Fractional flow reserve (FFR) has been proposed as the gold standard to assess functional severity of coronary artery stenosis and to stratify which lesions should be subjected to intervention (percutaneous coronary intervention [PCI]). A systematic review was performed in MEDLINE and EMBASE including studies indexed until November 2013 that used FFR for deferral or performance of PCI. Outcomes of interest were death, acute myocardial infarction (AMI), and new revascularization (RV). Nineteen studies were included, totaling 3,097 patients (3,796 lesions). Mean follow-up was 21.2 months. In indirect comparisons, FFR-PCI and FFR-defer groups had similar death (2.2% vs 2.0%, respectively, p = 0.86) and AMI rates (1.9% vs 1.9%, respectively, p = 1.00). RV rates were higher in the FFR-PCI group (14.0% vs 4.4%, p = 0.002). Direct comparisons (2-arm trials) also showed no differences in death (odds ratio [OR] 1.86 [95% CI 0.81 to 4.27], I 2 = 11.5, p = 0.14) and AMI rates (OR 0.75 [95% CI 0.21 to 2.69], I 2 = 47.1, p = 0.66); RV rates were again higher in the FFR-PCI (OR 3.10 [95% CI 1.25 to 7.70], I 2 = 72.2, p = 0.015). Meta-regression suggests influence of male gender on RV rates (β = 0.058, p = 0.026). In conclusion, deferral of PCI based on FFR is a safe strategy. Considerable heterogeneity was observed, however.
In the past decades, the invasive physiological assessment by means of fractional flow reserve (FFR)—a concept that was first introduced by Pijls et al, as a method to describe maximum achievable blood flow to the myocardium supplied by a stenotic artery in terms of coronary pressure measurement—has gained ground as an important complementary tool in the catheterization laboratory. Its ability to overcome the limitations of angiography in defining the significance of lesions eligible for percutaneous coronary intervention (PCI) has been subject of intensive investigation. Published evidence suggests that the method is feasible and reproducible and seems to be a safe and cost-effective strategy for deferral of PCI. In general, patients in whom PCI is deferred based on a negative FFR seem to have similar long-term outcomes compared with the ones undergoing PCI after a positive test result, and FFR-guided intervention apparently reduces the number of stented lesions, procedure costs, and the rates of hard clinical outcomes compared with angiography-guided revascularization (RV). This investigation was designed as a systematic review and meta-analysis of studies evaluating deferral or performance of PCIs based on FFR results, considering as outcomes of interest death, acute myocardial infarction (AMI), and repeated RV, to assess the clinical applicability of this method for decision making in the catheterization laboratory.
Methods
This work follows PRISMA statement for systematic reviews and is in accordance to specific guidelines for nonrandomized studies. Initially, a search in the main databases (MEDLINE, SciELO, EMBASE, Cochrane) was performed, searching for studies with similar objectives and methodology. No similar study was found.
A systematic search was performed in MEDLINE and Embase databases with the merged MeSH terms (“fractional flow reserve” AND “intervention”), (“fractional flow reserve” AND “angioplasty”), and (“fractional flow reserve” AND “PCI”), looking for studies, published until November 2013, that used FFR measurement to determine in which non–left main lesions PCI should be performed or deferred. Bibliographic citations from hand search of texts and from the MEDLINE “related articles” section and e-mail contact with investigators were allowed.
Study selection criteria were as follows: (1) observational or comparative studies (randomized or not) evaluating patients in whom PCI was performed or deferred based on FFR results; (2) FFR performed with standardized and well-described methodology; (3) vasodilator adequately described; (4) FFR cutoff of 0.75 or 0.80; (5) clinical, demographic, angiographic, and FFR data systematically reported; (6) interventional techniques reported; and (7) complete follow-up (FU) data and losses reported.
The titles returned were peer reviewed by 2 researchers (AFLB and FACM), according to the previously established criteria. Exclusion by title, abstract, and full-text analyses was independently performed, and discrepancies in each stage were solved by consensus after discussion with a senior author. The selected studies were read in full to confirm eligibility, and their data were tabulated and reviewed for statistical analysis. The second researcher independently double-checked the data extraction. The AMI rates were tabulated according to the study definition, as well as the RV rates (target vessel, target lesion, or any new RV).
Study quality was assessed by 2 authors (AFLB and GTRP) using the Newcastle-Ottawa Scale (NOS), a method for assessing the quality of nonrandomized studies (case-control studies, cohort studies, and time interrupted series). The 2 randomized-controlled trials (RCTs) were evaluated by the Jadad scale.
Data analysis was performed using Comprehensive Meta Analysis Software, version 2.2.048 (Biostat Inc., Englewood, New Jersey). Publication bias was evaluated through funnel plot and Egger’s test. Heterogeneity was explored with I 2 estimate (inconsistency measure) from Cochran Q , which describes the percentage of variability of the effect that is due to heterogeneity rather than chance. Given the small number of RCTs and to overcome the risk of bias of direct comparison of studies with nonsimilar arms, the results were pooled by random-effects model for the outcomes and indirect comparisons were performed between 2 subgroups of arms: FFR-PCI and FFR-defer. The pooled results were compared by the random-effects analysis assuming the study-to-study variance (τ 2 ) to be the same for both subgroups. These values are computed within subgroups, and the difference between subgroups was considered statistically significant if p <0.05 in the comparison of effect between FFR-PCI and FFR-defer.
To confirm the results, sensitivity analyses were done. Analyses by meta-regression (unrestricted maximum likelihood) or by subgroups were done when possible, to explore heterogeneity sources. A separate subgroup analysis with direct and indirect comparisons for studies with 2 arms was performed, and the point estimates were reported for 1-arm studies separately. To evaluate the possible impact of low-quality studies, we also did sensitivity analysis by exclusion of studies with NOS less than 7 stars. Additional analysis excluding studies with FFR cutoff of 0.80 and excluding the 2 RCTs was also done.
Results
Twenty-one articles remained for full-text reading after exclusions, and 19 remained for final analysis (2 RCTs and 17 observational studies, published from 1996 to 2013; Figure 1 ). Among these, 9 were 2-arm studies and 10 evaluated cohorts of only FFR-defer arms, totaling 9 FFR-PCI and 19 FFR-defer arms. In 1 trial, we included the FFR-defer arm (≥0.75) and the reference FFR-perform registry (<0.75), and in another one, we included the FFR-perform (<0.80) and the reference FFR-defer (≥0.80) registries ( Table 1 ).

| Paper | RCT | Strategy | N / lesions | Sex (% male) | Age (mean) | HTN / DM / Smoker (N) | FU (months) | FFR cut-off | Vasodilator | Death / AMI / RV (N) | Score (NOS / Jadad) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bech et al. 2001 | + | PCI | 144 / 144 | 86.1 | 60 | 42 / 13 / 29 | 12 | 0.75 | IC/IV adenosine | 0 / 0 / 0 | 9 / 3 ∗ | ||
| Defer | 91 / 91 | 61.5 | 61 | 36 / 25 / 27 | 0 / 9 / 1 | ||||||||
| Costa et al. 2007 | 0 | PCI | 21 / 39 | NP | 62.4 | NP | 12 | 0.75 | IV adenosine | 0 / 0 / 5 | 6 | ||
| Defer | 21 / 39 | NP | 62.4 | NP | 0 / 0 / 1 | ||||||||
| De Bruyne et al. 2012 | + | PCI | 447 / 890 | 79.6 | 63.5 | 347 / 123 / 89 | 7.1 | 0.80 | IV adenosine | 1 / 15 / 14 | 9 / 5 ∗ | ||
| Defer | 166 / 241 | 68.1 | 63.6 | 136 / 42 / 35 | 6.9 | 0 / 3 / 6 | |||||||
| Hirota et al. 2006 | 0 | PCI | 46 / 73 | 84.8 | 65.0 | 27 / 19 / 23 | 17.5 | 0.75 | IV adenosine | 0 / 0 / 9 | 8 | ||
| Defer | 26 / 26 | 84.6 | 64.7 | 14 / 15 / 19 | 0 / 0 / 2 | ||||||||
| Kobori et al. 2005 | 0 | PCI | 34 / 34 | 85.3 | 64 | 17 / 13 / 21 | 25 | 0.75 | IC papaverine | 1 / 0 / 3 | 8 | ||
| Defer | 113 / 121 | 76.1 | 62 | 70 / 34 / 67 | 0 / 0 / 1 | ||||||||
| Legalery et al. 2005 | 0 | PCI | 136 / 136 | 66.9 | 58 | 69 / 33 / 90 | 12 | 0.80 | IC adenosine | 1 / 1 / 20 | 9 | ||
| Defer | 271 / 271 | 69.0 | 60 | 121 / 69 / 161 | 5 / 4 / 28 | ||||||||
| Misaka et al. 2011 | 0 | PCI | 15 / 17 | 86.7 | 65.5 | 11 / 5 / 5 | 53 | 0.75 | IC papaverine | 0 / 0 / 2 | 9 | ||
| Defer | 29 / 33 | 75.9 | 66.4 | 22 / 15 / 14 | 0 / 1 / 1 | ||||||||
| Muller et al. 2011 | 0 | PCI | 144 / 144 | NP | 67.4 | NP | 40 | 0.80 | IC/IV adenosine | 16 / 2 / 26 | 9 | ||
| Defer | 564 / 564 | 55.0 | 68.7 | 285 / 95 / 199 | 30 / 2 / 11 | ||||||||
| Reczuch et al. 2004 | 0 | PCI | 7 / 8 | NP | 60 | NP | 15 | 0.75 | IV adenosine | 0 / 0 / 1 | 6 | ||
| Defer | 9 / 26 | NP | 60 | NP | 0 / 1 / 0 | ||||||||
| One arm studies / One arm included | |||||||||||||
| Bech et al. 1998 | 0 | Defer | 100 / 100 | 69.0 | 61 | 37 / 17 / 39 | 18 | 0.75 | IC/IV adenosine | 0 / 1 / 3 | 7 | ||
| Costa-Dias et al. 2004 | 0 | Defer | 21 / 21 | 66.7 | 66.4 | 13 / 3 / 4 | 19 | 0.75 | IC adenosine | 0 / 0 / 0 | 7 | ||
| Dominguez-Franco et al. 2008 | 0 | Defer | 136 / 144 | 80.9 | 62 | 56 / 40 / 65 | 30 | 0.75 | IC adenosine | 10 / 3 / 15 | 7 | ||
| Mates et al. 2004 | 0 | Defer | 50 / 62 | 66.0 | 60.8 | NP | 15.4 | 0.75 | IC/IV adenosine | 2 / 0 / 2 | 7 | ||
| Mates et al. 2005 | 0 | Defer | 85 / 111 | 63.5 | 61 | 57 / 26 / 31 | 22.5 | 0.75 | IC/IV adenosine | 2 / 1 / 3 | 7 | ||
| Ozdemir et al. 2002 | 0 | Defer | 51 / 58 | 74.5 | 54.4 | 21 / 8 / NP | 16.6 | 0.75 | IC adenosine | 0 / 0 / 3 | 6 | ||
| Pereira et al. 2013 | 0 | Defer | 231 / 300 | 68.4 | 65 | 187 / 68 / 37 | 21.2 | 0.80 | IC/IV adenosine | 1 / 2 / 14 | 7 | ||
| Pijls et al. 1996 | 0 | Defer | 24 / 24 | 54.2 | 55 | NP | 14.0 | 0.75 | IV adenosine | 0 / 0 / 0 | 8 | ||
| Reczuch et al. 2005 | 0 | Defer | 41 / 41 | 80.9 | 62 | NP | 15.0 | 0.75 | IV adenosine | 0 / 1 / 2 | 6 | ||
| Rieber et al. 2007 | 0 | Defer | 56 / 56 | 71.4 | 66 | 38 / 13 / 5 | 24.0 | 0.75 | IC adenosine | 0 / 0 / 5 | 7 | ||
A total of 3,097 patients and 3,796 lesions were considered for analysis; the weighted mean age was 63.6 years, 70% were men, 58% had hypertension, 24% had diabetes mellitus , and 35% were smokers. The mean FU time was 21.2 months (6.9 to 53). FFR methodology was similar among the studies. Detailed characteristics of the included studies are provided in Table 1 . Study quality analysis showed that in general, studies were representative for the population in question, with mean 7.5 stars in the NOS scale (6 to 9 stars). Jadad score was 3 and 5 for the 2 RCTs. Methodologically, the most important risk of bias detected was the direct comparison made in 7 studies that presented their data as nonrandomized direct comparison.
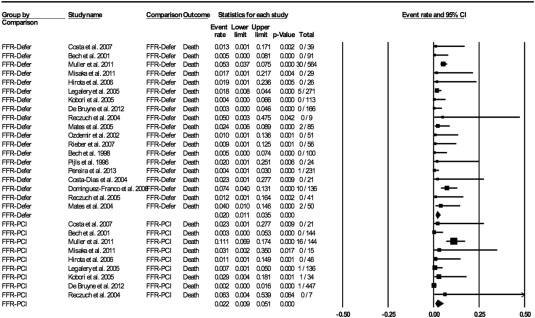
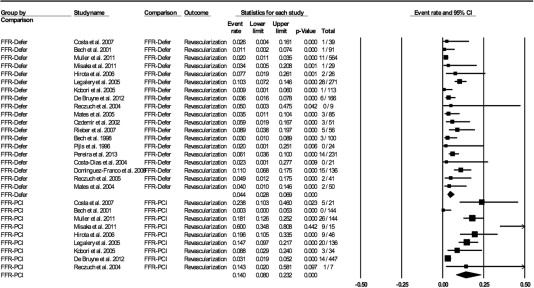
There were 110 death events reported in 10 arms, 84 AMI events in 14 arms, and 196 RV events in 24 arms. In indirect comparisons, the pooled rates of death were similar in FFR-PCI and FFR-defer arms (2.2%, 95% confidence interval [95% CI] 0.9% to 5.1%, I 2 = 72.7 vs 2.0%, 95% CI 1.1% to 3.5%, I 2 = 40.5, respectively, p = 0.86; Figure 2 ). The AMI rates were also similar (1.9% [95% CI 0.8% to 4.0%], I 2 = 0 vs 1.9% [95% CI 1.1% to 3.1%], I 2 = 49.8, p = 1.00). The repeated RV rates, however, were significantly higher in the FFR-PCI arms (14.0% [95% CI 8.0% to 23.2%], I 2 = 87.8 vs 4.4% [95% CI 8.8% to 6.9%], I 2 = 58.9, p = 0.002; Figure 3 ).
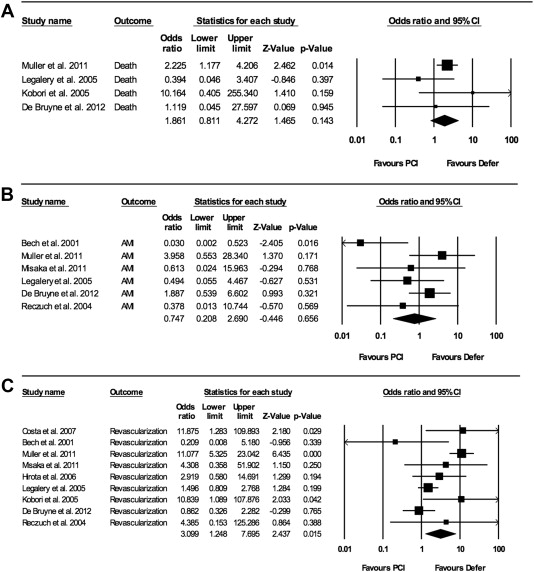
Even considering the risk of bias of nonrandomized direct comparisons, we performed this additional analysis for 2-arm trials. The findings were similar ( Figure 4 ), with no differences between FFR-PCI and FFR-defer for death (4 studies, odds ratio [OR] 1.86 [95% CI 0.81 to 4.27], I 2 = 11.5, p = 0.14) and AMI (6 studies, OR 0.75 [95% CI 0.21 to 2.69], I 2 = 47.1, p = 0.66). Higher RV rates (9 studies) were again observed in the FFR-PCI group (OR 3.10 [95% CI 1.25 to 7.70], I 2 = 72.2, p = 0.015).
Meta-regression suggests the influence of gender (percent men) on RV rates (β = 0.058, p = 0.026). No other cofactors (age, hypertension, diabetes, smoking, involvement of the left anterior descending artery) influenced the outcomes ( Table 2 ).



