Takotsubo cardiomyopathy (TTC) is characterized by reversible left ventricular (LV) systolic dysfunction independent of fixed coronary disease or coronary spastic pathogenesis. A number of investigators have documented marked elevation of natriuretic peptide levels at presentation in such patients. We sought to determine the pattern, extent, and determinants of the release of N-terminal pro-B type natriuretic peptide/B type natriuretic peptide (NT-proBNP/BNP) in patients with TTC. We evaluated NT-proBNP/BNP release acutely and during the first 3 months in 56 patients with TTC (96% women, mean age 69 ± 11 years). The peak plasma NT-proBNP levels were compared to the pulmonary capillary wedge pressure and measures of regional and global LV systolic dysfunction (systolic wall stress, wall motion score index, and LV ejection fraction) as potential determinants of NT-proBNP/BNP release. In patients with TTC, the plasma concentrations of NT-proBNP (median 4,382 pg/ml, interquartile range 2,440 to 9,019) and BNP (median 617 pg/ml, interquartile range 426 to 1,026) were substantially elevated and increased significantly during the first 24 hours after the onset of symptoms (p = 0.001), with slow and incomplete resolution during the 3 months thereafter. The peak NT-proBNP levels exhibited no significant correlation with either pulmonary capillary wedge pressure or systolic wall stress. However, the peak NT-proBNP level correlated significantly with the simultaneous plasma normetanephrine concentrations (r = 0.53, p = 0.001) and the extent of impairment of LV systolic function, as measured by the wall motion score index (r = 0.37, p = 0.008) and LV ejection fraction (r = −0.39, p = 0.008). In conclusion, TTC is associated with marked and persistent elevation of NT-proBNP/BNP levels, which correlated with both the extent of catecholamine increase and the severity of LV systolic dysfunction.
Patients with takotsubo cardiomyopathy (TTC) not infrequently have low cardiac output status at the initial presentation, but this does not always reflect associated pulmonary edema. A number of investigations have reported that at diagnosis, the plasma levels of B-type natriuretic peptide (BNP) or its precursor N-terminal proBNP (NT-proBNP) are markedly elevated in major cases. The reported increases in NT-proBNP/BNP levels in patients with TTC are surprising, given that the left ventricular (LV) filling pressure is not markedly elevated. The objective of the present study was to determine the basis for the elevation of natriuretic peptide levels in TTC, using predominantly NT-proBNP as a marker because of its longer half-life in plasma. In particular, we prospectively sought to determine whether NT-proBNP release correlated with the extent of acute catecholamine release, systemic inflammatory activation, and global/regional systolic dysfunction and pulmonary congestion.
Methods
Consecutive patients with TTC were prospectively identified according to the proposed Mayo Clinic criteria : (1) transient periapical or midventricular akinesia/hypokinesis, (2) no evidence for coronary artery disease or acute plaque rupture on the coronary angiogram, and (3) new ST/T wave changes and/or biomarker elevation.
To establish the baseline characteristics of the study group, the patients’ history and clinical profiles were evaluated by interviewing all patients and reviewing the hospital and physician records. This information included the preadmission likelihood of coronary artery disease, medical history, cardiac risk factors, clinical symptoms, and recent stress events. The hemoglobin level and estimated glomerular filtration rate at admission were also reported. The institutional ethics of human research committee approved the study, and all patients provided written informed consent before study entry.
Venous blood specimens were collected into tubes containing potassium ethylene diamine tetra acetic acid at diagnosis and daily thereafter for 3 days. The determination of plasma NT-proBNP and BNP was performed using an immunoassay (Elecsys E 170, Roche Diagnostics, Mannheim, Germany, and AxSYM, Abbott Laboratories, Illinois, respectively). The NT-proBNP level was assayed within 2 hours after venesection. For the BNP assay, the blood was centrifuged at 1,680 relative centrifugal force for 10 minutes at 2°C, and frozen plasma was stored at −80°C until analysis. In 31 patients, who presented within 12 hours of symptom onset, the NT-proBNP assay was performed at presentation and 12 hours thereafter to determine the pattern of early NT-proBNP release. The NT-proBNP and BNP assays were repeated at 10 days and 3 months after the diagnosis.
The plasma concentrations of normetanephrine, a nonacidic derivative of norepinephrine reflecting extraneuronal uptake and O- methylation, were measured as an index of catecholamine exposure in TTC. The venous blood at diagnosis was drawn into tubes containing ethylene diamine tetra acetic acid and centrifuged at 1680 relative centrifugal force for storage at −80°C for subsequent assay of normetanephrine using liquid chromatography/tandem mass spectrometry.
Additional serial routine biochemical investigations, including assays of troponin T and creatine kinase (Elecsys, Roche Diagnostics) were performed at admission and daily thereafter. Serial (daily) determination of plasma C-reactive protein concentrations was performed using a latex-enhanced immunoturbidometric assay (Elecsys 1010, Roche Diagnostics). All C-reactive protein results of <10 mg/L were then subjected to high-sensitivity C-reactive protein (Olympus au5400, Dallas, Texas) determination.
The diagnosis of TTC was established by cardiac catheterization and coronary angiography in all patients. At cardiac catheterization, the pulmonary capillary wedge pressure (PCWP) was determined using right heart catheterization in 34 patients for correlation with NT-proBNP release.
Echocardiography was performed in all patients acutely and after 10 days and 3 months. Standard views were obtained using a General Electric Vivid 7 echocardiography system (GE Medical Systems, Milwaukee, Wisconsin). Off-line analysis used Simpson’s biplane method for the estimation of LV ejection fraction, according to the guidelines set by the American Society of Echocardiocardiography. Wall motion was analyzed according to a 17-segment model by a cardiologist. The thickening and excursion of each segment was described and scored as previously described (normal, 1; hypokinesis, 2; akinesia, 3; and dyskinesis, 4). The wall motion score index was prospectively selected as an appropriate measure of the extent of regional wall motion impairment, given that LV ejection fraction would be influenced by segments exhibiting compensatory hyperfunction.
Cardiovascular magnetic resonance (CMR) imaging, performed acutely in 42 patients, was used primarily to calculate the regional left ventricular wall stress. Of the 56 patients, 14 were excluded because of an unwillingness to participate (n = 2), severe concomitant illness (n = 2), or a contraindication to CMR (n = 10). CMR was performed using a 1.5 Tesla Philips Intera Magnet (Philips Medical System, Best, The Netherlands). Late gadolinium enhancement CMR was performed 10 to 15 minutes after intravenous injection of 0.2 mmol/kg gadolinium-diethylennetriamine pentaacetic acid (Magnevist, Schering AG, Berlin-Wedding, Germany). Short-axis images of the left ventricle (8-mm slice thickness) were obtained, using SENSitivity Encoding (SENSE). Regional systolic wall stress (σ) was calculated at the basal (σ BASE ), midventricular (σ MID ), and apical (σ APEX ) levels, using the LaPlace-derived formula of Grossman et al, as adapted for use in CMR by Delépine et al. The average end-systolic internal radius, with the corresponding average radial thickness of the myocardial wall, was determined using off-line-analysis of CMR images, with the end-systolic frame defined by atrioventricular closure on a LV outflow tract view. Noninvasive systolic blood pressure measurements were incorporated. The LV basal (σ BASE ) and midventricular (σ MID ) wall stress was determined from short-axis images, and the apical wall stress (σ APEX ) was determined using measurements from the corresponding long-axis views, given that σ APEX is known to be underestimated when the wall thickness is determined from short-axis slices, a consequence of tangential slicing resulting from the increased radius of the wall curvature at the LV apex.
The data were analyzed using the Statistical Package for Social Science software, version 15 (SPSS, Chicago, Illinois) and presented as the mean ± SD for normally distributed data or the median and interquartile range for skewed data. The correlations between the NT-proBNP levels and PCWP, regional systolic wall stress, and wall motion score index were assessed using Spearman’s correlation analysis. A value of p <0.05 was considered significant.
Results
The clinical characteristics of the study population are listed in Table 1 . A total of 56 patients (54 women and 2 men) were diagnosed with TTC at 3 tertiary hospitals from September 2007 to December 2010. Only 6% of patients with TTC had been treated with β-adrenoreceptor antagonists before the diagnosis. Although the regional wall motion was significantly impaired in all patients at admission, the baseline LV ejection fraction was mildly reduced, improving significantly after 10 days (53 ± 13% vs 62 ± 10%, respectively, p = 0.005).
| Variable | TTC (n = 56) |
|---|---|
| Clinical characteristics | |
| Age (years) | |
| Mean ± SD | 69 ± 11 |
| Range | 41–93 |
| Body mass index (kg/m 2 ) | 28 ± 7 |
| Previous/current smoking | 18% |
| Systemic hypertension | 58% |
| Diabetes mellitus | 20% |
| Hyperlipidemia | 44% |
| Clinical presentation | |
| Potential acute stress | 81% |
| Chest pain | 98% |
| Dyspnea | 5% |
| ST-segment elevation on electrocardiogram | 36% |
| Laboratory findings | |
| Troponin T (mg/dl) | |
| Median | 0.32 |
| Interquartile range | 0.2–0.55 |
| Creatine kinase (IU/L) | |
| Median | 173 |
| Interquartile range | 109–245 |
| C-reactive protein/high-sensitivity C-reactive protein (mg/L) | |
| Median | 15 |
| Interquartile range | 5–41 |
| Renal dysfunction (glomerular filtration rate <60 ml/min) | 22.0% |
| Hemoglobin level (g/L) | 131 ± 16 |
⁎ Coronary risk factors, clinical presentation, routine laboratory assessment.
Of the 20 patients with TTC exhibiting initial ST-segment elevation, the diagnosis was made on day 1, during urgent catheterization, for all but 1 patient. Two patients were initially hypotensive. One died on day 7 from multiorgan failure. The median PCWP was 15 ± 7 mm Hg. Seven patients had a PCWP of ≥17 mm Hg, with a maximum of 36 mm Hg. All patients in the TTC group had troponin T elevations beyond the normal range for the laboratory, and 53% had creatine kinase elevations.
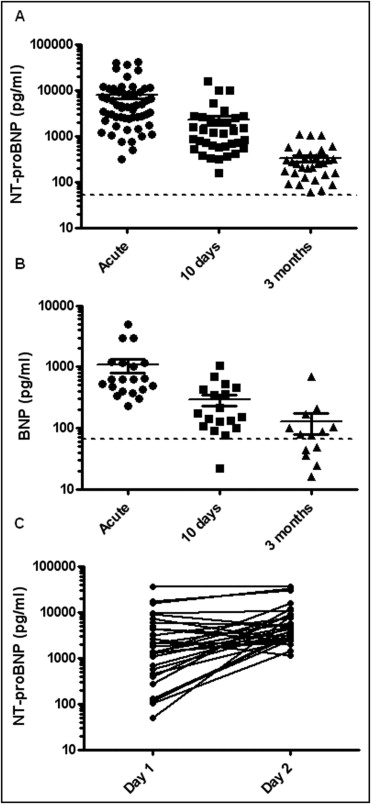
The NT-proBNP and BNP concentrations were markedly elevated beyond the population norms at diagnosis, with progressive resolution within 3 months ( Figure 1 ) . At 10 days, both NT-proBNP and BNP were still elevated beyond the age-corrected norms in all patients. At 3 months, there was residual, but borderline elevation. The peak NT-proBNP level (median 4,382 pg/ml, interquartile range 2,440 to 9,019) and BNP level (median 617 pg/ml, interquartile range 426 to 1,026) were closely correlated (r = 0.70, p = 0.0008). In patients presenting within 24 hours of symptom onset (n = 31), the median NT-proBNP level was 1,325 pg/ml (interquartile range 448 to 4,284) at presentation, with peak concentrations attained at day 2 (median 4,382 pg/ml, interquartile range 2,529 to 8,200, p = 0.001; Figure 1 ).
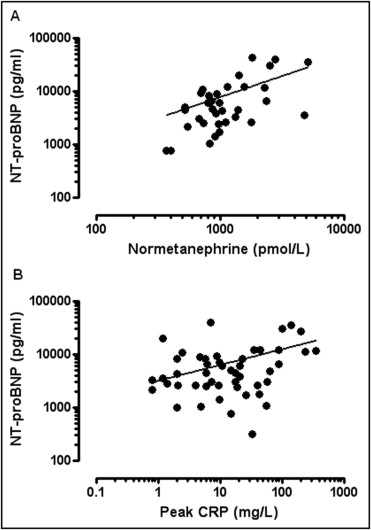
The median plasma normetanephrine concentration was 998 pmol/L (range 547 to 1,144). A close direct correlation (r = 0.53, p = 0.001) was found between the plasma normetanephrine concentrations at diagnosis and the peak NT-proBNP concentrations ( Figure 2 ) . The plasma concentrations of the peak (high-sensitivity) C-reactive protein were directly, but weakly, correlated with the peak NT-proBNP levels (r = 0.3, p = 0.05). Furthermore, a trend (r = 0.22, p = 0.08) was seen toward a correlation between the peak creatine kinase and peak NT-proBNP levels.