Operative Correction of Pectus Excavatum and Pectus Carinatum
Christopher S. Muratore
Thomas F. Tracy
Larry R. Kaiser
INTRODUCTION
Pectus excavatum ( funnel chest) and pectus carinatum (keel chest) are the most common chest wall deformities. Pectus excavatum is an anterior chest wall deformity that presents as a posterior depression and frequently associated with rotation of the sternum and the lower costal cartilages. It occurs in up to 1 in 300 to 1 in 1,000 births with a 4 to 1 male predominance. Protrusion of the body of the sternum, pectus carinatum, presents less frequently than excavatum and occurs more commonly in boys as well. The etiology of the pectus anomalies has not been established but the association between pectus excavatum and other musculoskeletal abnormalities, particularly scoliosis and Marfan’s syndrome, suggests that abnormal connective tissue plays a role. A genetic predisposition is supported by a family history of chest wall deformities in approximately 40% of patients. The clinical presentation of pectus deformities varies from a noted depression or protrusion in the neonatal stage that persists throughout childhood and becomes progressive in adolescence. Most commonly, the pectus deformity becomes apparent and progressive with the onset of puberty and the axial growth spurt. Although there is limited physiological dysfunction noted during this initial timeframe, patients may become symptomatic from a cardiopulmonary perspective as they become more active. A universal concern of significance to all pectus patients is the cosmetic disfigurement, which is associated with a serious loss of self-esteem and can affect social behavior. The anterior chest disfigurement appearance becomes a major issue for adolescents at a time of great vulnerability during phases of puberty that is often characterized by excessive physical, social, and emotional changes. Patients with these deformities experience feelings of shame and try to hide their chests as reflected by their choice of clothing or body posture and avoidance of social activities and sports. This compounds the cardiopulmonary symptoms; patients become more withdrawn perhaps adding to their physical symptoms, which has been documented well beyond adolescence into adulthood. The purpose of this chapter is to review the indications for operative repair, to the preoperative evaluation, and to describe the common techniques for operative correction. The discussion focuses on the contemporary minimally invasive Nuss procedure, the classic open Ravitch procedure, and alternative procedures used for secondary operations and adult patients.
 CLINICAL PRESENTATION
CLINICAL PRESENTATIONChildren with pectus excavatum present with a wide spectrum of chest depression deformities from a mildly depressed sternum to a severe case in which the sternum almost abuts the vertebral bodies. The depression is created by two components. The first is posterior angulation of the body of the sternum beginning just below the insertion of the second costal cartilage. The second component is posterior angulation of the costal cartilages-sternal junction due to a seeming overgrowth and deformity of the costal cartilages. The sternum itself appears normal; the posterior angulation is due to the abnormal cartilage growth and position. The deformity maybe broad and shallow or narrow and deep, and asymmetry might exist as well. Pectus excavatum is generally well tolerated in infancy and childhood. Older children, however, may complain of pain in the area of the deformed cartilages or of precordial pain during or after exercise. Some patients might have palpitations, presumably transient atrial arrhythmias and might be associated with mitral valve prolapse. The physiologic impact of pectus excavatum has been the topic of much debate including the evolution of cardiopulmonary testing, which is well documented in the literature. Generally, this has included extensive pulmonary and cardiovascular function evaluation including echocardiographic studies. More recently, pulmonary function tests combined with exercise stress and metabolic testing have been employed, but not uncommonly no physiologic abnormality is detected. Provocative testing with exercise may be the most accurate way to determine the level, if any, of physiologic derangement. Pectus carinatum patients rarely are symptomatic, and no consistent abnormalities related either to cardiac or pulmonary function have been observed. Most commonly, carinatum deformities are less noticeable until adolescence and tend to progress during the pubertal growth spurt.
PREOPERATIVE EVALUATION
Parents bring their child for surgical evaluation at various times. Often, a young child will present with the congenital pectus variant without symptoms or cognitive psychosocial concerns. These patients and families need reassurance and careful follow-up on a yearly basis. Another time for surgical evaluation comes with the prepubertal and pubertal growth spurt. The axial growth during puberty is a common time for worsening of the pectus excavatum depression. The two most popular surgical corrections to date are the modified Ravitch procedure (open technique) and the minimally invasive repair made popular by Nuss (Nuss procedure). The popularity of the minimally invasive Nuss procedure and widespread usage of social media has brought many families and children in for early evaluation. The patient workup for each surgical approach can be assessed at the initial consultation and tailored based on the family’s concerns and intentions as well as their desire for one procedure over another and modified by the surgeon’s preference for surgical repair technique. In some centers,
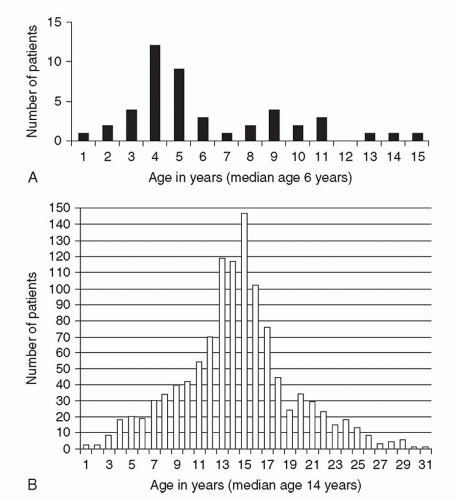
the Ravitch procedure, or some modification, is preferentially performed after the axial growth spurt has concluded. This allows for surgical correction of the deformity with minimal concern for recurrence from continued axial growth. Most often this procedure is performed in the mid-tolate teens. The Nuss procedure can be performed earlier, although not recommended to be performed too early, as continued growth after bar removal will create a similar pectus recurrence scenario. It is our practice to counsel families and patients about the timing of operation in the early-to-mid teens during the axial growth spurt if they are interested in the Nuss procedure as the duration of the bar placement is 2 to 4 years (Fig. 34.1).
the Ravitch procedure, or some modification, is preferentially performed after the axial growth spurt has concluded. This allows for surgical correction of the deformity with minimal concern for recurrence from continued axial growth. Most often this procedure is performed in the mid-tolate teens. The Nuss procedure can be performed earlier, although not recommended to be performed too early, as continued growth after bar removal will create a similar pectus recurrence scenario. It is our practice to counsel families and patients about the timing of operation in the early-to-mid teens during the axial growth spurt if they are interested in the Nuss procedure as the duration of the bar placement is 2 to 4 years (Fig. 34.1).
For those patients with a mild-to-moderate deformity who are sedentary, it is recommended that an exercise program, improved posture, and breathing exercises be prescribed and patients are reevaluated at 6 to 12 months follow-up intervals. Patients with clinically severe deformities at initial presentations can be carefully evaluated with a three-step process.
In addition to a thorough history, physical assessment of symptoms, the initial consultation permits education about the operative options if indicated and allows one to gauge the sincerity of a family’s and child’s wishes to proceed with surgical correction. The preoperative workup includes cross-sectional imaging with computed tomography (CT) scan or magnetic resonance imaging (MRI) of the chest to calculate the Haller index, a measurement of pectus depression severity calculated by dividing the transverse thoracic distance by the anterio posterior (AP) distance from posterior sternum to anterior vertebral body, pulmonary function studies including spirometry, and cardiology evaluation including echocardiogram and electrocardiogram. More recently, pulmonary function testing and stress treadmill cardiac evaluation can be combined as a measure of metabolic function providing an index of baseline cardiopulmonary performance. Surgical correction is generally indicated if the patient presents with symptoms, has a severe pectus excavatum based on the clinical evaluation including CT or MRI Haller index >3.2, evidence of cardiac or pulmonary compression on the CT, MRI, or echocardiogram, evidence of mitral valve prolapse, arrhythmia, or restrictive lung disease. An important additional criteria depending upon stage of pubertal development and social maturation is the degree of significant body image disturbance, which can influence both the child and family. A major consideration is the hesitation on the part of commercial payers to cover the cost of the pectus repair
SURGICAL CONSIDERATIONS
In 1998, Nuss reported a “minimally invasive” correction of pectus excavatum by insertion of a convex steel bar under the sternum. The technique is possiblly based on the malleability and flexibility of the anterior chest wall. Although it requires no cartilage incision or resection and no sternal osteotomy, it is a misnomer to consider it minimally invasive. This technique requires advanced skill, training, and careful pre- and intraoperative planning for successful outcome. It is of utmost importance to take a careful history including any allergy history to the components used in the traditional stainless steel bar. Should there be a history or family history of allergy to metal or Nickel, patch testing should be done. If an allergy is identified and confirmed, a titanium bar can be used instead of a stainless steel bar. The titanium bar, however, is not as malleable as steel and consequently must be bent at the factory with computer-assisted design manufacturing technology, which is readily available from the manufacture. A copy of the patient’s preoperative axial cross-sectional imaging scanning can be provided. Titanium is approximately four times as expensive as steel and therefore should not be used for routine cases where metal allergy is not an issue. The correct size bar needs to be determined in advance and this is accomplished by measuring the distance from the mid-axillary to mid-axillary line across the deepest point of the depression. The bar needs to be 2.5 cm or 1 inch shorter than the distance from the right-to-left mid-axillary line. The correct size and shape of the bar are critical to success of the operation and resulting elevation of the sternum. The stainless steel pectus support bar is bent in the operating room at the time of the operation to conform to the patient’s chest configuration; conversely, the titanium bar needs to be prebent at the manufacturing facility based on the custom measurements.
A preoperative discussion with the patient and family regarding the postoperative pain management is crucial. This has been the topic of some debate as evidenced by numerous reports published in the literature, which favor epidural versus patient-controlled analgesia (PCA). The pain control strategy also needs to be
modified in consultation with the anesthesia and pain management specialists at each institution. It is our preference in consultation with the pediatric anesthesiologist ahead of time to consider a thoracic epidural; however, a one-time lumbar intrathecal injection of morphine has proven equally efficacious. We also favor PCA as this reinforces the motivated patient to be an active participant in their postoperative pain management and recovery.
modified in consultation with the anesthesia and pain management specialists at each institution. It is our preference in consultation with the pediatric anesthesiologist ahead of time to consider a thoracic epidural; however, a one-time lumbar intrathecal injection of morphine has proven equally efficacious. We also favor PCA as this reinforces the motivated patient to be an active participant in their postoperative pain management and recovery.
Nuss Procedure
The operation is performed under general anesthesia (Fig. 34.2). Careful attention to pressure points and padding is essential and both arms are abducted comfortably so as not to cause injury. Some surgeons perform the procedure from the patients right to left, whereas others perform it from left to right. Moreover, other surgeons make a third incision in the subxiphoid region and apply a towel clip or a bone hook to help elevate the sternum for passage of finger or dissecting bar under the sternum. It is our practice once under anesthesia to measure the left-to-right mid-axillary distance again, to confirm the proper bar choice and then to bend the bar appropriately such that a slight overcorrection will be fashioned in the sternal region leaving a 2- to 4-cm flat section in the middle of the bar for sternal support. A 5.0-mm trocar is inserted either inferior to the site of bar placement or superior but in either position to allow for proper orientation and visualization of the mediastinum and passage of the bar across the mediastinum. Using CO2 insufflation, a 5.0-mm, 30-degree scope will help accomplish this visualization and safety. Once the deepest portion of the pectus depression is appreciated, bilateral subcutaneous incisions can be created just off the mid-axillary lines and carried to the height of the pectoral ridges bilaterally. Employing unilateral thoracoscopy, the pectus introducer bar can be passed through the subcutaneous tunnel to the pectoral ridge and carefully introduced into the thoracic cavity under direct visualization (Fig. 34.3A-34.3F




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree