The impact of a coronary revascularization strategy (early or deferred) on clinical outcomes of non–ST-segment elevation acute coronary syndrome (NSTE-ACS) has not been well established. The goal of this study was to systematically review randomized trials comparing early to deferred revascularization for NSTE-ACS. A systematic literature search of MEDLINE, ISI Web of Science, and Cochrane databases was conducted. Two reviewers independently determined the eligibility of clinical trials. Five trials with 4,155 patients were included for analysis. Meta-analysis showed that early revascularization produced no significant differences in the incidence of death (risk ratio [RR] 0.88, p = 0.47), recurrent myocardial infarction (RR 0.92, p = 0.58), and repeat revascularization compared to a deferred intervention. However, a significant decrease in refractory ischemia was observed in the early intervention group (RR 0.47, p <0.01), and the procedure also showed a tendency toward decreasing major bleeding events (RR 0.77, p = 0.08). According to stratification based on intervention era, extent of revascularization, and time of revascularization, subgroup analysis did not show between-group differences in all-cause mortality, recurrent myocardial infarction, and major bleeding events. Also, sensitivity analysis by alternatively using a random-effects model did not find any relevant influence on overall results in direction and magnitude. In conclusion, meta-analysis demonstrated that early coronary revascularization is feasible and safe for patients with NSTE-ACS, might markedly decrease the incidence of refractory ischemia, and appears to produce less bleeding.
Non–ST-segment elevation acute coronary syndrome (NSTE-ACS) is the most frequent manifestation of acute coronary syndrome and represents the largest group of patients undergoing coronary revascularization. However, optimal timing of coronary revascularization for patients with NSTE-ACS, i.e., immediately after admission or after pretreatment with optimal medical therapy, remains uncertain. The choice of time to coronary revascularization in patients with NSTE-ACS is an important clinical decision for its potential implication in hospital costs and clinical end points. It is an undeniable fact that an early coronary revascularization strategy shortens the length of in-hospital stay compared to a deferred strategy. However, the value of early versus deferred revascularization strategy in improving clinical outcomes of patients with NSTE-ACS has not been well established. To investigate the value of the 2 strategies in the management of NSTE-ACS we conducted this meta-analysis based on data from relevant randomized trials.
Methods
Relevant studies were identified through a computerized literature search of MEDLINE, ISI Web of Science, and Cochrane databases (Central Register of Controlled Trials and Cochrane Database of Systematic Reviews) through July 2010 using the search terms “early,” “routine,” “immediate,” “deferred,” “delayed,” “unstable angina,” “non–ST-segment elevation myocardial infarction,” “acute coronary syndrome,” “randomized,” and “human.” To ensure that no clinical trials were missed, we also conducted an extensive search of a citation database (ISI Web of Science) using cross references from eligible articles. No language restrictions were used.
Trials were included if they enrolled patients with a diagnosis of NSTE-ACS and randomly allocated patients to undergo early or deferred coronary revascularization. “Early” intervention was defined as coronary revascularization (percutaneous coronary intervention or coronary artery bypass grafting based on angiographic characteristics and physicians’ clinical judgment) soon after admission and randomization, and “deferred” intervention was defined as pretreatment using standard medical therapy and subsequent revascularization in later stages after enrollment. We excluded studies that compared invasive to conservative strategies or routine to selective intervention for patients with NSTE-ACS. Also, post hoc analysis of randomized trials was excluded from the analysis because of lack of a higher level of evidence. Two investigators (S.Z. and K.Y.) reviewed the literature and all citations in duplicate to identify potentially eligible studies and independently rejected or accepted each article based on the inclusion and exclusion criteria. Any disagreement was resolved by consensus between the 2 reviewers.
Two reviewers (S.Z. and K.Y.) independently extracted data on study characteristics including enrollment period, number of enrolled patients, patient demographics, risk factors for coronary artery disease, cardiac history, medical therapy, and interventions after randomization at baseline. Number of major clinical outcomes (e.g., all-cause death, recurrent myocardial infarction [MI], refractory ischemia, repeat intervention, and major bleeding events) was also extracted from each eligible trial. Reviewers resolved differences through consensus and the principal investigator (J.G.) resolved any disagreements. All eligible studies were assessed for the following quality criteria: randomization methods, blinding, and description of withdrawals and dropouts. Jadad quality scale, a numerical score from 0 to 5, was assigned to qualitatively assess the enrolled trials.
The Mantel-Haenszel method for fixed effects was used to investigate the combined results of individual studies. Risk ratios (RRs) with 95% confidence intervals (CIs) for all outcomes were computed as summary statistics. For studies with no event of interest in a treatment group, 1.0 was added to all cells for continuity correction. Heterogeneity across studies was quantified using the I 2 statistic with a scale of 0% to 100% (>75% represented very large between-study inconsistency). Data stratified according to intervention era, extent of revascularization, and absolute differences in intervention time were analyzed to investigate clinical factors affecting clinical outcomes. Sensitivity analyses were conducted to examine the robustness of the effect by alternatively using a random-effects model. We quantitatively assessed publication bias using the Begg adjusted-rank correlation test and Egger regression asymmetry test based on data on all-cause mortality and recurrent MI. Results were considered statistically significant at a p value <0.05. Analyses were performed with RevMan 5.0 (Cochrane Collaboration, Copenhagen, Denmark). The meta-analysis was prepared according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline.
Results
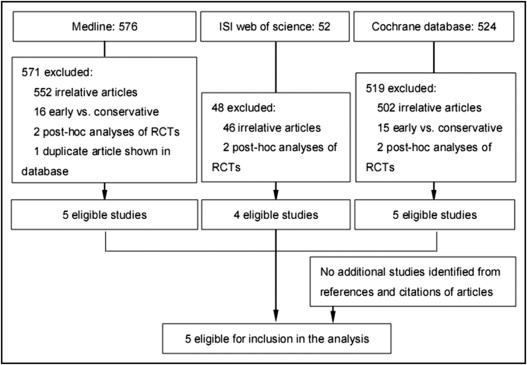
Detailed search steps are presented in Figure 1 . Briefly, from the initial literature search we identified 576 items in MEDLINE, 52 in ISI Web of Science, and 524 in the Cochrane database. After elaborative screening 5 studies were eligible for inclusion in analysis and no additional relevant study was identified from the references and citations of eligible articles.
In total 4,155 patients with NSTE-ACS in the 5 trials were included for analysis. Baseline demographics of patients in each study are presented in Table 1 . Of enrolled patients 2,153 were randomly allocated to undergo early intervention and 2,002 to deferred intervention. Most patients undergoing coronary revascularization received a percutaneous coronary intervention. Median time to revascularization ranged from 0.5 hour to 16 hours in the early intervention group and from 21.6 to 86 hours in the deferred intervention group if time 0 was defined as the time of randomization. Follow-up ranged from 30 days (all enrolled trials) to 6 months (The Immediate Versus Deferred Coronary Angioplasty In Non-ST-Segment Elevation Acute Coronary Syndromes [OPTIMA] trial and The Timing of Intervention in Acute Coronary Syndromes [TIMACS] trial ). Mean age of patients in the enrolled trials was consistently >60 years and participants were mostly men. In addition, almost all patients received contemporary evidence-based therapy such as aspirin, thienopyridine, anticoagulant, β blocker, and statins. The level of evidence for each article was graded with a score of 3 to 5 according to the Jadad quality score (see supplemental data ).
| Characteristics | ABOARD | TIMACS | OPTIMA | ISAR-COOL | ELISA |
|---|---|---|---|---|---|
| Enrollment period | 2006–2008 | 2003–2008 | 2004–2007 | 2000–2002 | 2000–2001 |
| Patients ⁎ | 175/177 | 1,593/1,438 | 73/69 | 203/207 | 109/111 |
| Age (years) | 65 | 65 | 62 | 70 † | 63 |
| Women | 28% | 35% | 32% | 33% | 30% |
| Smoking | 33% | NA | 38% | 21% | 35% |
| Diabetes mellitus | 27% | 27% | 20% | 29% | 14% |
| Previous myocardial infarction | 18% | 20% | 23% | 24% | 15% |
| Increased cardiac biomarker | 74% | 77% | 46% | 67% | 68% |
| Previous percutaneous coronary intervention | 27% | 14% | 23% | 22% | 14% |
| Previous coronary artery bypass grafting | 6% | 7% | 6% | 11% | 9% |
| Treatment during hospitalization | |||||
| Aspirin | 100% | 98% | 99% | 100% | 100% |
| Thienopyridine | 98% | 87% | 100% | 100% | 100% |
| Glycoprotein IIb/IIIa inhibitors | 61% | 23% | 95% | 100% | 50% |
| Anticoagulant | 98% | 97% | 95% | 100% | 100% |
| β Blocker | 86% | 87% | 96% | 95% | 100% |
| Statin | 95% | 85% | 97% | 85% | NA |
| Interventions after randomization | |||||
| Coronary angiography ⁎ | 83.4%/85.3% | 97.6%/95.7% | 100%/100% | 100%/100% | 99%/100% |
| Median time (hours) ⁎ | 1.2/21 | 14/50 | 0.5/25 | 2.4/86 | 6/50 |
| Percutaneous coronary intervention ⁎ | 80.1%/69.5% | 59.6%/55.1% | 100%/99% | 70.4%/64.3% | 61.0%/58.0% |
| Median time (hours) ⁎ | 1.9/21.6 | 16/52 | 0.5/25 | 2.4/86 | 6/50 |
| Time differences (hours) ‡ | 19.7 | 36 | 24.5 | 83.6 | 44 |
| Overall percutaneous coronary intervention or coronary artery bypass grafting ⁎ | 91.1%/80.8% | 74.4%/68.7% | 100%/99% | 78.3%/72.0% | 75.0%/77.0% |
| Relative difference in rate of revascularization § | 12.7% | 8.3% | 1.0% | 8.8% | −2.6% |
⁎ Expressed as early intervention group/deferred intervention group.
‡ (Early revascularization rate minus deferred revascularization rate)/deferred revascularization rate.
§ Time from randomization to revascularization in early intervention group minus that in deferred intervention group.
Of the 5 enrolled trials 2 were conducted in the era of bare-metal stents (before 2003) and 3 in the drug-eluting stent era. There were 2 studies (The Angioplasty to Blunt the Rise of Troponin in Acute Coronary Syndromes Randomized for an Immediate or Delayed Intervention [ABOARD] trial and OPTIMA ) with a relatively small difference in time to catheterization between the 2 strategies (19.7 and 24.5 hours), 2 trials (TIMACS and Early or Late Intervention in unStable Angina [ELISA] pilot study ) with an intermediate time difference (36 and 44 hours), and 1 study (The Intracoronary Stenting With Antithrombotic Regimen Cooling-Off [ISAR-COOL] trial ) with a relatively large time difference (83.6 hours; Table 1 ). In addition, 2 studies (OPTIMA and ELISA ) had a low relative difference in the use of revascularization between the 2 groups (−2.6% and 1%), and the other 3 had a high relative difference (8.3%, 8.8%, and 12.7%, respectively; Table 1 ).
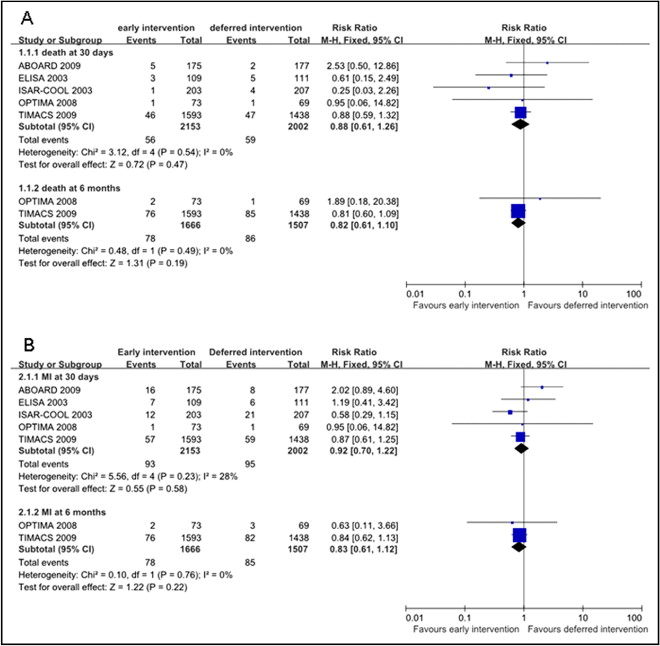
Meta-analytic pooling for 30-day and 6-month all-cause mortality showed that early revascularization did not provide a greater survival advantage compared to a deferred intervention (RR 0.88, p = 0.47; RR 0.82, p = 0.19, respectively; Figure 2 ) . There was no evidence for heterogeneity among the enrolled trials (I 2 = 0%). Moreover, subgroup analysis demonstrated that intervention era and extent of revascularization had no effect on the survival of patients with NSTE-ACS ( Figure 3 ) . When analysis was restricted to absolute differences in intervention time between the 2 treatment arms, RRs for all-cause mortality were 2.48 (95% CI 0.49 to 12.66) in the low time difference subgroup, 0.86 (95% CI 0.58 to 1.26) in the moderate time difference subgroup, and 0.15 (95% CI 0.01 to 2.80) in high time difference subgroup, with no statistical significances ( Figure 3 ).