Chapter 77 Pacemaker and Implantable Cardioverter-Defibrillator Therapy in Pediatric Patients with and Without Congenital Heart Disease
Overview of Pacemaker and Implantable Cardioverter-Defibrillator Therapy
No large clinical trials or prospective studies in children are available to offer guidelines for pacemaker and device implantation in children. For this reason, the adult guidelines have served as a basis for pediatric implantations. The most recent indications for device implantation are shown in Box 77-1 (pacing) and Box 77-2 (ICD or cardiac resynchronization therapy [CRT]).1 This chapter discusses the unique circumstances and special indications in children and adolescents and in those with congenital heart disease that are not addressed by the adult studies and guidelines.
Box 77-1 Indications for Pacing in Children and Adolescents
Class I
Class IIa
Pacemaker Therapy for Children and Patients with Congenital Heart Disease
Several important considerations in young patients separate them from adults. Children, especially neonates, require higher heart rates to maintain an adequate cardiac output. An increasing population of survivors of palliative procedures for various forms of congenital heart disease has suboptimal cardiovascular physiology, compromised myocardial function, or both. They are vulnerable to the effects of bradycardia, which may leave them with inadequate cardiac output and increased vulnerability to both atrial and ventricular arrhythmias. Moreover, loss of AV synchrony associated with complete heart block or junctional bradycardia may result in symptoms at heart rates that would be tolerated in individuals with normal cardiovascular physiology.2,3 In most patients, pacemaker implantation is indicated when symptoms associated with bradycardia are present, with subsequent improvement of those symptoms with chronotropic support, restoration of AV synchrony, or both. Because of the lack of large pediatric randomized double-blind clinical trials, the level of evidence for most recommendations is based on the consensus of experts.
Specific Pacing Issues
Sinus Node Dysfunction
Isolated sinus node dysfunction is extremely rare in children with structurally normal hearts. Pediatric sinus node disease is most commonly encountered after repair of congenital heart disease, with device implantation indicated only for symptomatic patients.4 It can be challenging to correlate bradycardia with symptoms of fatigue, dizziness, or syncope. Before implanting a pacemaker, it is important to exclude reversible causes of bradycardia such as seizure, increased intracranial pressure, hypothyroidism, hypothermia, apnea, sepsis, medications, or other systemic conditions. Since average heart rates decrease as children grow, bradycardia is a relative term, and no specific heart rate “cut-off” that defines an indication for pacing exists.
In a carefully selected subgroup of children with profound bradycardia and asystole associated with pallid breath-holding spells, pacing has been successful in alleviating symptoms.5
The combination of sinus bradycardia with atrial tachyarrhythmias (tachycardia-bradycardia syndrome) is becoming more common as patients survive complex repairs for congenital heart disease. The loss of sinus rhythm is considered an independent risk factor for the development of these intra-atrial re-entrant arrhythmias.6 Although antiarrhythymic drugs may be useful, their use may be limited by pre-existing bradycardia.7 Long-term atrial pacing and atrial anti-tachycardia pacing (ATP) have both been used with equivocal results.7,8
Postoperative Atrioventricular Block
Natural history studies have established a very poor prognosis with up to 50% mortality in patients with permanent heart block after surgical repair of congenital heart disease.9 Advanced second-degree or third-degree postoperative heart block that has persisted for at least 7 days and is not expected to resolve is considered a class I indication for pacemaker placement.1 Patients with transient AV block after surgery have a small but definite risk of late progression to complete AV block decades after surgery and need close monitoring and follow-up.10,11 Patients with residual bi-fascicular block and progressive P-R interval prolongation may be particularly at risk for development of late-onset AV block.12 Because of this possibility, unexplained syncope is a class IIa indication for pacing in these patients once other cardiac and noncardiac etiologies of syncope have been ruled out.1
Congenital Complete Atrioventricular Block
In children with structurally normal hearts, congenital complete AV block (CCAVB) is the most common indication for permanent pacing, and accounts for 20% to 30% of the entire pediatric paced population in large single-center reports.13,14 CCAVB is often caused by fetal exposure to maternal lupus antibodies but may be idiopathic as well. The subgroup of patients with maternal lupus associated CCAVB tend to present with the need for pacing at an earlier age and are more likely to develop dilated cardiomyopathy compared with those with idiopathic CCAVB.15
Class I indications for permanent pacing include a wide QRS escape rhythm, complex ventricular ectopy, or ventricular dysfunction.1 In neonates with a narrow QRS escape rhythm, the class I indication is met when the average heart rate is below 55 beats/min or below 70 beats/min for infants with significant congenital heart disease. Beyond the first year of life, the class IIa indication states that pacing is appropriate for average heart rates below 50 beats/min, or when abrupt pauses of two to three times the basic cycle length occur, or when symptoms of chronotropic incompetence are present.1
Long QT Syndrome
In long QT syndrome (LQTS), pacing prevents bradycardia and pauses and may even shorten the QT interval. Pacing alone has been shown to be efficacious for certain high-risk patients with LQTS, and although most high-risk patients in the modern era are treated with ICD therapy, a simple pacemaker may be a good option for small patients in whom ICD implantation is not feasible.16
Lyme Carditis
Lyme disease is a common cause of acquired heart block in children and should be considered in any child presenting with heart block. In one recent large study of 207 children with Lyme disease, 33 (16%) developed carditis.17 Nine patients had complete heart block, and three of those received temporary pacing, but no patient required permanent pacing. With very rare exceptions, heart block in the setting of Lyme disease is transient and responds to antibiotic therapy. In cases of advanced second-degree or third-degree AV block, some have recommended corticosteroid therapy in addition to antibiotics. The opinion on using steroids is mixed, and evidence is limited to isolated case reports and series.18
Technical Considerations and Challenges of Implantation
General Principles
Pediatric pacemakers should be implanted by specialized teams with expertise in the unique aspects of pacing in children and familiarity with the anatomic variations associated with congenital heart disease.19 Procedures are usually performed with the patient under general anesthesia and monitored by a pediatric cardiac anesthesiologist.
The psychosocial adjustments of the patient and family must also be considered, and trained nurses, play/child-life therapists, and other psychosocial professionals should be made an essential part of the implantation team. The techniques of epicardial and transvenous pacemaker implantation are discussed in detail in other chapters of this book and elsewhere.19
Transvenous Versus Epicardial Systems
Transvenous systems are more reliable and have greater longevity compared with epicardial systems. In one large pediatric cohort, transvenous leads had lower thresholds and significantly more longevity compared with steroid-eluting epicardial leads.20 Epicardial pacing is generally preferred for smaller patients and for patients with congenital heart disease who have intracardiac shunts.21 For the infant who requires lifelong pacing, an epicardial pacing system preserves the venous anatomy and ideally defers transvenous implantation until the child has grown closer to adult size. Although transvenous pacing is technically feasible in infants, lead survival is significantly decreased, and the risk of venous occlusion may present an obstacle to placement of additional leads in the future.22,23 As small patients grow and the distance between the generator and the heart increases, tension can develop on the lead. This problem is sometimes addressed by placing a right atrial loop to introduce more “slack” in the lead, although these loops can promote adhesions of the lead body to the vessel walls, making extraction difficult, and often may not straighten out as planned with growth.24–26
It is clear that infants should receive epicardial pacing systems when indicated, but the choice between the epicardial and transvenous approaches is more difficult in toddlers and young children. The transvenous approach is attractive because it avoids thoracotomy and is associated with increased lead survival time. However, venous thrombosis may be a problem when adult-sized pacing leads are placed into small vessels. One study evaluated 63 children with transvenous pacing leads with echocardiography and venography to determine the incidence of venous thrombosis and found that 18% of them had moderate or severe thrombosis at follow-up.27 Children who had thrombosis were younger at implant (4.5 vs. 8.2 years) and had a higher ratio of lead diameter to body surface area.27 This suggests that children in the age range of 3 to 6 years may have better long-term outcomes with epicardial pacing because venous anatomy is preserved. It also suggests that a two-lead system may have a higher thrombosis risk than a single-lead system and should be avoided unless absolutely necessary.
In the setting of congenital heart disease with intracardiac shunting, a risk of thromboembolic events exists, and epicardial pacing is preferred at any age.21 Epicardial pacing may be used and should be strongly considered in small children, even when trans-venous pacing is technically feasible in the interests of maintaining venous access for future use. Steroid-eluting epicardial leads are preferred, and the lead should be secured in a scar-free area to optimize pacing and sensing thresholds. A limited left thoracotomy approach may be successful in older children or in children with scars from prior thoracotomies.
Single-Chamber Versus Dual-Chamber Pacing
In the setting of heart block, dual-chamber DDD pacing provides AV synchrony and is obviously more physiological than single-chamber ventricular pacing. However, children with normal hearts or repaired congenital heart disease do surprisingly well with rate-responsive VVIR pacing and can be expected to lead active lives.25 The merits of AV synchrony may be outweighed by the challenges of implanting a two-lead transvenous system, including increased surgical risk and operative time and the late risk of venous thrombosis and lead malfunction. When the child reaches adolescence or young adulthood, an upgrade to a dual-chamber system may be indicated. For infants, single-lead epicardial implantation can be accomplished with a smaller incision and with less intrathoracic dissection than in the case of a dual-chamber system. This shortens the recovery time and preserves the chest, heart, and thoracic cavity for future operations. For a school-aged child undergoing transvenous implantation, a single ventricular lead is less likely to cause venous occlusion compared with a two-lead system.
Pectoral Versus Abdominal Implantation
In general, epicardial leads are attached to abdominal pulse generators and transvenous leads are attached to pectoral devices. Although a transvenous lead can be tunneled to an abdominal device, this approach is generally avoided because it exposes the lead to trauma. Submuscular pockets are preferred for pediatric patients and are thought to minimize trauma and improve cosmetic results.28
Single-Lead VDD Pacing Systems
Single-lead VDD pacing combines a traditional ventricular pacing lead with atrial-sensing electrodes that make passive contact with atrial tissue and allow for atrial sensing without atrial pacing capabilities. The ACC/AHA/NASPE (American College of Cardiology/American Heart Association/National Association for Sport and Physical Education) guidelines state that VDD pacemakers are indicated for patients with AV block and normal sinus node function, and no need for atrial pacing.29 These leads are an attractive option for pediatric patients because they provide AV sequential pacing without the need for two leads in a potentially small vascular space. The most obvious disadvantage is that atrial pacing is not available in patients with coexisting sinus node dysfunction or bradycardia related to antiarrhythmic drug therapy. Atrial undersensing can also be a problem because a dedicated atrial lead is lacking. However, problems with atrial undersensing affect only 2% to 5% of these patients and rarely produce clinical symptoms. Data on the extractability of these leads, as compared with others, are not available.
Specific Challenges in Congenital Heart Defects
Transposition of the Great Arteries
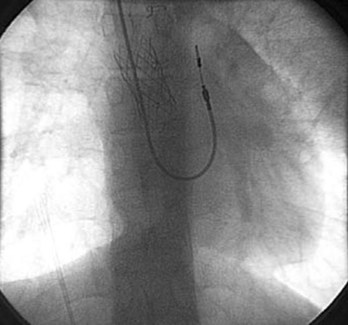
Patients who have undergone intra-atrial baffle repair (Mustard, Senning procedures) often have sinus node dysfunction and atrial flutter as adolescents and adults related to their extensive atrial surgery. At implantation, the atrial lead must be secured to the superior aspect of the anatomic left atrium, now in the physiological right or systemic venous atrium (Figure 77-1). Care must be taken to avoid phrenic nerve stimulation when pacing in this area. Because the systemic venous ventricle is a morphologic left ventricle with smooth walls and small trabeculae, an active fixation lead is preferred.
These patients often develop obstruction of the superior vena cava (SVC), which precludes the transvenous approach to pacing; hence, venography before implantation is important to delineate venous anatomy. Placing a stent in the atrial baffle may open the obstructed area and allow passage of the transvenous leads in some cases.30 The presence of right-to-left atrial or baffle shunts should also be identified and closed before placement of the transvenous pacing leads to prevent paradoxic emboli and strokes.
Single Ventricle
Several anatomic substrates result in single-ventricle physiology and are ultimately palliated with the Fontan operation, the most common being hypoplastic left heart syndrome. The systemic venous return is connected directly to the pulmonary artery and hence, access for transvenous ventricular pacing is lacking. Sinus node dysfunction is very common in this group, and atrial tachyarrhythmias, especially intra-atrial re-entrant tachycardia (IART) or focal atrial tachycardia, become more common as these patients approach adulthood. In single-ventricle patients with pure sinus node dysfunction with no AV nodal disease, a single-chamber atrial pacing system can sometimes be placed via the transvenous approach, provided that no residual “fenestration” that would be a source of paradoxic emboli is present and that atrial tissue can be reached through the systemic venous connection (which may be impossible if the conduit is entirely extracardiac).31 Because of the low-flow state in the systemic venous atrium, thrombosis is a potential concern, and epicardial pacing may be chosen even when transvenous pacing is technically possible.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree