Significant mitral regurgitation (MR) constitutes an important co-existing valvular heart disease burden in the setting of aortic valve stenosis. There are conflicting reports on the impact of significant MR on outcomes after transcatheter aortic valve implantation (TAVI). We evaluated the impact of MR on outcomes after TAVI by performing a meta-analysis of 8 studies involving 8,927 patients reporting TAVI outcomes based on the presence or absence of moderate-severe MR. Risk ratios (RRs) were calculated using the inverse variance random-effects model. None-mild MR was present in 77.8% and moderate-severe MR in 22.2% of the patients. The presence of moderate-severe MR at baseline was associated with increased mortality at 30 days (RR 1.35, 95% confidence interval [CI] 1.14 to 1.59, p = 0.003) and 1 year (RR 1.24, 95% CI 1.13 to 1.37, p <0.0001). The increased mortality associated with moderate-severe MR was not influenced by the cause of MR (functional or degenerative MR; RR 0.90, 95% CI 0.62 to 1.30, p = 0.56). The severity of MR improved in 61 ± 6.0% of patients after TAVI. Moderate-severe residual MR, compared with none-mild residual MR after TAVI, was associated with significantly increased 1-year mortality (RR 1.48, 95% CI 1.31 to 1.68, p <0.00001). In conclusion, baseline moderate-severe MR and significant residual MR after TAVI are associated with an increase in mortality after TAVI and represent an important group to target with medical or transcatheter therapies in the future.
Transcatheter aortic valve implantation (TAVI) is the standard of care for severe symptomatic aortic stenosis (AS) in inoperable patients and an alternative to surgical aortic valve replacement (SAVR) in high–surgical risk patients. However, TAVI is still a relatively novel technology, and short- and long-term morbidity and mortality after TAVI remains significant. There is substantial interest in the identification and modification of factors influencing morbidity and mortality after TAVI. Moderate-severe mitral regurgitation (MR) is present in 20% to 30% of patients who underwent TAVI and constitutes a significant coexisting valvular heart disease burden. Before TAVI therapy is extended to patients with mixed valvular heart disease (severe AS and significant MR) who are surgical candidates, the impact of coexisting MR on TAVI outcomes must be assessed systematically. There are several clinically relevant and unresolved issues that need to be addressed in patients with coexisting severe AS and significant MR who underwent TAVI. These include the impact of baseline MR severity, cause of MR, or transcatheter heart valve type on outcomes; the impact of TAVI on MR severity; and the impact of residual MR on outcomes. We performed a meta-analysis and systematic review of the literature to evaluate the impact of coexisting MR on outcomes after TAVI. Whether medical therapy or newer transcatheter mitral technologies can be used to optimize outcomes in the patients who underwent TAVI needs to be studied.
Methods
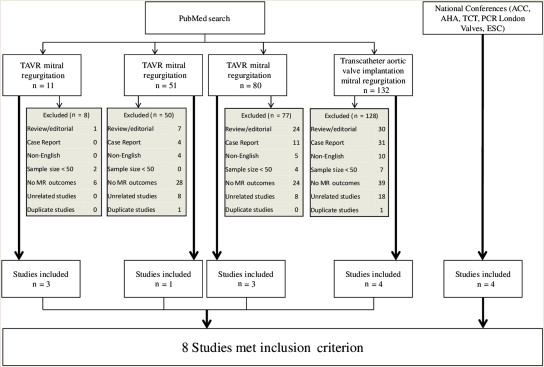
A systematic review of literature was performed following the Quality of Reporting of Meta-Analysis guidelines. We searched the PubMed database for published studies, prospective and retrospective, in English using the terms “TAVI mitral regurgitation,” “TAVI mitral regurgitation,” “transcatheter aortic valve replacement and mitral regurgitation,” and “transcatheter aortic valve implantation and mitral regurgitation.” Abstract lists from the 2012 to 2013 scientific meetings of the American Heart Association, the American College of Cardiology, Transcatheter Cardiovascular Therapeutics, the European Society of Congress, and PCR London Valves were searched. The full text of all the studies evaluating the interaction between MR and TAVI was reviewed to screen for eligible studies for the meta-analysis. The final search was run on November 12, 2013.
Studies were included if they met the following criteria: (1) reported data on 30-day and/or 1-year TAVI outcomes based on the presence/absence of MR, (2) at least 50 patients in each study, (3) reported to have enrolled consecutive patients, and (4) publication in a peer-reviewed journal or presentation at a major national cardiology meeting. In cases of multiple reports from the same center/group, the report with the largest sample size was selected.
MR severity was graded as none (grade 0), mild (grade 1), moderate (grade 2), or severe (grade 3) according to the American Society of Echocardiography and the European Association of Echocardiography recommendations for the assessment of valvular heart disease, integrating structural, Doppler, and quantitative parameters. Degenerative MR was defined as MR secondary to a structural abnormality in the mitral valve apparatus, whereas functional MR was defined as MR secondary to regional or global left ventricular remodeling without structural abnormalities of the valve apparatus. Residual MR was assessed based on the first available echocardiogram up to 30 days after TAVI. All-cause mortality at 30 days and 1 year after TAVI was evaluated.
Data were extracted independently by 2 reviewers (TC and AN), and disagreements were reviewed together by the 2 reviewers and resolved by discussion. In addition to the data on 30-day and 1-year outcomes, other variables abstracted included, but were not limited to, the following: first author and senior author; year of publication; country of study; study size; mean age, Society of Thoracic Surgeons score, and EuroScore; type of transcatheter heart valve and approach used; duration of follow-up; study definitions, inclusion and exclusion criteria; and other primary and secondary outcomes of each study. The first author and senior author of included studies were contacted to obtain additional data to evaluate the impact of the cause of MR, individual grades of MR, and residual MR on outcomes after TAVI; of these, the authors of 7 of 8 studies provided the relevant information to perform these additional analyses.
The following end points were evaluated: (1) impact of baseline MR on mortality (primary end point) and other secondary end points after TAVI, (2) impact of the cause of MR (functional or degenerative) on outcomes after TAVI, (3) impact of MR grade on outcomes after TAVI, (4) change in the severity of MR after TAVI, (5) impact of residual MR on mortality after TAVI, and (6) stratification of mortality according to valve type.
The inverse variance random-effects model was used to obtain risk ratio (RR) and 95% confidence intervals (CIs). The event rates were estimated from the survival curves, when not reported, using methods as described previously. Meta-regression analysis was performed to evaluate the impact of individual variables on the study effect size. Egger’s test was used to assess publication bias. A p value <0.05 was considered statistically significant. Heterogeneity was assessed using Q-statistic and I 2 test. Sensitivity analysis was performed by excluding 1 study at a time and switching from random-effects to a fixed-effects model. Statistical analysis was performed using Review Manager Statistics Software, version 5.1 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark).
Results
A total of 274 published manuscripts were identified on Pubmed using the search by keywords ( Figure 1 ). The final analysis was performed on a total of 8 studies comprising 8,927 patients, meeting all inclusion and no exclusion criteria. The studies included 7 nonrandomized registries and 1 study reporting combined outcomes from the randomized controlled Placement of Aortic Transcatheter Valves (PARTNER) trials (cohorts A and B). Baseline characteristics of the individual studies are summarized in Tables 1 and 2 . None-mild MR was present in 77.8% (6,942 of 8,927) and moderate-severe MR in 22.2% (1,985 of 8,927) of the patients. In the 7 studies reporting the prevalence of moderate and severe MR separately, moderate MR was present in 18.9% (1,593 of 8,428) and severe MR in 3.4% (288 of 8,428) of patients. TAVI was performed by transfemoral approach in 76.0% (3,894 of 5,127), transapical approach in 20.9% (1,071 of 5,127), subclavian approach in 2.1% (107 of 5,127), and transaortic approach in 1.1% (55 of 5,127) of patients; information on vascular approach was not available in 41.4% (3,800 of 8,927) of the patients. The balloon-expandable Edwards valve (Cribier-Edwards/Edwards-SAPIEN/Sapien XT; Edwards Lifesciences, Irvine, California) was used in 72.6% (6,289 of 8,659), and the self-expanding Medtronic CoreValve was used in 27.4% (2,370 of 8,659) of patients.
| Study | Country | Valve type | Edwards valve | CoreValve | Sample size | Females | Age (Mean ± SD) in years | ||
|---|---|---|---|---|---|---|---|---|---|
| None-mild MR | Moderate-severe MR | None-mild MR | Moderate-severe MR | ||||||
| Barbanti et al. | North America | Edwards | 499 (100.0%) | – | 499 | 177 (44.7%) | 56 (54.4%) | 83.2 ± 7.7 | 84.5 ± 6.6 |
| Baumgartner et al. | Europe | Edwards | 2615 | – | 2615 | 1186 (56.6%) | 322 (62.0%) | 81.4±6.3 | 81.9±6.1 |
| Bedogni et al. | Italy | MCV | – | 1007 (100.0%) | 1007 | 375 (56.0%) | 180 (53.4%) | 81 ± 5 | – |
| Van Belle et al. | FRANCE 2 | Both | 2137 (66.9%) | 1058 (33.1%) | 3195 | – | – | – | – |
| Hutter et al. | Germany | Both | – | – | 268 | 132 (63.5%) | 35 (58.3%) | – | – |
| Khawaja et al. | London | Edwards | 316 | – | 316 | 108 (42.2%) | 27 (45.0%) | 81.8±8.9 | 83.2±7.4 |
| Ruck et al. | Sweden | Both | 271 (47.0%) | 305 (53.0%) | 576 | – | – | 81.3 | 82.2 |
| Toggweiler et al. | Canada | Edwards | 451 (100.0%) | – | 451 | 163 (51.1%) | 76 (57.6%) | 81 ± 9 | 82 ± 7 |
| Cumulative | 6289 (72.6%) | 2370 (27.4%) | 8927 | 2141 (41.5%) | 696 (13.5%) | ||||
| Study | None-mild MR | Moderate-severe MR | Moderate MR | Severe MR | Improvement in MR | Worsening of MR | No change in MR |
|---|---|---|---|---|---|---|---|
| Barbanti et al. | 396 (79.4%) | 103 (20.6%) | – | – | 30 (57.7%) | 3 (5.8%) | 19 (36.5%) |
| Baumgartner et al. | 2096 (15.1%) | 519 (19.8%) | 462 (17.7%) | 57 (2.2%) | 378 (5.8%) | 13 (2.5%) | 128 (24.7%) |
| Bedogni et al. | 670 (39.7%) | 337 (33.8%) | 243 (24.3%) | 94 (9.4%) | 100 (11.5%) | 6 (2.3%) | 155 (59.4%) |
| Van Belle et al. | 2534 (12.4%) | 661 (20.7%) | 603 (18.9%) | 58 (1.8%) | – | – | – |
| Hutter et al. | 208 (77.6%) | 60 (22.4%) | 41 (15.2%) | 19 (7.1%) | 21 (96.8%) | 2 (6.5%) | 8 (25.8%) |
| Khawaja et al. | 256 (81.1%) | 60 (18.9%) | 53 (16.7%) | 7 (2.2%) | 32.46 (50.0%) | 0.0 | 27.5 (9%) |
| Ruck et al. | 463 (68.8%) | 113 (19.6%) | 102 (17.7%) | 10 (1.8%) | – | – | – |
| Toggweiler et al. | 319 (87.8%) | 132 (29.3%) | 89 (19.7%) | 43 (9.5%) | 73 (22.7%) | 1 (0.8%) | 22 (16.7%) |
| Cumulative | 6942 (77.8%) | 1985 (22.2%) | 1593 (18.9%) | 288 (3.4%) | 61% ± 6.0% | 3.0% ± 1.0% | 36.0% ± 4.0% |
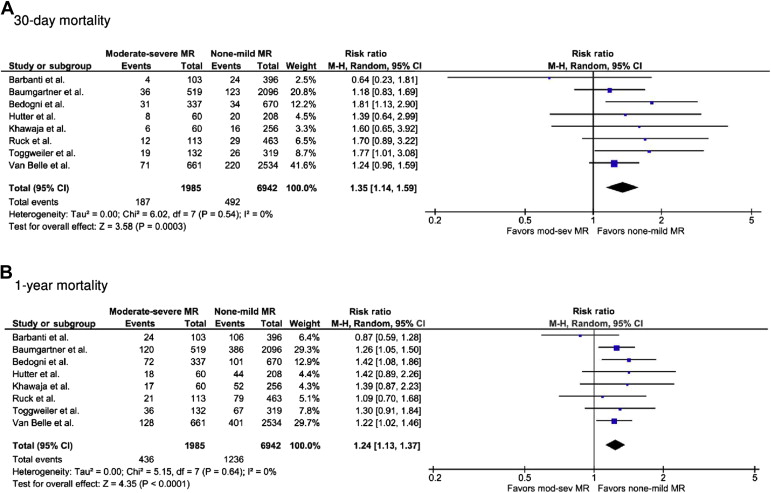
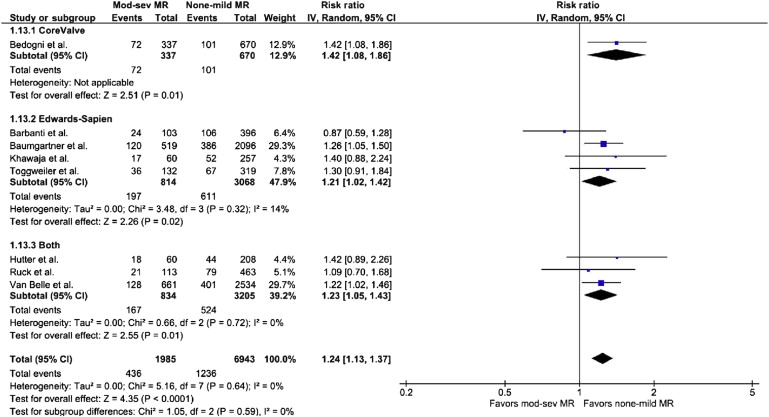
Study outcomes are listed in Table 3 . The presence of moderate-severe MR at baseline was associated with increased all-cause mortality at 30 days (RR 1.35, 95% CI 1.14 to 1.59, p = 0.0003, I 2 = 0%, chi-square = 6.02) and 1 year (RR 1.24, 95% CI 1.13 to 1.37, p <0.0001, I 2 = 0%, chi-square = 5.15; Figure 2 ). The presence of moderate-severe MR was associated with increased 30-day rehospitalization rates (RR 1.75, 95% CI 1.02 to 2.99, p = 0.04, I 2 = 0%, chi-square = 0.60); the re-hospitalization rates at 1 year were not different between the 2 groups (RR 1.02, 95% CI 0.81 to 1.79, p = 0.36, I 2 = 79%, chi-square = 9.41; Supplementary Figure 1 ). There was no difference in the proportion of patients in the New York Heart Association heart failure classes I and II between the 2 groups, at 30 days or 1 year.
| Outcome | Risk ratio | 95% CI | I 2 | Chi 2 | p-value |
|---|---|---|---|---|---|
| All – cause mortality | |||||
| 30-day | 1.35 | 1.14-1.59 | 0.0% | 6.02 | 0.0003 |
| 1 year | 1.24 | 1.13-1.37 | 0.0% | 5.15 | <0.0001 |
| Cardiac mortality | |||||
| 30-day | 1.30 | 0.63-2.67 | 66.0% | 5.85 | 0.48 |
| 1 year | 1.39 | 1.13-1.72 | 6.0% | 2.12 | 0.002 |
| Rehospitalization | |||||
| 30-day | 1.75 | 1.02-2.99 | 0.0% | 0.60 | 0.04 |
| 1 year | 1.20 | 0.81-1.79 | 79.0% | 9.41 | 0.36 |
| NYHA functional class | |||||
| 30-day | 0.98 | 0.91-1.04 | 71.0% | 7.01 | 0.46 |
| 1 year | 0.96 | 0.89-1.04 | 55.0% | 4.42 | 0.35 |
| Stroke | 0.69 | 0.37-1.30 | 0.0% | 0.57 | 0.25 |
| Pacemaker | 0.90 | 0.54-1.49 | 68.0% | 9.28 | 0.67 |
| Subgroups by valve type | |||||
| CoreValve | 1.42 | 1.08-1.86 | – | – | 0.01 |
| Edwards | 1.21 | 1.02-1.42 | 14.0% | 3.48 | 0.02 |
| Combined | 1.23 | 1.05-1.43 | 0.0% | 0.66 | 0.01 |
| Subgroups by individual grades of MR | |||||
| Mod. vs. none-mild MR | 1.32 | 1.03-1.70 | 58.0% | 11.96 | 0.03 |
| Sev. vs. none-mild MR | 1.75 | 0.73-4.22 | 89.0% | 46.38 | 0.21 |
| Sev. vs. mod. MR | 1.29 | 0.76-2.20 | 67.0% | 15.08 | 0.35 |
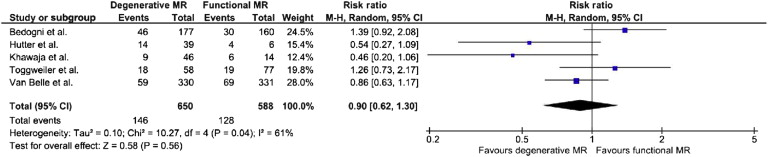
Five studies provided information on 1-year mortality in patients with moderate-severe MR at baseline, stratified according to the cause of MR (functional MR, n = 588; degenerative MR, n = 650) ; 2 of the 5 studies had <20 patients in the functional MR group. In patients with moderate-severe MR at baseline, 1-year mortality was not statistically different between functional or degenerative MR groups (RR 0.90, 95% CI 0.62 to 1.30, p = 0.56, I 2 = 61%, chi-square = 10.27; Figure 3 ).
Mortality at 1 year was analyzed according to the type of transcatheter heart valve implanted. One study used the CoreValve device, 4 studies used the Edwards valve, and 3 studies used both valve types. Consistent with the increased 1-year mortality overall (as reported previously), both CoreValve (RR 1.42, 95% CI 1.08 to 1.86, p = 0.01, heterogeneity not applicable) and Edwards valve studies (RR 1.21, 95% CI 1.02 to 1.42, p = 0.02, I 2 = 14%, chi-square = 3.48) had a statistically significant increase in 1-year mortality with moderate-severe MR ( Figure 4 ).
We evaluated the impact of MR grade on 1-year mortality after TAVI. Six studies including 5,812 patients (none-mild MR, n = 4450; moderate MR, n = 1131; severe MR, n = 231) provided information on 1-year mortality, stratified according to the MR grade. There was a statistically significant increase in 1-year mortality associated with moderate MR compared with none-mild MR (RR 1.32, 95% CI 1.03 to 1.70, p = 0.03, I 2 = 58%, chi-square = 11.96) and a trend toward increased mortality with severe MR compared with moderate MR (RR 1.29, 95% CI 0.76 to 2.20, p = 0.35, I 2 = 67%, chi-square = 15.08) or severe MR compared with none-mild MR (RR 1.75, 95% CI 0.73 to 4.22, p = 0.21, I 2 = 89%, chi-square = 46.38; Table 3 ). The lack of statistical significance in analyses involving severe MR was related to the relatively small number of patients with severe MR. With the performance of sensitivity analysis by switching from random-effects to fixed-effects model, the trend toward increased mortality became statistically significant for both severe MR compared with none-mild MR (RR 1.91, 95% CI 1.49 to 2.43, p <0.00001, I 2 = 89%, chi-square = 46.38) and severe MR compared with moderate MR (RR 1.42, 95% CI 1.08 to 1.87, p = 0.01, I 2 = 67%, chi-square = 15.08).
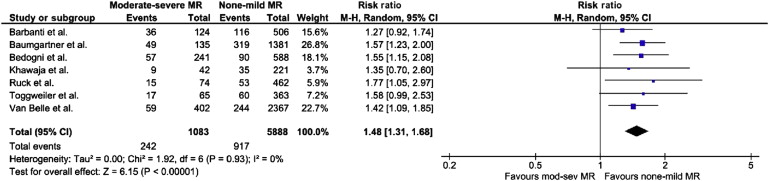
The severity of moderate-severe MR improved in 61 ± 6.0%, worsened in 3.0 ± 1.0%, and remained unchanged in 36.0 ± 4.0% of the patients. Seven studies including 6,971 patients (none-mild residual MR, n = 5,888; moderate-severe residual MR, n = 1,083) provided information on 1-year mortality, stratified according to the severity of residual MR after TAVI. The presence of moderate-severe residual MR after TAVI was associated with a statistically significant increase in 1-year mortality, compared with none-mild residual MR (RR 1.48, 95% CI 1.31 to 1.68, p <0.00001, I 2 = 0%, chi-square = 1.92; Figure 5 ).