Although the clinical relevance of aneurysm of the membranous ventricular septum (AMVS) in adults is unclear, the frequency of AMVS detection has been increased because cardiac multidetector computed tomography has been widely adopted for the evaluation of coronary artery disease. Therefore, we aimed to assess the clinical significance of AMVS in a longitudinal study. In 30,120 adults with suspected coronary artery disease who underwent cardiac multidetector computed tomography in 3 hospitals, 52 patients with AMVS were retrospectively selected. We evaluated the clinical symptoms and electrocardiographic abnormalities (cross-sectional study) and the prevalence of embolic stroke (observational study) during a median 40-month (range 6 to 74 months) observation period. For the assessment of embolic stroke, we excluded 9 patients with other explainable embolic sources. Conduction abnormalities were noted in 13 of 52 adults (25%) with AMVS on electrocardiography and embolic stroke occurred in 6 of 43 patients (14%). The mean age and the prevalence of hypertension were significantly higher in the embolic stroke group than in the event-free group (p <0.05). Thrombi were detected in the 11.6% of AMVS, which was significantly related with embolic stroke (p <0.05). The size and morphology did not change in 15 patients with serial follow-up images. In conclusion, our study suggests that AMVS in adults should not be ignored because AMVS may be related to conduction abnormality or embolic stroke, and it does not spontaneously resolve or diminish in size.
The clinical relevance of an incidentally detected aneurysm of the membranous ventricular septum (AMVS) in adults is unclear. Although most patients with AMVS are asymptomatic, various complications including cerebral embolism, cardiac arrhythmias, right ventricular outflow tract obstruction, bacterial endocarditis, and rupture may occur. AMVS-related cerebral stroke has been documented in several reports. However, to date, no study has been reported regarding the incidence of AMVS-related embolic events or the natural course of AMVS in adults. Therefore, our aim was to evaluate the clinical significance of incidentally detected AMVS in adults with cardiac multidetector computed tomography (MDCT) in a longitudinal study.
Methods
A database of electrocardiography (ECG)-gated cardiac MDCT from 3 tertiary general hospitals (Seoul National University Bundang Hospital, Seoul National University Hospital, and Asan Medical Center in Korea) was used for collection of study subjects. In 30,120 adults who underwent cardiac MDCT for the evaluation of coronary artery disease (CAD) from January 2007 to June 2012, we selected 52 adults (29 women; mean age, 54.0 ± 14.2 years) with incidentally detected AMVS using the key words of “ventricular septal aneurysm,” and “aneurysm of membranous interventricular septum” or combination words of “ventricular septum,” “membranous septum,” “aneurysm,” or “outpouching sac” and observed these patients for evaluation of clinical significance during the mean of 40 months. AMVS was defined as an outpouching sac protruding into the right ventricle, located near the membranous portion of the ventricular septum. We evaluated basic demographic data, risk factors, clinical symptoms, and ECG findings in all subjects.
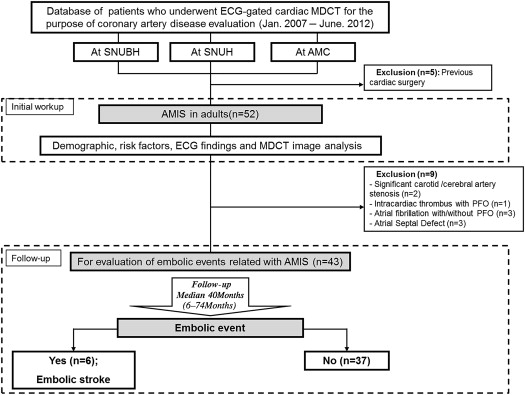
During the median 40-month observation period (range 6 to 74 months) for the evaluation of the direct relation between AMVS and embolic stroke, we excluded 9 patients who had other explainable causes for stroke as follows: significant carotid or cerebral artery atherosclerosis (n = 2), other potential cardiogenic embolic sources, such as intraventricular thrombus (n = 1) and atrial fibrillation (n = 3), or paradoxical embolic source such as atrial septal defect (n = 3). Among them, 3 patients have combined patent foramen ovale (PFO). PFO was usually diagnosed using echocardiography with intravenous agitated saline injection and Valsalva maneuver. However, in the patients without transthoracic echocardiography (TTE) examination, a channel-like appearance in the interatrial septum with shunt on cardiac MDCT was considered as PFO. Therefore, 43 patients (24 women; mean age, 52.5 ± 14.5 years) were finally longitudinally observed for the occurrence of embolic events. The study flow chart is summarized in Figure 1 .
CT examinations were performed using 64-multidetector CT (Brilliance 64; Philips Medical Systems, Best, The Netherlands) with 64 × 0.625-mm slice collimation, 420-ms gantry rotation time, and 120-kVp tube voltage; dual-source MDCT (Somatom Definition; Siemens Medical Solutions, Forchheim, Germany) with 2 × 32 × 0.6-mm slice collimation, 330-ms gantry rotation time, and 100- to 120-kVp tube voltage; or 256-multidetector CT (Brilliance iCT; Philips Medical Systems, Eindhoven, Netherlands) with 128 × 0.625-mm detector collimation, 270-ms gantry rotation time, and 100- to 120-kVp tube voltage, according to body mass index. ECG-based tube current modulation was performed in all patients. As routine practice, the CT data were processed using 3-dimensional software (Rapidia; INFINITT, Seoul, Korea), and multiple reformations including the short-axis (SA), 2-chamber, and 4-chamber images were generated.
Raw cardiac MDCT image data sets of the subjects who had incidentally detected AMVS with MDCT from each institution were sent to a core laboratory for analysis. MDCT images were reviewed independently by 2 experienced cardiovascular radiologists using a workstation with specialized software (TeraRecon Inc., San Mateo, California) blinded to clinical information.
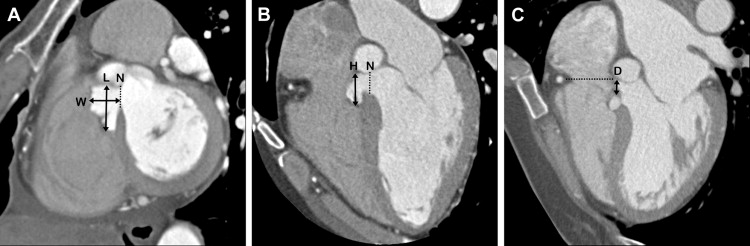
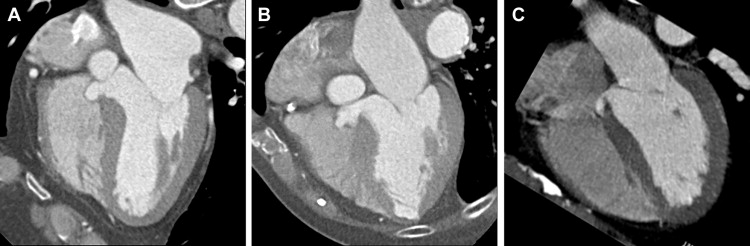
The size and morphologic characteristics of AMVS were evaluated to determine the related factors for embolic stroke. The width and length of AMVS were measured on the SA view and the height on the 4-chamber view ( Figure 2 ). The greatest dimension among them was defined as the longest diameter of AMVS. The neck diameter of AMVS was defined as the narrowest portion along the ventricular septum on each view. To measure the distance from the tricuspid valve, the shortest diameter was measured from the septal leaflet of the tricuspid valve along the ventricular septum on the 4-chamber view. The shape of the AMVS was classified into 3 types as follows: (1) round, spherical feature with smooth margin; (2) lobulated, clam-like feature with digitated margin; and (3) elongated, the height of the AMVS being ≥2 times the width ( Figure 3 ). The volume was calculated assuming that the AMVS was an ellipsoid. We also evaluated for the presence of thrombus attached to AMVS. Any filling defect with low attenuation located in AMVS was defined as intra-aneurysmal thrombus. For all parameters, interobserver agreements were checked, and the average value was used for analysis.
In 52 patients with incidentally detected AMVS on cardiac MDCT, TTE was performed in 41 patients; the mean time interval between the 2 methods was 15 days (range 0 to 90 days). TTE examinations were performed using ultrasonographic systems (Acuson Sequoia 512; Siemens, Erlangen, Germany; Philips i33 Cardiograph; Philips Medical Systems, Eindhoven, The Netherlands). All images and measurements were acquired from the standard views, according to the guidelines of the American Society of Echocardiography. All TTE images and reports transferred to the core laboratory center were reviewed for the presence of AMVS and intra-aneurysmal thrombus on each standard view by 2 experienced cardiologists.
During observation periods, the medical records from each hospital or data from Korean National Statistical Office and National Health Insurance Corporation were obtained for reviewing the occurrence of embolic stroke. Embolic stroke was defined as multiple scattered cerebral infarctions without not only significant steno-occlusion of relevant arteries but also other explainable cause despite an adequate diagnostic evaluation. In our study, transient ischemic attack of unknown cause was included to the embolic stroke. Results were confirmed by an attending neurologist based on clinical symptoms or brain imaging.
Statistical analyses were performed using SPSS, version 20.0 (SPSS, Chicago, Illinois). A p value <0.05 was considered statistically significant. For comparison of the morphologic characteristics of AMVS between the embolic stroke group and event-free group and detectability of AMVS between MDCT and TTE, the independent t test and Fisher’s exact test were used for continuous variables and categorical variables, separately.
Results
The baseline demographic and clinical characteristics of the 52 adults with incidentally detected AMVS by cardiac MDCT are listed in Table 1 . Among them, ventricular septal defects were identified in 3 patients, and they were all of insignificant size. The mean age was 54 years (range 23 to 85 years); 55.8% were women. Half of the patients with AMVS have various symptoms such as atypical chest pain or dyspnea, whereas the other half were asymptomatic. On ECG, 13 patients (25%) had conduction anomalies such as with right bundle branch block (RBBB) (n = 4), first-degree atrioventricular block (n = 3), and atrial fibrillation (n = 3). However, these findings were not severe enough to require pacemaker insertion. In the patients who underwent TTE (n = 41), 17 patients (41.5%) had a coexisting valve disease: tricuspid regurgitation (n = 8), mitral regurgitation (n = 6), aortic regurgitation (n = 2), and aortic stenosis (n = 1). Most of these patients had trivial or mild-degree disease, except for only 1 patient who had moderate aortic regurgitation.
| Age (years), mean ± SD | 54.0 ± 14.2 |
| Female | 29 (55.8%) |
| BMI(kg/m 2 ), mean ± SD | 24.3±4.0 |
| Hypertension | 16 (30.8%) |
| Diabetes mellitus | 6 (11.5%) |
| Dyslipidemia | 14 (26.9%) |
| Smoker | 8 (15.4%) |
| Family history of CVD | 2 (3.8%) |
| Medication of statin | 11 (21.2%) |
| Medication of aspirin or anticoagulation drug | 9 (17.3%) |
| Atypical chest pain | 15 (28.8%) |
| Dyspnea | 7 (13.5%) |
| Palpitation | 3 (5.8%) |
| Syncope | 1 (1.9%) |
| Asymptomatic, but have clinical risk factors | 26 (50.0%) |
| ECG findings | |
| Right bundle branch block | 4 (7.7%) |
| 1st atrioventricular block | 3 (5.8%) |
| Atrial fibrillation | 3 (5.8%) |
| Left anterior fascicular block | 2 (3.8%) |
| Left bundle branch block | 1 (1.9%) |
| Normal or no-specific | 39 (75.0%) |
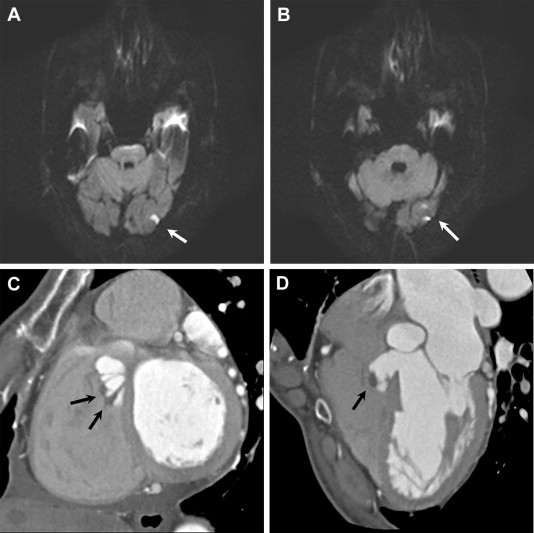
During the median 40-month observation period, embolic strokes occurred in 6 of 43 patients (14%). In the embolic stroke group, the mean age (64.3 ± 17.8 vs 50.6 ± 13.1 years, p = 0.029) and the prevalence of hypertension (66.7% vs 16.2%, p = 0.020) were significantly higher than those of the event-free group. Morphologic parameters, such as the longest diameter, volume, neck diameter, or shape, were not significantly different between the 2 groups. Intra-aneurysmal thrombi were detected in 5 of 43 patients (11.6%) with cardiac MDCT; all these thrombi were detected in AMVS with lobulated shape. The prevalence of intra-aneurysmal thrombus was significantly higher in the embolic stroke group than in the event-free group (50% vs 5.4%, p = 0.014; Figure 4 ). All patients with intra-aneurysmal thrombi were treated with antiplatelet agents. Three of them who had embolic stroke symptom underwent anticoagulant treatment for 2 weeks.
In 52 adults with AMVS, 15 patients underwent follow-up noninvasive imaging (mean 24 months; range 9 to 61 months) such as cardiac MDCT (n = 7) or TTE (n = 9) during the observation period. One patient underwent both MDCT and TTE during follow-up. There was no significant change in the size of the AMVS (mean difference in the longest diameter 0.4 mm; range −2.5 to 1.8 mm) and morphology at the maximum 61-month follow-up.
TTE was performed for 41 of 52 patients with incidentally detected AMVS on cardiac MDCT. AMVS was detected by TTE in 29 of 41 patients (70.7%), in any standard view. AMVS was most commonly visualized on the SA view (77.8%), whereas poorly visualized on the 2-chamber view (22.2%). TTE did not detect AMVS in 12 patients (29.3%) with MDCT-detected AMVS; this was named the TTE(−)/MDCT(+) AMVS group. The longest dimension and volume of the AMVS were significantly smaller in the TTE(−)/MDCT(+) AMVS group than the TTE(+)/MDCT(+) AMVS group (p <0.05; Table 2 ). In the 12 patients with TTE(−)/MDCT(+) AMVS, 5 patients (41.7%) had an AMVS volume <0.5 cm 3 , which was the most common cause of the undetected AMVS with TTE. Other explanations for AMVS being undetected by TTE were poor sonic window because of cardiac valve calcification (n = 3), calcified apical pseudoaneurysm of the left ventricle (n = 1), obesity with a body mass index >30 kg/m 2 (n = 1), and severe thoracic deformity (n = 1). One case was diagnosed as shielded AMVS because of dilated sinus of Valsalva (n = 1). In the TTE(−)/MDCT(+) AMVS group, 1 patient had an episode of acute embolic stroke. Although intra-aneurysmal thrombi were detected by MDCT in 5 patients, none of these thrombi were detected by TTE. The reasons for this were poor sonic window (n = 1), anticoagulant therapy on diagnosis with cardiac MDCT (n = 2), and long interval with >5 days between MDCT and TTE (n = 2).



