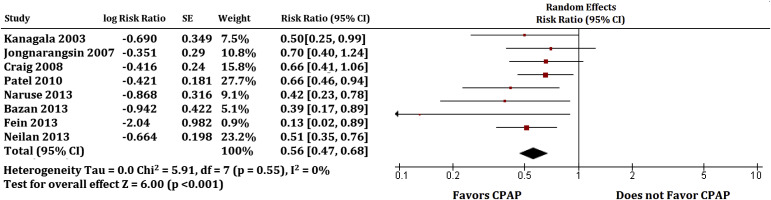
Atrial fibrillation (AF) is a significant health care problem for patients with obstructive sleep apnea (OSA). Continuous positive airway pressure (CPAP) as a therapy for OSA is underused, and it is unknown if CPAP might reduce rates of AF. We systematically reviewed the published reports on CPAP use and risk of AF. MEDLINE, EMBASE, CINAHL, Web of Science, meeting abstracts, and Cochrane databases were searched from inception to June 2015. Studies needed to report the rates of AF in participants who were and were not on CPAP. Data were extracted by 2 authors. A total of 8 studies on OSA were identified (1 randomized controlled trial) with 698 CPAP users and 549 non-CPAP users. In a random effects model, patients treated with CPAP had a 42% decreased risk of AF (pooled risk ratio, 0.58; 95% confidence interval, 0.47 to 0.70; p <0.001). There was low heterogeneity in the results ( I 2 = 30%). In metaregression analysis, benefits of CPAP were stronger for younger, obese, and male patients (p <0.05). An inverse relationship between CPAP therapy and AF recurrence was observed. Results suggest that more patients with AF also should be tested for OSA.
Obstructive sleep apnea (OSA) and atrial fibrillation (AF) are both on an increase in the United States. Cardioversion and catheter ablation therapy are frequently indicated in difficult-to-treat cases of AF. However, there is a high rate of recurrence of AF, ranging from 25% to 60% over 5 years. OSA increases the risk of recurrent AF after catheter ablation by 40% (risk ratio [RR], 1.40; 95% confidence interval [CI], 1.16 to 1.68). Patients with AF are not frequently screened for OSA and much of the OSAs remain untreated in patients with AF who underwent catheter ablation. Cardiologists frequently do not manage OSA and continuous positive airway pressure (CPAP), which may lead to underdiagnosis and undertreatment of AF. It is not well known if treating OSA with CPAP in this group of AF patients is beneficial. We performed a systematic review that examined whether treating OSA with CPAP in patients with AF is associated with reduced risk of recurrent AF after catheter ablation.
Methods
Our study model was based on Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines including the overall design, implementation, and data presentation. We identified research questions, developed and justified eligibility criteria, and prespecified an analytical plan.
Two authors independently assessed study quality and extracted data (W.T.Q. and U.B.N.). MEDLINE, EMBASE, Cochrane databases, EBSCO, and Web of Science were searched from inception to June 2015 for relevant randomized clinical trials and cohort studies. Reference lists of each study were also manually searched for any relevant citations. The search terms used were “sleep apnea,” “obstructive sleep apnea,” “sleep apnoea,” “obstructive sleep aponea,” “sleep apnoea AND heart arrhythmias,” “sleep apnoea AND continuous positive airway pressure,” and “cardiac arrhythmias AND sleep apnea.” Searches were made without any language or other restrictions. Databases were searched for prospective cohort and intervention studies with CPAP as an intervention and cardiac arrhythmia as an outcome measure.
We included all studies that evaluated the efficacy of CPAP in adults aged older than 18 years with a diagnosis of OSA based on polysomnography, with a minimum apnea–hypopnea index of >4 events/hour. Patients had at least one type of arrhythmia, which included atrial and/or ventricular premature beats, AF, atrial flutter, ventricular fibrillation, supraventricular tachycardia, and recurrence of arrhythmias. Studies focused only on central sleep apnea were excluded. We included CPAP intervention in OSA patients with documented arrhythmias and one week or more of CPAP therapy. We excluded any studies that did not report on measures of arrhythmias before and after CPAP usage. Recurrence of AF was considered as the outcome measure. We did not restrict our outcome to any specific follow-up period.
Random effects model was used to estimate pooled effect of CPAP on burden of arrhythmia and number of events of cardiac arrhythmias. Between-study heterogeneity was assessed by I 2 method. Guidelines issued by Cochrane Handbook for Systematic Reviews of Interventions were followed to assess quality of studies. Publication bias was assessed by evaluating a funnel plot for asymmetry. For all studies, we extracted the study baseline characteristics, event rates, sample sizes, RR, and 95% CIs for the primary and secondary outcomes. We extracted RRs for CPAP therapy in catheter-ablated AF patients and recurrence rates of AF from published manuscripts and abstracts. The effect sizes were obtained from intention-to-treat analyses and fully adjusted models in the cohort studies. The primary analysis measured the pooled estimate of recurrent AF risk associated with CPAP therapy.
To study heterogeneity, we hypothesized a priori that the effect sizes might differ according to methodologic quality of the studies. Thus, we used a random effects model as described by DerSimonian-Laird. The random effects model assumes that the studies included in the meta-analysis are a random sample of hypothetical study populations. This model more conservatively estimates combined data with a wider CI, and the summary statistic is less likely to be significant. Heterogeneity was assessed using the Cochrane Q statistic, and the percentage of total variability due to true between-study heterogeneity was evaluated using the I 2 measure. A p value <0.10 was considered significant for I 2 measure and interaction tests.
We assessed publication bias subjectively by visual inspection of Begg’s funnel plot and objectively by Egger’s regression asymmetry test because funnel plots may be inaccurate in the assessment of very large studies. To address the possibility that “N” number of studies possibly were missing from our analysis and that these studies (if included) would shift the effect size toward the null, we used Orwin’s fail-safe N formula. If the meta-analysis has captured all relevant studies, then the funnel plot is expected to be symmetric. However, if there is asymmetry in the plot, it is expected that some studies missing from the analysis. This asymmetry is addressed by Duval and Tweedie “trim and fill” method. For example, if there are more studies on the right-hand side and fewer studies on the left-hand side of the funnel plot, this would raise concern that missing studies potentially exist. However, the “trim and fill” method trims the right-hand asymmetric studies to calculate an unbiased effect by an iterative procedure. It then fills the plot by reintroducing the right-hand trimmed studies on the right and imputed counterparts to the left of the mean effect. We report here the unbiased effect and the number of possible missing studies from the analysis. We also performed an additional cumulative analysis to evaluate if there was a temporal effect of the studies. In addition, we evaluated removal of individual studies on the pooled RRs.
We performed metaregression to examine if the natural log-transformed RRs of the effect of CPAP therapy on AF recurrence were influenced by baseline characteristics of the studies. We used an unrestricted maximal likelihood method for mixed effects regression to evaluate for slope significance. All analyses were performed using RevMan v. 5.0 and Comprehensive Meta-Analysis v. 2.2.4.
Results
Our search yielded a total of 122 published studies after excluding duplicates. These were screened based on abstracts and titles. Of these 122 published studies, 29 studies were obtained and read in detail. Of these, 21 studies were excluded ( Figure 1 ). Finally, 8 studies were included in the meta-analysis, of which 1 was randomized controlled trial and 7 were cohort studies.
The 8 studies were published between 2003 and 2013 and included a total of 4,516 participants with AF who underwent catheter ablation. Of these, 1,247 patients were diagnosed with OSA and 698 were treated with CPAP. AF recurred in 125 (18%) participants who used CPAP and 205 (37%) participants who did not. Characteristics of participants in the 8 studies are given in Table 1 . The mean ages of the participants ranged from 50 to 66 years, and most were men. One study recruited only men.
| Study | N | Study design | Country | Year | Age | Males | BMI | Smoking | Beta blocker | CAD | LVEF | Hypertension | Diabetes | CVA | Dyslipidemia | Severe OSA | CPAP Users |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Kanagala et al. 2003 | 118 | Cohort | USA | 2003 | 66 | 73% | 34 | – | 35% | – | 52% | 63% | 17% | – | – | 100% | 30% |
| Jongnarangsin et al. 2008 | 324 | Cohort | USA | 2007 | 57 | 76% | 28 | – | – | 11% | 56% | 46% | – | – | – | 10% | 56% |
| Craig et al. 2008 | 83 | RCT | UK | 2008 | 50 | 100% | 35 | 19% | 26% | 5% | – | 24% | 24% | 2% | – | 100% | 52% |
| Patel et al. 2010 | 3,000 | Cohort | USA | 2010 | 54 | 76% | 28 | – | – | 12% | 52% | 40% | 15% | 2% | – | 21% | 49% |
| Neilan et al. 2013 | 720 | Cohort | USA | 2013 | 56 | 74% | 30 | – | 68% | 8% | 55% | 51% | 15% | – | 33% | 20% | 50% |
| Bazan et al. 2013 | 56 | Cohort | Spain | 2013 | 66 | 79% | 31 | 55% | 29% | 11% | 61% | 70% | – | – | – | 82% | 48% |
| Fein et al. 2013 | 62 | Cohort | USA | 2013 | 57 | 74% | 26 | – | 4% | 23% | 60% | 68% | 19% | – | – | 100% | 52% |
| Naruse et al. 2013 | 153 | Cohort | Japan | 2013 | 60 | 84% | 25 | – | 64% | – | 66% | 59% | 23% | – | 49% | 76% | 71% |
The strength of evidence and quality assessment of the studies are listed in Table 2 . There was only one randomized controlled trial, and the rest of the studies were cohort studies. Scores show that the cohort studies were of acceptable quality; however, information obtained by randomized controlled trial was of inferior quality. The strength of evidence is intermediate because randomized controlled trials related to the study question were not available. Five studies were performed in the United States, 1 in the United Kingdom, 1 in Japan, and 1 in Spain. All the studies were written in English, and all were published in peer-reviewed journals.
| Study | Question Sufficiently described | Design evident and appropriate to answer study question | Method of subject selection described and appropriate | Subject characteristics sufficiently described | Random Allocation to treatment reported | Blinding of investigators reported | Blinding of subjects reported | Outcome well defined and robust/assessment reported | Sample size appropriate | Analysis described and appropriate | Variance Reported for main outcomes | Controlled for confounding | Results reported in sufficient detail | Results Support conclusions | SCORE |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Kanagala et al. 2003 | Yes | Yes | Yes | Yes | N/A | N/A | N/A | Partial | Yes | Yes | Yes | No | Yes | Yes | 19/22 |
| Jongnarangsin et al. 2008 | Yes | Yes | Yes | Yes | N/A | N/A | N/A | Yes | No | Partial | Yes | No | No | Yes | 15/22 |
| Craig et al. 2008 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | No | Yes | Yes | No | No | Yes | 18/28 |
| Patel et al. 2010 | Yes | Yes | Yes | Yes | N/A | N/A | N/A | Partial | Yes | Partial | Yes | Yes | Yes | Yes | 20/22 |
| Neilan et al. 2013 | Yes | Yes | Yes | Yes | N/A | N/A | N/A | Partial | Yes | Yes | Yes | Yes | Yes | Yes | 21/22 |
| Bazan et al. 2013 | Yes | Yes | Yes | Yes | N/A | N/A | N/A | Partial | Yes | Yes | Yes | No | Yes | Yes | 19/22 |
| Fein et al. 2013 | Yes | Yes | Yes | Yes | N/A | N/A | N/A | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 22/22 |
| Naruse et al. 2013 | Yes | Yes | Yes | Yes | N/A | N/A | N/A | Partial | Yes | Yes | Yes | Yes | Yes | Yes | 21/22 |
Meta-analysis of these 8 studies showed that use of CPAP was associated with 44% decreased risk for recurrence of AF in a random effects model (pooled RR, 0.56; 95% CI, 0.47 to 0.68; p <0.001). There was no heterogeneity in the results (chi square, 5.91; p = 0.55; I 2 = 0%). Removing the study with largest sample size did not change the pooled effect size (pooled RR, 0.53; 95% CI, 0.43 to 0.66; p <0.001). The RR effect sizes ranged from 0.13 to 0.70 for the included studies ( Figure 2 ). We also evaluated the removal of individual studies on pooled RR ( Figure 3 ); the results were consistent. Similarly, plots of the cumulative effect sizes of consecutive studies also showed consistent trend toward benefit ( Figure 4 ).


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


