The aim of this study was to evaluate the heterogeneity of the association of a preserved or reduced ejection fraction (EF) with the increased risk of outcomes among patients with acute heart failure syndromes. Of the 4,842 patients enrolled in the Acute Decompensated Heart Failure Syndromes (ATTEND) registry in Japan, 4,720 patients were evaluated to investigate the association of EF and clinical features or co-morbidities with all-cause mortality after admission. The median follow-up period after admission was 519 (388 to 781) days. The all-cause mortality rate did not differ between the reduced EF and preserved EF groups (24.9% and 24.5%, respectively). To evaluate the heterogeneity of the influence of a preserved or reduced EF on all-cause mortality, subgroup analyses were performed. As a result, there were significant interactions in the association of a preserved or reduced EF with all-cause mortality when the patients were stratified by an ischemic cause, a hypertensive cause, previous hospitalization for heart failure, diabetes mellitus, and anemia. The influence of a nonischemic cause, a hypertensive cause, or new-onset heart failure on the risk of all-cause mortality was significantly greater in patients with preserved EF than in those with reduced EF. In contrast, the influence of diabetes mellitus or anemia on the risk of all-cause mortality was significantly greater in patients with reduced EF than in those with preserved EF. In conclusion, the present analysis demonstrated that the association of a preserved or reduced EF with the clinical outcome differs markedly in relation to the clinical features or co-morbidities of these patients.
Several epidemiologic studies have recently shown that about half of all patients hospitalized for acute heart failure syndromes (AHFS) have a preserved left ventricular ejection fraction (EF). Patients with heart failure (HF) with a preserved EF have been reported to display pathophysiologic characteristics similar to those of patients with HF with a reduced EF. Furthermore, most of the large-scale contemporary studies have suggested that differences in survival between the 2 types of HF are generally minimal. However, it remains unknown whether there are subgroups of patients with AHFS with a preserved or reduced EF that is associated with a higher risk of morbidity or mortality. Additionally, it has been reported that very few hospitalized HF registries have collected data on both in-hospital and postdischarge outcomes. Accordingly, we evaluated the heterogeneity of the association of a preserved or reduced EF with the increased risk of clinical outcomes among patients hospitalized for AHFS who were evaluated in inpatient and outpatient settings.
Methods
As a nationwide hospital-based prospective cohort study, the Acute Decompensated Heart Failure Syndromes (ATTEND) registry, which is a prospective multicenter observational cohort study of AHFS, accumulates data on patients with AHFS admitted to 53 hospitals throughout Japan. Patients are enrolled at their first admission and then followed, with data collection being patient based and not event based. The study design and methods, as well as patient characteristics, have been described previously. In brief, the ATTEND registry study is being performed to clarify the profile of patients with AHFS in Japan, including demographic and clinical characteristics, current treatment, in-hospital mortality, and postdischarge morbidity or mortality. Treatment of AHFS is not specified and is selected by each attending physician. This study was conducted according to the principles of the Declaration of Helsinki. Institutional review board approval was obtained at each participating hospital before commencing the study, and all patients gave written informed consent.
Patients with AHFS who fit the modified Framingham criteria, which only include variables assessed at admission, are eligible for entry into the ATTEND registry. However, patients aged <20 year old, those with acute coronary syndrome, and others considered unsuitable for the study by their physicians are excluded. The present study focused on patients enrolled in the ATTEND registry from April 2007 to December 2011 for whom left ventricular EF data (or qualitative assessment of left ventricular systolic function) at admission, in-hospital data, and follow-up data after discharge were available. A preserved EF was defined as left ventricular EF >40% or qualitative assessment of normal or mildly impaired systolic function (if left ventricular EF was not measured) at admission, whereas a reduced EF was defined as left ventricular EF ≤40% or moderate and/or severe systolic dysfunction on qualitative assessment at admission. Anemia on admission was defined as hemoglobin <13.0 g/dl for men and <12.0 g/dl for women according to the World Health Organization classification. The primary end point of this study was all-cause mortality after admission, whereas the secondary end point was a composite of all-cause mortality and readmission for HF.
Data are presented as the mean (SD), median with interquartile range, or percentage. Student t test was used for between-group comparison of continuous variables with a normal distribution, whereas the Mann-Whitney U test was used for skewed continuous or discrete variables. Nominal variables were compared with the chi-square test. Curves for the cumulative probability of events were estimated by the Kaplan-Meier method. To evaluate the influence of a preserved or reduced EF on the risk of morbidity or mortality after admission, the Cox proportional hazards model was applied and the heterogeneity of the influence or interaction was evaluated. Two-tailed p values <0.05 were considered to indicate statistically significant differences. All analyses were performed by an independent biostatistics and data center (STATZ Institute, Inc., Tokyo, Japan).
Results
Of the 4,842 patients enrolled in the ATTEND registry during the study period, 4,720 patients (97.4%) with left ventricular EF data at admission, in-hospital data, and follow-up data after discharge were included in this analysis. Left ventricular EF was preserved on admission in 45.2% of the enrolled patients. Baseline characteristics of the patients with a preserved and reduced EF at admission are listed in Table 1 . The median follow-up period after admission was 519 (388 to 781) days. The rate of all-cause mortality after admission was 24.7%, whereas the composite end point of all-cause mortality and readmission for HF was reached by 41.7% of the subjects. This sample of 4,720 patients had 85.5% power to detect an increase of 20% of hazard ratio in risk of all-cause death, with a 2-sided p value <0.05.
| Variables | Overall (n = 4720) | Reduced EF (n = 2585) | Preserved EF (n = 2135) | P-value |
|---|---|---|---|---|
| Age (years) | 72.9±13.8 | 69.7±14.4 | 76.8±12.0 | <0.001 |
| Men | 57.9% | 67.9% | 45.7% | <0.001 |
| Prior hospitalization for heart failure | 36.3% | 39.1% | 32.9% | <0.001 |
| Hypertension | 69.4% | 65.2% | 74.5% | <0.001 |
| Dyslipidemia | 36.8% | 38.8% | 34.5% | 0.002 |
| Diabetes mellitus | 33.8% | 35.1% | 32.1% | 0.030 |
| Chronic obstructive pulmonary disease | 12.3% | 10.8% | 14.1% | <0.001 |
| Stroke | 14.1% | 13.3% | 15.0% | 0.097 |
| Etiology | ||||
| Ischemic | 31.3% | 39.5% | 21.4% | <0.001 |
| Hypertensive | 17.8% | 12.8% | 23.8% | <0.001 |
| Valvular | 19.2% | 11.0% | 29.1% | <0.001 |
| Atrial fibrillation at admission | 36.0% | 31.2% | 41.8% | <0.001 |
| Clinical profile on admission | ||||
| Paroxysmal nocturnal dyspnea | 53.4% | 56.6% | 49.6% | <0.001 |
| Orthopnea | 63.6% | 66.7% | 59.8% | <0.001 |
| Jugular venous distension | 53.2% | 54.5% | 51.5% | 0.172 |
| Peripheral edema | 66.9% | 63.6% | 70.9% | <0.001 |
| NYHA functional class | ||||
| III | 37.8% | 36.4% | 39.6% | 0.022 |
| IV | 43.9% | 48.2% | 38.8% | <0.001 |
| Body mass index (kg/m 2 ) | 23.2±4.6 | 23.2±4.5 | 23.2±4.6 | 0.769 |
| Systolic blood pressure (mmHg) | 145.3±36.6 | 143.1±37.4 | 147.9±35.5 | <0.001 |
| Diastolic blood pressure (mmHg) | 82.5±22.6 | 84.5±23.5 | 80.0±21.2 | <0.001 |
| Heart rate (beats/min) | 98.5±29.2 | 103.7±28.3 | 92.1±29.1 | <0.001 |
| Blood urea nitrogen (mg/dl) | 27.8±26.1 | 28.4±29.6 | 27.0±21.2 | 0.064 |
| Serum creatinine (mg/dl) | 1.43±1.57 | 1.49±1.71 | 1.36±1.38 | 0.004 |
| Estimated GFR (ml/min/1.73m 2 ) | 49.6±26.8 | 49.9±27.7 | 49.4±25.6 | 0.527 |
| Serum sodium (mEq/l) | 139.3±4.4 | 139.2±4.3 | 139.4±4.5 | 0.309 |
| Hemoglobin (g/dl) | 12.0±2.6 | 12.6±2.6 | 11.4±2.4 | <0.001 |
| Anemia ∗ | 58.0% | 50.1% | 67.5% | <0.001 |
| B-type natriuretic peptide (pg/ml) | 708 (363-1287) | 924 (510-1582) | 508 (270-927) | <0.001 |
| Intravenous therapy during hospitalization | ||||
| Diuretics | 76.3% | 77.7% | 74.7% | 0.014 |
| Any vasodilator | 78.6% | 81.2% | 75.4% | <0.001 |
| Any inotrope | 18.5% | 24.1% | 11.8% | <0.001 |
| Oral medications at admission | ||||
| Loop diuretic | 46.3% | 46.4% | 46.1% | 0.865 |
| Spironolactone or eplerenone | 19.8% | 20.9% | 18.4% | 0.160 |
| Angiotensin converting enzyme inhibitor | 14.6% | 16.2% | 12.7% | <0.001 |
| Angiotensin receptor blockers | 35.0% | 30.9% | 39.9% | <0.001 |
| Beta-blockers | 33.8% | 35.1% | 32.2% | 0.033 |
| Calcium-channel blockers | 29.0% | 19.5% | 40.4% | <0.001 |
| Digoxin | 12.8% | 11.4% | 14.5% | 0.002 |
| Aspirin | 32.4% | 33.8% | 30.7% | 0.021 |
| Warfarin | 24.5% | 23.1% | 26.3% | 0.010 |
| Statin | 23.6% | 23.9% | 23.3% | 0.640 |
∗ Anemia was defined as a hemoglobin <13.0 g/dl for men and <12.0 g/dl for women.
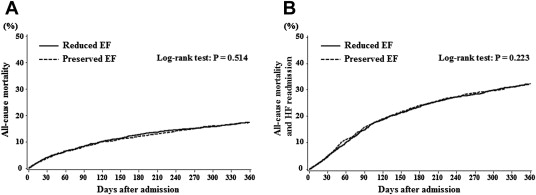
The all-cause mortality rate after admission did not differ between the preserved and reduced EF groups (24.5% and 24.9%, respectively; p = 0.761). Similarly, the composite outcome (all-cause mortality and readmission for HF) did not differ between the 2 groups (41.0% and 42.4%, respectively; p = 0.321). Kaplan-Meier estimates of all-cause mortality and the composite outcome after admission in the reduced EF and preserved EF groups are shown in Figure 1 . The all-cause mortality rate after admission ( Figure 1 ) and the rate of reaching the composite end point ( Figure 1 ) did not differ between the 2 groups (log-rank test p = 0.514 and p = 0.223, respectively).
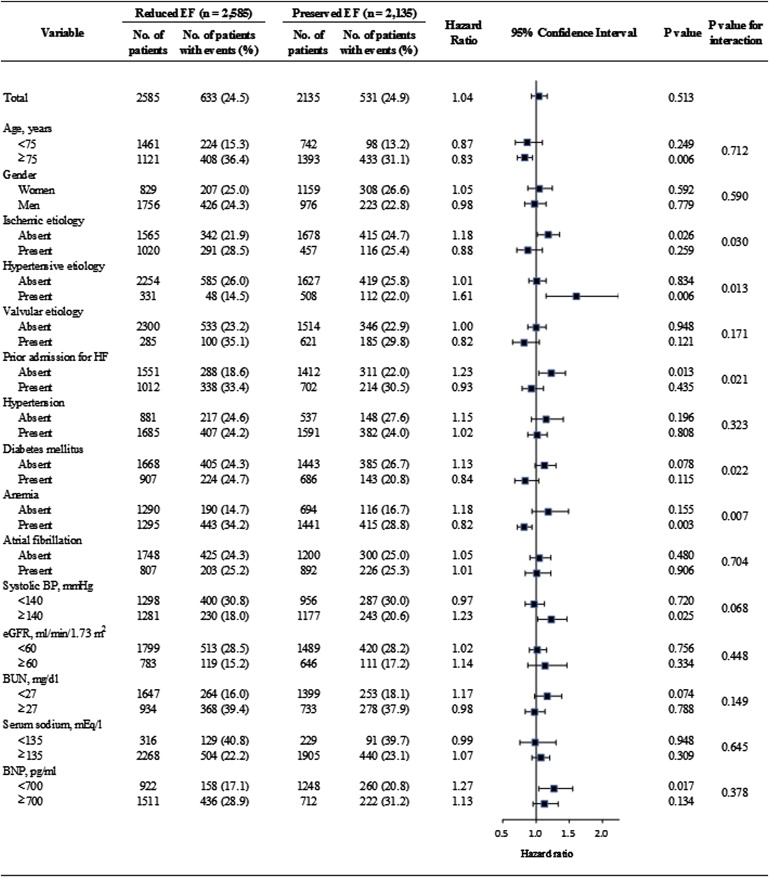
To evaluate the heterogeneity of the association of a preserved or reduced EF with the increased risk of subsequent morbidity or mortality, subgroup analyses were performed using the Cox proportional hazards model ( Figures 2 and 3 ). As shown in Figure 2 , there were significant interactions in the association of a preserved or reduced EF with all-cause mortality when the patients were stratified by an ischemic cause, a hypertensive cause, previous hospitalization for HF, diabetes mellitus (DM), and anemia. The all-cause mortality rate in patients with an ischemic cause did not differ between the preserved and reduced EF groups, whereas this rate in patients without an ischemic cause was significantly higher in patients with preserved EF than in those with reduced EF (p = 0.030 for the interaction). Similarly, the all-cause mortality rate in patients without a hypertensive cause or with previous hospitalization for HF did not differ between these 2 EF groups, whereas this rate in patients with a hypertensive cause or without previous hospitalization for HF (i.e., those with new-onset HF) was significantly higher in patients with preserved EF than in those with reduced EF (the p values for interaction were 0.013 and 0.021, respectively). Thus, the influence of nonischemic cause, hypertensive cause, or new-onset HF on the risk of all-cause mortality was significantly greater in patients with preserved EF than in those with reduced EF. In contrast, the presence of DM was associated with a tendency for a higher risk of all-cause death in patients with reduced EF than in those with preserved EF, whereas the absence of DM was associated with a tendency for a higher risk of all-cause death in patients with preserved EF patients than in those with reduced EF (p = 0.022 for the interaction). In addition, the absence of anemia was associated with a tendency for a higher risk of all-cause death in patients with preserved EF than in those with reduced EF, whereas this rate in patients with anemia was significantly higher in patients with reduced EF than in those with preserved EF (p = 0.007 for the interaction). Thus, the influence of DM or anemia on the risk of all-cause mortality was significantly greater in patients with reduced EF than in those with preserved EF. As shown in Figure 3 , analysis revealed similar trends for the composite end point of all-cause mortality and readmission for HF. Interestingly, there were significant interactions in the association of a preserved or reduced EF with the composite end point, but not all-cause mortality alone, when the patients were stratified by valvular cause and baseline systolic blood pressure (SBP). The composite end point rate in patients with a baseline SBP <140 mm Hg did not differ between these 2 EF groups, whereas this rate in patients with a baseline SBP ≥140 mm Hg was significantly higher in patients with preserved EF than in those with reduced EF (p = 0.036 for the interaction). In contrast, the composite end point rate in patients without a valvular cause did not differ between these 2 EF groups, whereas the presence of a valvular cause was associated with a tendency for a higher risk of the composite end point in patients with reduced EF than in those with preserved EF (p = 0.043 for the interaction).