Other Risk Factors for Coronary Artery Disease
Liviu Klein
Philip Greenland
Overview
More than 80% of patients who develop clinically significant coronary artery disease (CAD), and more than 95% of those who will experience a fatal CAD event, have at least one major cardiac risk factor (1,2). Nonetheless, the prevalence of traditional risk factors is almost as high in those without disease as in subsequently affected individuals (1,2,3,4,5,6). As a consequence, the predictive models for risk assessment (7,8), the cornerstone of primary prevention, have a lower than desired accuracy in predicting CAD risk in any individual patient. The search for new risk factors that could refine risk assessment combined with advances in vascular biology in recent years have led to the discovery of a plethora of circulating biomarkers implicated in the pathology of atherosclerosis (Table 11.1). This chapter outlines the relationship between the leading candidate biomarkers and novel risk factors for CAD.
C-Reactive Protein
Historical Considerations and Chemical Structure
C-reactive protein (CRP) was first detected in 1930 by Tillet and Frances, who identified a substance in the sera of patients acutely infected with pneumococcal pneumonia that formed a precipitate when combined with polysaccharide C of Streptococcus pneumoniae (9). It was found subsequently that this reaction was not unique to pneumococcal pneumonia but could be observed with a large variety of other acute infections and inflammatory states.
CRP is a calcium-binding pentameric protein consisting of five identical, noncovalently linked, 23-kDa subunits (10). It is present in trace amounts in humans and appears to have
been highly conserved over hundreds of millions of years (11). CRP is synthesized primarily by hepatocytes in response to activation of several cytokines, such as interleukins 1 and 6, and tumor necrosis factor-α (TNF-α). Because the clearance rate of CRP remains constant, its serum level is determined only by its rate of production.
been highly conserved over hundreds of millions of years (11). CRP is synthesized primarily by hepatocytes in response to activation of several cytokines, such as interleukins 1 and 6, and tumor necrosis factor-α (TNF-α). Because the clearance rate of CRP remains constant, its serum level is determined only by its rate of production.
TABLE 11.1 Selected Novel Risk Factors for CAD | ||
|---|---|---|
|
Measurement and Plasma Concentration
When monitoring states of extremely active inflammation such as sepsis or arthritis that yield CRP levels above 20 to 30 mg/L, qualitative or semiquantitative laboratory techniques, most commonly latex agglutination, have been used. The development of high-sensitivity methods with lower detection limits of 0.2 mg/L allow differentiation of low-level states of inflammation that are required for use in CAD risk assessment. Accurate and rapid quantitative measures of high-sensitivity CRP are obtained using laser nephelometry, rate immunonephelometry or turbidimetry, and enzyme immunoassay (12). Taking into account the day-to-day variability of CRP measurements over time, its predictive value can be improved by using the average of several serial measurements (13).
In healthy persons in the absence of active inflammatory states, CRP levels are usually below 1 mg/L (14). There is no apparent circadian variability, as is observed with cytokines (15), and there is no evidence for seasonal variations as has been reported for fibrinogen (16). CRP has a long half-life, and concentrations appear to be fairly stable over long periods of time in most individuals (17). Heritability studies suggest that 35% to 40% of the variance in CRP levels is genetically determined (18).
CRP serum concentration is physiologically elevated in the third trimester of pregnancy as well as in patients taking oral contraceptives or hormone replacement therapy (19). Levels of CRP are higher in women than in men (20) and are markedly different among different ethnicities: African-American women have higher levels than Caucasians or Hispanics, whereas Chinese women have the lowest CRP levels (20,21,22). Obesity has been associated with high levels of CRP (23) and weight loss leads to a prompt reduction in serum CRP (24).
C-Reactive Protein and Atherosclerosis
Evidence accumulated over the past decade supports a central role for inflammation in all phases of the atherosclerotic process, from lesion initiation through progression and, ultimately, plaque rupture (25). Recruitment of mononuclear leukocytes to the intima is one of the earliest events in the formation of an atherosclerotic lesion and is followed shortly by their adhesion, transmigration into the subendothelial space and transformation into foam cells (26). T lymphocytes are also attracted to the site of early lesion development (27) and along with the endothelial cells secrete cytokines and growth factors, further amplifying the proinflammatory state and promoting migration and proliferation of smooth muscle cells (27). The cells of the atheromatous plaque produce TNF-α, which together with interferon-γ and interleukin-1, increase interleukin-6 and CRP production (27). CRP is expressed in atherosclerotic plaque (28) and may enhance expression of local adhesion molecules (29), increase expression of endothelial plasminogen activator inhibitor 1 (30), reduce endothelial nitric oxide bioactivity (31), and alter low-density lipoprotein (LDL) cholesterol uptake by macrophages (32). The expression of human CRP in CRP-transgenic mice directly enhances intravascular thrombosis (33) and accelerates atherogenesis (34). CRP has been found within thin cap atheromas and immunohistochemical deposition of CRP within plaques corroborates the concept that inflammation is an important component to plaque instability reflected by serum CRP (35).
C-Reactive Protein and Prediction of Cardiovascular Events in Asymptomatic Individuals
The first association of CRP with CAD events in asymptomatic individuals derives from a nested case control study of the observational component of the Multiple Risk Factor Intervention Trial (MRFIT). The study showed that over 17 years of follow-up, CAD deaths among smokers were 4.3-fold greater among those in the highest versus the lowest quartile of CRP (36). These findings were later confirmed in the Physicians’ Health Study, where baseline CRP values were compared for
543 subjects without cardiovascular disease and for 543 who developed such vascular disease over 8 years of follow-up. Men in the highest quartile had a relative risk for myocardial infarction of 2.9 compared with men in the lowest quartile, independent of many of the usual cardiovascular risk factors (37). The same investigators have demonstrated subsequently that women who developed cardiovascular events had higher baseline CRP levels than control subjects and those with the highest levels at baseline had a sevenfold increase in the risk of myocardial infarction or stroke over 3 years of follow-up (38).
543 subjects without cardiovascular disease and for 543 who developed such vascular disease over 8 years of follow-up. Men in the highest quartile had a relative risk for myocardial infarction of 2.9 compared with men in the lowest quartile, independent of many of the usual cardiovascular risk factors (37). The same investigators have demonstrated subsequently that women who developed cardiovascular events had higher baseline CRP levels than control subjects and those with the highest levels at baseline had a sevenfold increase in the risk of myocardial infarction or stroke over 3 years of follow-up (38).
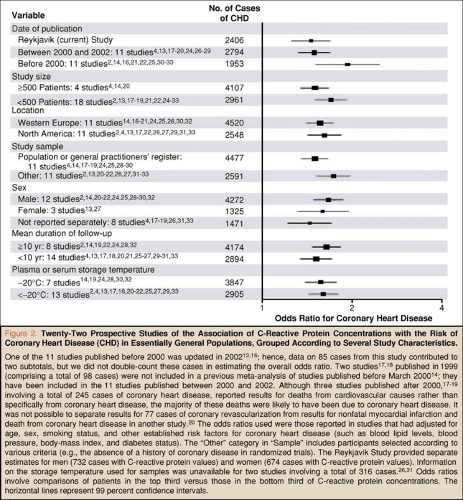 FIGURE 11.1. Prospective studies of CRP and CAD. (Source: Reproduced with permission from Danesh et al. [39]). |
Since the publication of these initial reports, there have been a plethora of studies supporting a role for CRP in cardiovascular event prediction among apparently healthy individuals (39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56). These data are robust and remarkably consistent across over 20 European and American cohorts that included men, women, and middle-aged and older individuals (39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56) (Fig. 11.1). Although the initial studies have suggested an odds ratio for CAD events of about 2.0 (57), more recent data indicate an odds ratio in the range of 1.4 to 1.6 in comparing individuals with baseline values in the top third with those in the bottom third of CRP distribution (39).
C-Reactive Protein and Prediction of Cardiovascular Events in Individuals With Preexisting Cardiovascular Disease
Several studies examined the role of CRP in predicting recurrent events in patients with acute coronary syndromes. One such study found that elevated CRP on admission for ST-elevation myocardial infarction was associated with a sixfold higher rate of ischemic events (recurrent angina, myocardial infarction) and a lower 1-year event-free survival rate (58). In another study, predischarge CRP in the setting of unstable
angina was associated with an eightfold higher rate of recurrent or new myocardial infarctions within 2 weeks of discharge and with lower 1-year event-free survival (59).
angina was associated with an eightfold higher rate of recurrent or new myocardial infarctions within 2 weeks of discharge and with lower 1-year event-free survival (59).
In a recent randomized controlled trial of lipid-lowering strategy in patients with acute coronary syndromes, achieving a lower level of CRP at 30 days post event was associated with a significant improvement in the 2-year event-free survival (myocardial infarction or CAD death), an effect present at all levels of LDL-cholesterol (60). Although the authors emphasized that decreasing both LDL cholesterol below 70 mg/dL and CRP below 1 mg/L is associated with the lowest event rate, it is interesting to note that this reduction in events was minimal compared to decreasing only LDL cholesterol below 70 mg/dL (1.9 versus 2.7 events per 100 person-years) (60).
Interventions That Lower C-Reactive Protein
Although no specific therapies have been developed to decrease CRP and there is no direct evidence that risk of future cardiovascular events is diminished by its reduction, several interventions are effective in decreasing CRP concentration. Lifestyle changes, weight loss, and smoking cessation have beneficial effects on inflammatory markers, including CRP (24,61). Several drugs such as peroxisome proliferator-activated receptors agonists (62), angiotensin converting enzyme inhibitors/angiotensin receptor blockers (63), aspirin (37), niacin (64), clopidogrel (65), and 3 hydroxy-3-methylglutaryl coenzyme A reductase inhibitors (statins) (55,60,66,67) have also been shown to decrease serum CRP levels.
Clinical Implications
Although CRP has been found to be an independent predictor for future cardiovascular events in asymptomatic individuals, most of the epidemiologic studies report only the relative risk and fail to show the absolute risk associated with increased CRP or the receiver operating curve comparing CRP to other risk factors, making it difficult to gauge the true incremental value of using CRP for cardiovascular risk prediction. Recent studies have shown that CRP may have a role in refining the Framingham risk prediction model in middle-aged and older individuals at intermediate risk of CAD events (10-year risk of 10% to 20%) (56,68,69,70) and therefore the most logical use of CRP is in these individuals.
The American Heart Association and the Centers for Disease Control and Prevention issued recommendations on using CRP for risk stratification in primary prevention (71). These recommendations advocate obtaining at least two CRP measurements, preferably 2 weeks apart, and categorizing CRP levels according to approximate tertiles in adult populations: low risk (<1 mg/L), average risk (1.0 to 3.0 mg/L), and high risk (>3.0 mg/L). CRP levels above 10 mg/L generally indicates presence of a significant acute phase response, and further assessment is required to determine the cause. Individuals reclassified as high risk (10-year risk of >20%) based on CRP should have the traditional risk factors treated intensively, and those reclassified as low risk (10-year risk of <10%) may follow a more conservative approach.
Further data from prospective clinical trials are needed to determine if patients should be treated on the basis of elevated CRP alone. One such trial, currently in progress in the United States, is the Justification for the Use of statins in Primary prevention: an Intervention Trial Evaluating Rosuvastatin (JUPITER) (72). This study is investigating whether long-term treatment with rosuvastatin decreases the rate of major cardiovascular events in patients with lower LDL cholesterol and high CRP.
Fibrinogen
Chemical Structure
Fibrinogen is a large (340-kDa) glycoprotein synthesized in the liver and is composed of two identical subunits linked through a disulfide bond. Each of the subunits consists of three polypeptide chains (Aα, Bβ, and γ) encoded by three separate genes on the long arm of chromosome 4 (73). The final step in the coagulation cascade, the conversion of soluble fibrinogen into insoluble fibrin polymer, is mediated by thrombin, which cleaves fibrinopeptide A from the Aα chain and fibrinopeptide B from the Bβ chain. The proteolytic fragments of fibrinogen have several other functions, including stimulating hematopoiesis, promoting smooth muscle proliferation, and having a possible role in containing bacterial infection. Elevated fibrinogen concentrations occur as a consequence of increased hepatic production or reduced clearance from the circulation (74).
Measurement and Plasma Concentration
The circulating fibrinogen concentration ranges from 200 to 400 mg/dL. In practice, assay standardization for fibrinogen has been inadequate, and analytic consistency across reference laboratories remains poor (74). Levels are higher in African Americans and women, and levels increase with age, after menopause, and with increasing body fat (74). Fibrinogen concentrations decrease with exercise and in individuals who consume alcohol (74). Levels also correlate positively with other risk factors for vascular disease, increasing with concentrations of LDL cholesterol and lipoprotein (a) and decreasing with increasing high density lipoprotein (HDL) cholesterol (74). Fibrinogen levels are also higher in patients with hypertension (75) and diabetes mellitus (76). Smoking also increases fibrinogen concentration (77), which may decrease upon smoking cessation (74,78). Higher concentrations of plasma fibrinogen have been observed in smokers with the T148-A455 allele compared with homozygotes for the common C148-G455 allele (79). In addition, fibrinogen is an acute phase reactant that increases in a variety of disorders, including infections, neoplasms, and hepatitis (74).
Fibrinogen and Atherosclerosis
Plasma fibrinogen regulates cell adhesion, chemotaxis, and proliferation, influences platelet aggregation and blood viscosity, interacts with plasminogen binding, and, in combination with thrombin, mediates the final step in clot formation and the response to vascular injury (80,81,82). Recent data also suggest that the association of fibrinogen with CAD may relate to its role in inflammation (83).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


