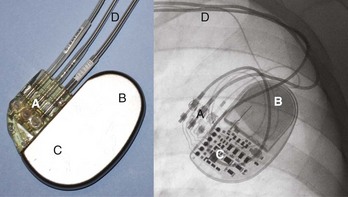
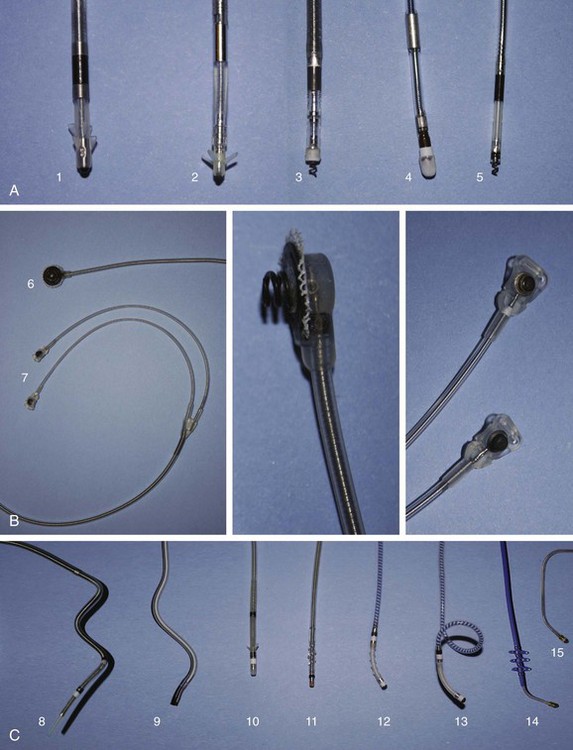
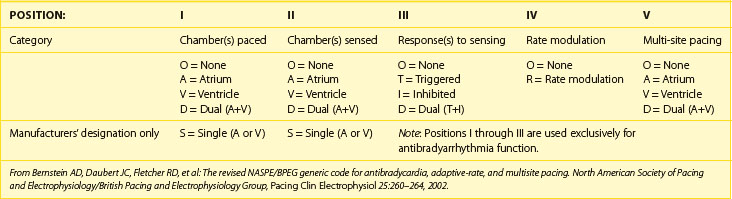
The international revised North American Society of Pacing and Electrophysiology and the British Pacing and Electrophysiology Group (NASPE/BPEG) generic (NBG) pacemaker code (Table 37-1) is generally used to address the pacing chamber, the chambers sensed, and the response to sensing as well as to determine if rate modulation and multi-site pacing have been activated.2 Figure 37-1 shows electrocardiograms (ECGs) with the three most often used methods of cardiac stimulation. In Figure 37-2, a photograph and the x-ray image of a pacemaker with the most important components are shown. These are the connectors for the electrodes leading to the heart; the pulse generator itself comprises the power source and the electronic circuit that controls the timing, the impulses, and a variety of programmable features. The pacemaker is connected to one or more pacemaker electrodes (epicardiac or endocardiac), which allow conduction of the stimulus from the pulse generator to the myocardium (Figure 37-3). Pacemaker electrodes can be implanted in the right atrium, the right ventricle, and the coronary sinus for left-sided stimulation by venous access or inserted surgically for epicardial access. Electrodes can be unipolar or bipolar.
Table 37-1 The Revised NASPE/BPEG Generic (NBG) Code for Antibradycardia, Adaptive-Rate, and Multi-site Pacing
The third part of the pacemaker system (beside the pacemaker itself and the electrodes) is the pacemaker programmer (Figure 37-4), which usually is not considered as critical for pacemaker operation. However, this tool is used to check the integrity of the pacemaker system and control the functioning of the pacemaker. Nowadays, these programmers have evolved into dedicated computers, which have made possible extensive programming of pacemakers and advanced interrogation of pacemaker diagnostics. This chapter focuses on the essential elements and developments of modern pacemaker follow-up.
Organization of the Pacemaker Clinic
In the early pacemaker era, follow-up largely was intended to monitor the proper technical operation of the electronic device itself. Over time, pacemakers have evolved into a stable and trustable technology, and they are now equipped with multiple diagnostic tools. Although the proper technical functioning of the pacemaker still is the most critical part of therapy, a shift from pure technical device checkup to clinical rhythm control is often necessary. Therefore modern pacemaker follow-up takes place in a highly specialized, multi-disciplinary environment. There is general consensus about the various aspects of monitoring cardiovascular implantable electronic devices (CIEDs).3 The essential elements of a well-organized pacemaker clinic are summarized below.
Staff and Assisting Personnel
A well-organized pacemaker clinic can depend on personnel from multiple disciplines. The pacemaker follow-up clinic is under the supervision of the cardiologist and an allied professional with a technical background such as a medical engineer or a skilled nurse or dedicated nurse practitioner. Both physicians and allied professionals should have internationally accepted competencies.4,5 The pacemaker clinic is typically integrated into a general cardiology facility, which facilitates easy access to administrative and other supporting personnel. Involvement of a dedicated psychologist and pediatric cardiologists may be required.
Equipment
Routine pacemaker follow-up is often performed in a dedicated pacemaker control room (Figure 37-5), which allows efficient, high-quality device follow-up. This room should be equipped with an examination table, an electrocardiogram (ECG) recorder, pacemaker programmers with appropriate and updated device software, advanced life support material such as external defibrillator with trans-cutaneous pacing capabilities and resuscitation materials, technical documentation, and specifications of pacemakers in use. Computers connected to the hospital network and the Internet, with online access to electronic patient records, the pacemaker database, and remote follow-up web pages, should be available.
Normal Routine Pacemaker Follow-up
Postimplantation and Predischarge Follow-up
Proper pacemaker functioning and connection of the electrodes must be confirmed in the peri-operative and immediate postoperative periods. After the implantation of a pacemaker system, pacemaker follow-up should be performed on a regular basis to confirm the efficacy of the applied therapy.3,6,7 The first follow-up should be performed before hospital discharge.
Long-Term Device Follow-up
A technical control was normally required 3 months after implantation to verify the output of the pacemaker and to fine-tune the stimulation as the threshold (which varies the most in the first few months because of the endocardiac healing process) returns to the baseline. The output could be optimized at this point in time. If an automatic capture control function is available, checked at the time of discharge, and activated, the first control can be delayed.8
Contents of Routine Ambulatory Pacemaker Follow-up
To achieve the goals of the pacemaker clinic, routine pacemaker follow-up should be performed in a structured way. Box 37-1 summarizes all the elements of a methodical, routine, more advanced control (as needed).
Box 37-1 Follow-up Procedures at the Pacemaker Clinic
History
Potential Pacing-Related Complaints
Pectoral or diaphragmatic muscle stimulation
Position-dependent or motion-dependent palpitations