The presence of mitral regurgitation (MR) is associated with an impaired prognosis in patients with ischemic heart disease. However, data with regard to the impact of this condition in patients with ST-segment elevation myocardial infarction (STEMI) treated by means of primary percutaneous coronary intervention (PPCI) are lacking. Our aim was to assess the effect of MR in the long-term prognosis of patients with STEMI after PPCI. We analyzed a prospective registry of 1,868 patients (mean age 62 ± 13 years, 79.9% men) with STEMI treated by PPCI in our center from January 2006 to December 2010. Our primary outcome was the composite end point of all-cause mortality or admission due to heart failure during follow-up. After exclusions, 1,036 patients remained for the final analysis. Moderate or severe MR was detected in 119 patients (11.5%). Those with more severe MR were more frequently women (p <0.001), older (p <0.001), and with lower ejection fraction (p <0.001). After a median follow-up of 2.8 years (1.7 to 4.3), a total of 139 patients (13.4%) experienced our primary end point. There was an association between the unfavorable combined event and the degree of MR (p <0.001). After adjustment for relevant confounders, moderate or severe MR remained as an independent predictor of the combined primary end point (adjusted hazard ratio [HR] 3.14, 95% confidence interval [CI] 1.57 to 6.27) and each event separately (adjusted HR death 3.1, 95% CI 1.34 to 7.2; adjusted HR heart failure 3.3, 95% CI 1.16 to 9.4). In conclusion, moderate or severe MR detected early with echocardiography was independently associated with a worse long-term prognosis in patients with STEMI treated with PPCI.
It has been consistently proved that mitral regurgitation (MR) after myocardial infarction (MI) conveys a poorer prognosis, and the presence of MR has been linked to an increased risk of death and heart failure (HF). However, information regarding the role of MR in prognosis of patients with ST-segment elevation myocardial infarction (STEMI) treated by means of primary percutaneous coronary intervention (PPCI) remains scarce. PPCI is currently the preferred reperfusion strategy in patients with STEMI and it has shown an impact on the severity of ischemic MR. The presence of acute ischemic MR is a severe complication associated with increased in-hospital mortality. However, consistent data addressing the influence of MR among survivors of a reperfused STEMI are lacking and those published present conflicting outcomes. The purpose of our study was to investigate the effect of residual MR in the long-term prognosis of patients with STEMI treated by PPCI.
Methods
The study cohort consisted of patients with STEMI. The Galician Health Service has developed an active program to offer PPCI to the majority of the population: the PROgrama GALlego de atencion al Infarto Agudo de Miocardio (PROGALIAM). Details of this program have been described previously. All patients presenting with typical chest pain lasting at least 30 minutes with ST-segment elevation ≥1 mm in ≥2 contiguous leads (or reciprocal ST depression ≥1 mm in leads V 1 or V 2 ) or left bundle branch block within the first 12 hours after the beginning of symptoms were eligible for PPCI. Baseline characteristics including cardiovascular (CV) risk factors, medical history, or the use of CV drugs were recorded from the patient directly or from the medical records if necessary.
Patients who died during their index hospitalization, those who presented with mechanical complications, other severe valvulopathy, or those with organic MR (defined as an intrinsic valve disease including severe calcified mitral valve, primary leaflet or chordal pathology, endocarditis, or chronic rheumatic disease) were excluded from the study protocol. The study was designed and performed in accordance with the regulations of the institutional ethical committee. All patients gave written informed consent.
All patients with STEMI during the study period underwent a transthoracic echocardiogram before hospital discharge. Echocardiograms were performed and analyzed by expert echocardiographic cardiologists in our hospital (the interventional hospital) and in the other 3 non–percutaneous coronary intervention centers of our region. The images were digitally recorded for off-line analysis in Xcelera workstation (Philips Medical Systems, Amsterdam, The Netherlands). Data were used unaltered from the original echocardiographic report without knowledge of patients’ outcomes. The severity of MR was assessed during routine clinical interpretation according to current guidelines. For this purpose, color flow Doppler was used as initial evaluation, adding supportive signs and quantitative parameters. The MR was classified into 4 strata as none (grade 0), mild (grade 1+), moderate (grade 2+ to 3+), and severe (grade 4+). For the study purposes, moderate and severe MRs were analyzed altogether, following previously published studies.
The study end point was a composite of all-cause mortality after hospital discharge and development of new-onset HF during follow-up. Mortality was defined as death by any cause and was obtained from hospital records. CV mortality was collected as well and defined as mortality related with a precise CV cause (infarct, arrhythmia, cardiogenic shock, or end-stage HF). HF was considered as readmission to the hospital for management of HF, using for the diagnosis the current guidelines. Data were identified using medical records and discharge summaries.
Results as presented as mean ± SD for continuous normally distributed variables, as median (interquartile range) for continuous nonnormally distributed data, and as percentages for categorical variables. Analysis of normality was performed with the Kolmogorov-Smirnov and Shapiro-Wilk tests. Characteristics were compared across groups with chi-square test or Fisher’s exact test, as required, for categorical variables and analysis of variance or Kruskal-Wallis nonparametric test for continuous variables. Survival curves were constructed using the Kaplan-Meier method and compared by the log-rank test. Cox proportional hazard modeling was used to determine the risk of death or HF according to the different degrees of MR. A model adjusted by age, gender, left ventricular ejection fraction, multivessel coronary disease, final Thrombolysis In Myocardial Infarction flow in the responsible artery, Killip class at admission, anterior infarct, previous MI, previous coronary artery bypass grafting, and diabetes was used to address the effect of MR degrees on our primary end point. To better depict the effect of the MR degrees on clinical events, a Cox regression analysis using moderate and severe MR as individual degrees and comparing them with no or mild MR was carried out as well. p Values <0.05 were considered significant. All analyses were performed with SPSS 20.0 statistical package for Windows (SPSS 20.0, Chicago, Illinois).
Results
From January 2006 to December 2010, a total of 1,868 consecutive patients with STEMI were treated by PPCI at the Complejo Hospitalario Universitario A Coruña, of whom 1,069 had an echocardiogram performed before discharge, available for analysis. Forty-three patients were also excluded because of in-hospital death, 27 because of organic MR, and 7 because of mechanical complication or other severe valvulopathy. After exclusions, the study population comprised 1,036 patients. The median time between PPCI and the echocardiography was 4 days (interquartile range 2 to 6). No trace of MR was detected in 462 patients (44.6%), mild degree of MR was present in 455 patients (43.9%), and moderate or severe MR in 119 patients (11.5%; moderate MR 90 patients [8.7%] and severe MR 29 patients [2.8%]).
Baseline clinical and demographic characteristics, stratified by the severity of MR, are listed in Table 1 . Patients with greater degrees of MR were more likely to be older, women, and to show history of diabetes, hypertension, and smoking habit. They presented also with higher Killip class and more frequent multivessel coronary artery disease. The rest of the baseline characteristics were balanced between groups.
| Variable | MR | |||
|---|---|---|---|---|
| No (n = 462) | Mild (n = 455) | Moderate or Severe (n = 119) | p Value | |
| Age (yrs) | 59 ± 13 | 63 ± 13 | 69 ± 11 | <0.001 |
| Women | 69 (15) | 105 (23) | 34 (29) | <0.001 |
| Hypertension | 187 (40) | 220 (48) | 63 (53) | 0.006 |
| Diabetes mellitus | 57 (12) | 89 (20) | 26 (22) | 0.002 |
| Current smokers | 231 (50) | 162 (36) | 18 (15) | <0.001 |
| Dyslipidemia | 175 (38) | 187 (41) | 48 (40) | 0.30 |
| Cardiac arrest | 7 (2) | 5 (1) | 1 (1) | 0.42 |
| Killip III and IV | 9 (2) | 19 (4) | 12 (8) | 0.003 |
| MI location | ||||
| Anterior | 198 (43) | 198 (44) | 52 (44) | 0.50 |
| Inferior | 229 (50) | 231 (51) | 58 (49) | 0.47 |
| Previous MI | 34 (7) | 34 (8) | 8 (7) | 0.51 |
| PreCABG | 7 (2) | 3 (1) | 3 (3) | 0.09 |
| Stroke or TIA | 10 (2) | 16 (4) | 4 (3) | 0.21 |
| Number of vessels | 0.02 | |||
| 1-Vessel disease | 243 (53) | 227 (50) | 47 (40) | |
| 2-Vessel disease | 123 (27) | 131 (29) | 41 (35) | |
| 3-Vessel disease | 67 (29) | 84 (19) | 25 (21) | |
| TIMI 3 after PPCI | 266 (92) | 246 (90) | 62 (88) | 0.396 |
With regard to echocardiographic data, patients with increasing degree of MR presented with significantly lower left ventricular ejection fraction, higher left ventricular diameters, and E/E′ ratio ( Table 2 ).
| Variable | MR | |||
|---|---|---|---|---|
| No (n = 462) | Mild (n = 455) | Moderate or Severe (n = 119) | p Value | |
| Left ventricular ejection fraction (%) | 57 ± 10 | 53 ± 11 | 46 ± 14 | <0.001 |
| Left ventricular end-diastolic diameter (cm) | 4.8 ± 0.6 | 4.9 ± 0.6 | 5.2 ± 0.8 | <0.001 |
| Left ventricular end-systolic diameter (cm) | 3.2 ± 0.6 | 3.4 ± 0.7 | 3.8 ± 1.0 | <0.001 |
| E Doppler mitral/E′ tissue Doppler mitral | 8.4 ± 3.3 | 11.5 ± 5.5 | 13.6 ± 6.9 | 0.006 |
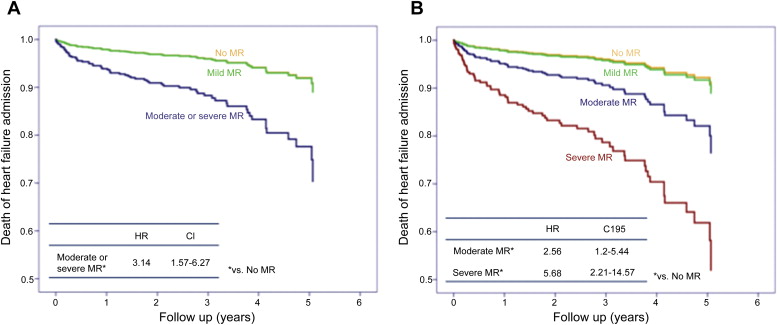
During a median follow-up of 2.8 years (range 1.7 to 4.3), the primary event occurred in 139 patients (13.4%; 79 patients during in this time, of which CV cause was diagnosed in 50 of them, and 60 patients needed to be readmitted due to HF). The risk of developing the primary end point was higher in patients with moderate or severe MR compared with those with mild or no MR (34.5% vs 14.1% vs 7.4%; p <0.001). Kaplan-Meier analysis showed an association between the unfavorable combined event and the degree of MR. In fact, the survival free of death or HF at median follow-up for patients with no MR, mild MR, and moderate or severe MR were 95%, 90%, and 70%, respectively (p value <0.001).
After adjustment for relevant confounders, moderate or severe MR remained as an independent predictor of death or HF (hazard ratio [HR] 3.14, 95% confidence interval [CI] 1.57 to 6.27, p = 0.001; Figure 1 ). In addition to MR, other independent factors of the combined outcome were age, female gender, left ventricular ejection fraction, previous MI, previous coronary artery bypass grafting, and Killip class III or IV at admission ( Table 3 ). When analyzing separately each end point of the combined event, the same Cox proportional hazard model showed that moderate or severe MR was a significant predictor of mortality (HR 3.11, 95% CI 1.34 to 7.2, p = 0.008) and readmission for the treatment of HF (HR 3.3, 95% CI 1.16 to 9.42, p = 0.026; Figure 2 ). Similar results were obtained when CV mortality was studied. Thereby higher degrees of MR persisted as an independent predictor of the CV combined end point (HR 3.83, 95% CI 1.66 to 8.8, p = 0.002) and CV mortality (HR 6.06, 95% CI 1.59 to 23.08, p = 0.008) in the multivariable analysis.
| Variable | HR | 95% CI | p Value |
|---|---|---|---|
| MR | |||
| Mild | 1.11 | 0.57–2.18 | 0.75 |
| Moderate or severe | 3.14 | 1.57–6.27 | 0.001 |
| Age | 1.04 | 1.02–1.06 | 0.001 |
| Female sex | 1.96 | 1.14–3.38 | 0.02 |
| Left ventricular ejection fraction | 0.93 | 0.91–0.95 | <0.001 |
| Previous MI | 2.49 | 1.23–5.03 | 0.01 |
| Previous CABG | 3.44 | 1.01–11.7 | 0.048 |
| Killip class III and IV | 3.08 | 1.4–6.81 | 0.006 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


