A chronic total occlusion (CTO) is defined as an occlusive (100% stenosis) coronary lesion with anterograde Thrombolysis In Myocardial Infarction 0 flow for at least 3 months. CTOs are common in patients referred for coronary angiography (up to 33%) and are associated with angina, impaired quality of life, and reduced survival. Unfortunately, CTO percutaneous coronary intervention continues to be underperformed worldwide (10% to 15% at most institutions, ∼30% where expert operators are available). The aim of this study was to address common fallacies pertaining to CTOs among cardiologists by providing a concise review of pertinent previously published reports along with an update on safety and efficacy of state-of-the-art CTO percutaneous coronary intervention techniques.
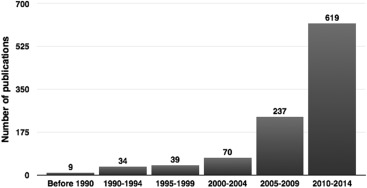
A chronic total occlusion (CTO) is defined as an occlusive (100% stenosis) coronary lesion with anterograde Thrombolysis In Myocardial Infarction 0 flow for at least 3 months. CTOs are seen in up to 33% of patients who underwent coronary angiography ( Table 1 ). Therefore, it is not surprising that the interest of the scientific community has been growing exponentially over the course of the last decade ( Figure 1 ).
| CTO prevalence ∗ | CTO PCI prevalence † | |
|---|---|---|
| Christofferson 2005 | 25% | 11% |
| Claessen 2009 (STEMI population) | 13% | |
| Werner 2009 | 33% | 18% |
| Jolicoeur2012 | 4.6% | |
| National registries | ||
| Grantham 2009 (NCDR) | 5.5% | 14% |
| Råmunddal 2014 (SCAAR) | 7.8% | 22% |
| CTO PCI centers | ||
| Fefer 2012 | 18% | 30% |
| Jeroudi 2014 | 19% | 30% |
∗ CTO prevalence: patients with CTO/total cath laboratory patient population (with or without coronary artery disease) excluding coronary artery bypass graft patients.
† CTO PCI prevalence: patients with CTO PCI /total patients with CTO.
Aside from centers with advanced CTO percutaneous coronary intervention (PCI) programs, the overall CTO PCI attempt rate remains low averaging 10% to 15% ( Table 1 ). Common reasons for low attempt rates include lack of awareness of pertinent data demonstrating benefit of CTO PCI, combined with traditionally low success rates and high complication rates. The purpose of this review is to address common CTO fallacies and briefly describe current CTO PCI state-of-the-art practices with focus on safety and efficacy.
Myth no. 1: CTOs Are Benign Lesions That Do Not Need to Be Revascularized
Data from observational studies ( Supplementary Table ) suggest that revascularization of a CTO conveys several potential advantages ( Figure 2 ). First, it has been shown that the area of myocardium distal to a CTO (as evaluated with fractional flow reserve) is nearly always ischemic, irrespective of the degree of collateralization. Successful CTO PCI effectively relieves ischemia and is therefore associated with less angina, improved physical function and quality of life, as compared with a failed attempt.
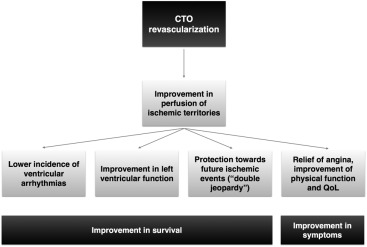
The presence of a CTO in a non–infarct-related artery (IRA) has been associated with worse outcomes in patients presenting with ST-elevation myocardial infarction. If the coronary bed distal to a CTO depends on collateral flow from the IRA, the area at risk of the IRA would extend beyond its own supply territory, including also the myocardial region that depends on the CTO artery, thus resulting in larger infarct size (“double jeopardy” concept).
The presence of a CTO has been associated with incomplete revascularization, which in turn has been linked to persistent left ventricular (LV) dysfunction on follow-up. Additionally, late percutaneous revascularization of an occluded artery after myocardial infarction (>12 hours and up to 60 days: “subacute total occlusion”) has been associated with improved LV remodeling (and hence better survival), as compared with medical therapy. This beneficial effect of PCI is maintained also when the latter is performed for >3 months after occlusion: CTO PCI has been shown to improve LV remodeling and function at medium-and long-term follow-up.
Additional evidence on the nonbenign nature of CTO comes from the analysis of the arrhythmic potential of these lesions. In a cohort of implantable cardioverter-defibrillator recipients, patients with a CTO experienced a higher incidence of appropriate shocks for malignant ventricular arrhythmias, as compared to subjects without CTO. Finally, ventricular arrhythmias can manifest as sudden death in patients with CTO even in the absence of myocardial scar, thus being related with an ischemic phenomenon.
As a result of all the aforementioned beneficial effects, a successful CTO PCI has been repeatedly associated with better survival at follow-up (a finding potentially driven by more frequent complete revascularization), as compared with a failed attempt.
Myth no. 2: There Are Alternative and More Effective Ways to Deal With CTO than PCI
In patients with CTO, PCI effectively relieves ischemia and a baseline ischemic burden >12.5% of LV myocardium has been shown to identify those most likely to have a significantly decreased ischemic burden after PCI. Even patients with CTO with well-developed collateral circulation benefit from revascularization (either percutaneous or surgical) because patients who underwent revascularization have better survival rate on follow-up.
Regarding the comparison between PCI and coronary artery bypass graft (CABG), subjects who underwent CTO PCI suffered a higher incidence of repeat revascularization, but there were no differences in death and major adverse cardiac events. Similar observations come from the SYNergy between PCI with TAXus and cardiac surgery (SYNTAX) trial, in which patients with CTO who underwent PCI experienced a twice as high incidence of revascularization during follow-up, but no differences in other end points.
Globally, these data suggest that revascularization is superior to medical therapy in patients with CTO and the method of revascularization influences exclusively the incidence of a nonhard end point such as repeat revascularization (lower in patients with CABG).
Myth no. 2: There Are Alternative and More Effective Ways to Deal With CTO than PCI
In patients with CTO, PCI effectively relieves ischemia and a baseline ischemic burden >12.5% of LV myocardium has been shown to identify those most likely to have a significantly decreased ischemic burden after PCI. Even patients with CTO with well-developed collateral circulation benefit from revascularization (either percutaneous or surgical) because patients who underwent revascularization have better survival rate on follow-up.
Regarding the comparison between PCI and coronary artery bypass graft (CABG), subjects who underwent CTO PCI suffered a higher incidence of repeat revascularization, but there were no differences in death and major adverse cardiac events. Similar observations come from the SYNergy between PCI with TAXus and cardiac surgery (SYNTAX) trial, in which patients with CTO who underwent PCI experienced a twice as high incidence of revascularization during follow-up, but no differences in other end points.
Globally, these data suggest that revascularization is superior to medical therapy in patients with CTO and the method of revascularization influences exclusively the incidence of a nonhard end point such as repeat revascularization (lower in patients with CABG).
Myth no. 3: CTO PCI Is Technically Very Difficult and Is Associated With a High Complication Rate and a Low Success Rate
One of the major obstacles that have hampered the widespread adoption of CTO PCI is the difficulty of the procedure, along with its greater risk of complications, as compared with non-CTO PCI. Indeed, there has been a very steep learning curve for CTO PCI across the past 3 decades, with success rates <80% even in experienced centers in the 1990s ( Figure 3 ). The advances in CTO PCI technique and the introduction of dedicated devices allowed an improvement in outcomes with success rates of 80% to 90% in specialized centers during the 2000s. Moreover, the introduction of drug-eluting stents led to long-lasting clinical results, with significantly reduced need for repeat revascularization (≤8% at 3 to 5 years), as compared with bare-metal stents.
Historically, complications of CTO PCI have also been a concern, with nonnegligible rates, compared to non-CTO PCI. However, because of advances in techniques and devices, CTO PCI has become a safer intervention, with rates of perforation with tamponade (0.4% to 1%), contrast-induced nephropathy (1%), myocardial infarction (1%), and death (0.4% to 1%), only slightly higher than non-CTO PCI.
History of Modern CTO PCI
Until approximately 2010, the published series included selected patient populations because CTO PCI was almost exclusively based on anterograde wire escalation, a technique that has been proved to be effective only in a limited CTO subset (well-visualized proximal cap, suitable and visible distal target, the presence of microchannels within the CTO, minimal or no calcification, occlusion length <20 mm, and no angulation >45° within the CTO).
The first decade of the 2000s, however, witnessed the introduction and progressive adoption of novel techniques that allowed achievement of higher rates of successful revascularization. In particular, anterograde dissection-reentry techniques, adopted from peripheral interventions and pioneered in the coronary arteries by Colombo, facilitated safe and effective crossing of long occlusions. Retrograde techniques, such as controlled anterograde and retrograde subintimal tracking pioneered by Katoh and reverse controlled anterograde and retrograde subintimal tracking, paved the way to the efficient and safe percutaneous revascularization of specific lesion subsets previously considered off limits for even the most experienced CTO operators (ambiguous proximal cap, poor distal target, and long occlusions).
The integration and implementation of all these scientific contributions (in particular, the retrograde approach and dissection-reentry techniques) boosted the transition toward modern CTO PCI technique, with tangible effects on procedural success. From 2009 to 2012, groups of expert operators from Japan, the United States, and Canada published their experience with modern retrograde technique in all-comer series (little or no anatomic exclusion criteria were used), approaching a 90% success rate.
These experiences culminated with the formal theorization of the so-called “hybrid algorithm”. With the implementation of this new tool and dedicated devices for collaterals dilatation during retrograde approach (Corsair; Asahi Intecc, Aichi, Japan; and Turnpike; Vascular Solutions, Minneapolis, Minnesota) and for anterograde dissection-reentry (CrossBoss and StingRay; Boston Scientific, Natick, Massachusetts), the success rate of CTO PCI has been consistently shown to approximate 90%, even when performed by novel operators.
Indications and Modalities of CTO Revascularization
Figure 4 outlines several real-world scenarios of patients with CTO, with recommended indications for revascularization. Revascularization should be strongly pursued in patients with symptoms attributable to the presence of a CTO, even without information on ischemia/viability. In asymptomatic subjects with inducible ischemia and/or viability, revascularization should also be attempted, albeit considering the chances of success and the risks of the procedure. It must be underscored that the indications for revascularization should include not only the possible impact on prognosis but also symptomatic relief. Additionally, clinicians should strive to actively look for inducible ischemia/viability in patients with CTO because in real-world practice, subjects with CTO are not only undertreated but also underdiagnosed, thus lowering even more their likelihood of undergoing revascularization.
Figure 5 provides a roadmap for the choice of method of revascularization in patients with CTO depending on the presence of single or multivessel disease. Aiming for a complete revascularization is of paramount importance because incomplete revascularization is associated with worse prognosis. In patients with CTO with multivessel disease, this implies that percutaneous revascularization should not be limited to non-CTO lesions in an effort to improve collateralization to the CTO because this strategy has no pathophysiologic foundations and has been shown to be associated with worse long-term survival rate. In these patients, if the CTO vessel is the left anterior descending artery, CABG should be considered as the revascularization method of choice. If the occluded vessel is the right coronary artery or circumflex, complete percutaneous revascularization can be attempted: we advocate starting with PCI of the CTO vessel and subsequently performing non-CTO vessel PCI. In case of failure of CTO PCI, CABG should be considered. Additional factors shifting the balance toward CABG in multivessel disease are, a SYNTAX score >22, diabetes, and LV dysfunction. In case of one-vessel disease involving a CTO, PCI should be the revascularization method of choice. CABG can be considered in case of low likelihood of success of PCI in case of left anterior descending CTO. The Supplementary Material presents real-world examples of recommended CTO patient management.




