Fig. 30.2 ECG in non-ST segment elevation myocardial infarction (NSTEMI). Sinus bradycardia, heart rate 40 b/min. The P wave shows a late predominantly negative deflection in lead V1 (left atrial enlargement). PR interval markedly lengthened at 320 ms. QRS complexes unremarkable (perhaps generally a bit small). The T wave is flat in lead I, inverted (just) in lead aVL, and biphasic in leads V4–6, i.e. T wave changes laterally. The T wave in lead V1 is upright (as opposed to the normal inversion). This patient has T wave changes only, the distribution of which suggests an acute lesion in a major branch of the circumflex coronary artery, or less likely, a branch of the left anterior descending. The sinus bradycardia suggests good-going beta-blocker therapy (though the heart rate is too slow for beta-blocker therapy to be the only explanation), or sinus node disease (which often relates to disease of the sinus node branch of the right coronary artery). The long PR interval partly relates to the sinus bradycardia, but also suggests intrinsic conducting tissue disease, which could be due to fibrosis, or perhaps right coronary artery disease affecting the conducting tissue.
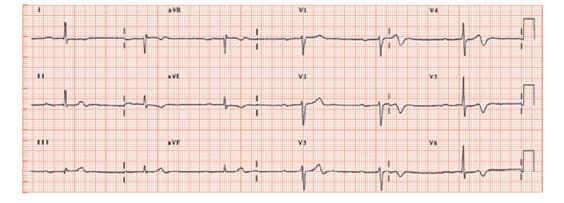
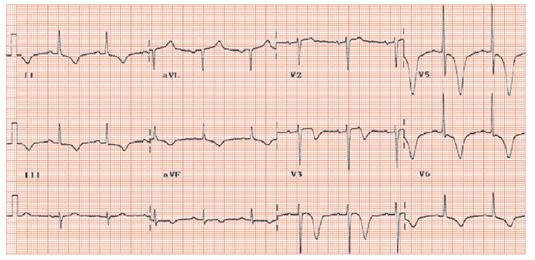
Fig. 30.3 Pan-anterior T wave inversion – the ‘LAD syndrome’ ECG. Sinus rhythm, heart rate 63 b/min, normal P wave. Normal QRS axis. Normal R wave height, no pathological Q waves. The T wave in leads I, II, aVL, and leads V2–6 are very abnormal, showing deep symmetrical T wave inversion. This ECG pattern is so suggestive as to be pathognomonic for a lesion in the left anterior descending coronary artery, often in the proximal portion, and is termed the ‘LAD syndrome’ ECG. It is also found in the very rare condition of Tako-tsubo syndrome (see Chapter 27).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


