Direct transfer (DT) to the catheterization laboratory has been demonstrated to reduce delays in primary percutaneous coronary intervention (PPCI). However, data with regard to its effect on long-term mortality are sparse. The aim of this study was to investigate the effect of DT on long-term mortality in patients with ST-segment elevation myocardial infarctions treated with PPCI. A cohort study was conducted of 1,859 patients (mean age 63.1 ± 13 years, 80.2% men) who underwent PPCI from May 2005 to December 2010. From the whole series, 425 patients (23%) were admitted by DT and 1,434 (77%) by emergency departments. DT patients were younger (mean age 61 ± 12 vs 64 ± 12 years, p = 0.017), were more frequently men (86% vs 76%, p = 0.001), and had a higher proportion of abciximab use (77% vs 64%, p <0.0001). The DT group had a shorter median contact-to-balloon time (105 vs 122 minutes, p <0.0001) and a shorter time to treatment (185 vs 255 minutes, p <0.0001) compared with the emergency department group. Thirty-day and long-term mortality (median follow-up 2.4 years, interquartile range 1.6 to 3.2) were lower in the DT group (3% vs 6%, p = 0.049, and 9.4% vs 14.4%, p = 0.008, respectively). An adjusted Cox regression analysis proved that the DT group had an improved prognosis during follow-up (hazard ratio 0.71, 95% confidence interval 0.50 to 0.99). In conclusion, DT of patients with ST-segment elevation myocardial infarctions for PPCI was associated with fewer delays and improved survival. This benefit was maintained after long follow-up. This strategy should be emphasized in all networks of ST-segment elevation myocardial infarction care.
Primary percutaneous coronary intervention (PPCI) is the current preferred strategy to treat patients with ST-segment elevation myocardial infarctions (STEMIs) when performed in a timely fashion by experienced operators. This technique has yielded superior results over thrombolytic therapy even when long transfer distances are necessary. A relevant prognostic role of reperfusion delays in STEMI has been demonstrated, and door-to-balloon and total ischemic time have been linked to increasing mortality. However, delays in performing PPCI are usually longer than recommended in practice guidelines, and this may nullify the advantages of mechanical reperfusion over lysis. To overcome this problem, several strategies have been proposed, and national efforts in the United States and in Europe have been made to address all organizational issues. Among these strategies, direct transfer (DT) from the field, bypassing the emergency department, to the catheterization laboratory has emerged as a safe and effective protocol for minimizing PPCI-related delays. Nevertheless, data with regard to its effect on mortality and, above all, its long-term impact on patients’ prognoses are lacking. The purpose of this study was to address the effect of DT of patients with STEMI from the field on long-term mortality.
Methods
Data with regard to our STEMI network have been reported elsewhere. According to this program, all patients directly admitted to hospitals with interventional facilities are offered PPCI as the preferred reperfusion strategy, and patients arriving at hospitals without on-site PPCI capabilities are rapidly transferred to interventional hospitals to undergo the procedure. Transport of patients is carried out mostly by Emergency Medical System-061 (EMS-061), although a significant proportion of patients reach the hospital by their own means. EMS-061 has 2 types of ambulances: transport ambulances, managed by paramedics with the capabilities to mobilize patients and provide basic life support, and emergency care ambulances, managed by medical staff members with training in intensive care medicine and capable of delivering advanced life support. Ambulances can collect patients directly from secondary hospitals or from primary care points. Emergency care ambulances have the capability to activate the interventional team directly. This activation is strongly recommended when patients’ first contact is EMS-061, directly or through their primary care physicians.
All patients presenting with typical chest pain lasting >30 minutes with ST-segment elevation ≥1 mm in ≥2 contiguous leads (or reciprocal ST-segment depression ≥1 mm in lead V 1 or V 2 ) or left bundle branch block in the first 12 hours after symptom onset were eligible for PPCI. Patients transferred for rescue PCI or those who were not intended for angioplasty were excluded from the analysis.
Time to contact was defined as the time from symptom onset and first contact with the medical system able to perform the diagnosis of STEMI (EMS-061 emergency care ambulances or emergency departments). Time to treatment was defined as the time that had elapsed between symptom onset and mechanical reperfusion. Contact-to-balloon delay was the time between the first medical contact (the emergency departments of PCI or non-PCI hospitals or EMS-061 ambulances in cases of DT) and the restoration of coronary blood flow. Mortality was defined as death by any cause within that period, the information being obtained from medical records or by telephone call if necessary. We assessed short-term (30 days), midterm (6 months), and long-term (end of follow-up) mortality.
Results are presented as mean ± SD for continuous normally distributed variables, as median (interquartile range) for continuous data not normally distributed, and as percentages for categorical data. Analysis of normality was performed using the Kolmogorov-Smirnov and Shapiro-Wilk tests. Categorical data and proportions were compared using chi-square or Fisher’s exact tests as required. Comparisons of continuous variables were analyzed using unpaired Student’s t tests and Mann-Whitney U tests as appropriate. Logistic regression analysis adjusted for age >75 years, gender, and cardiogenic shock on admission was used to adjust the relation between DT and short-term mortality. Cox regression analysis adjusted for age >75 years, gender, cardiogenic shock, diabetes, anterior wall myocardial infarction, time to contact, angiographic success, and the left ventricular ejection fraction was performed to assess the role of DT in long-term mortality. A subgroup analysis was also performed to evaluate the effect of DT on survival in patients with high risk profiles. Subgroups analyzed were early presenters (≤2 hours from symptom onset), those with anterior wall myocardial infarction, those with cardiogenic shock on admission, and those with known diabetes mellitus. Survival analysis and survival curves were obtained using the Kaplan-Meier method. A p value <0.05 was considered significant. All analyses were performed using SPSS version 20.0 for Windows (SPSS, Inc., Chicago, Illinois).
Results
From May 2005 to December 2010, 2,119 patients entered in our STEMI protocol. Most had STEMIs (n = 1,859 [88%], mean age 63.1 ± 13 years, 80.2% men), and only 260 patients (12%) had no significant coronary lesions.
Of 1,859 patients with STEMIs, 425 (23%) were triaged in the field and directly transported to the catheterization laboratory by EMS-061, whereas 1,434 (77%) first attended the emergency departments of any of the hospitals included in our angioplasty network. Baseline clinical and procedural characteristics are listed in Tables 1 and 2 . Patients who experienced DT were younger, more frequently men, and more frequently smokers, and the use of abciximab was significantly higher in this group. With regard to procedural characteristics, patients in the DT group had a higher percentage of radial access and lower heart rates. The rest of the baseline clinical, angiographic, and procedural characteristics were balanced between groups.
| Variable | DT (n = 425) | Emergency Department (n = 1,434) | p Value |
|---|---|---|---|
| Age (yrs) | 61 ± 12 | 64 ± 12 | 0.017 |
| Men | 365 (86%) | 1,125 (76%) | 0.001 |
| Hypertension | 165 (39%) | 602 (42%) | 0.246 |
| Diabetes | 65 (15%) | 261 (18%) | 0.166 |
| Current smokers | 160 (38%) | 419 (30%) | 0.001 |
| Dyslipidemia ∗ | 158 (37%) | 464 (32%) | 0.064 |
| Anterior wall myocardial infarction | 184 (43%) | 608 (42%) | 0.748 |
| Previous myocardial infarction | 23 (5.4%) | 92 (6.4%) | 0.451 |
| Previous unstable angina | 24 (5.6%) | 101 (7%) | 0.313 |
| Previous PCI | 25 (6%) | 92 (6.4%) | 0.691 |
| Previous coronary bypass graft | 2 (0.5%) | 15 (1%) | 0.274 |
| Cardiogenic shock | 13 (3.1%) | 46 (3.2%) | 0.878 |
| Abciximab use | 326 (77%) | 911 (64%) | <0.0001 |
∗ Low-density lipoprotein cholesterol ≥130 mg/dl, total cholesterol ≥200 mg/dl, or statin treatment.
| Variable | DT (n = 425) | Emergency Department (n = 1,434) | p Value |
|---|---|---|---|
| Multivessel disease | 189 (44%) | 689 (48%) | 0.195 |
| Radial access | 343 (81%) | 1,079 (75%) | 0.020 |
| Coronary artery diseased | |||
| Left main | 11 (2.6%) | 46 (3.2%) | 0.515 |
| Right | 256 (60%) | 860 (60%) | 0.922 |
| Left circumflex | 147 (35%) | 558 (39%) | 0.107 |
| Left anterior descending | 274 (65%) | 941 (66%) | 0.662 |
| TIMI flow grade 0/1 before intervention | 276 (65%) | 1,018 (71%) | 0.215 |
| Stent use | 361 (85%) | 1,187 (83%) | 0.293 |
| Drug-eluting stent | 35 (8.2%) | 128 (8.9%) | 0.658 |
| Left ventricular ejection fraction | 58.7 ± 14.1 | 57.3 ± 14.8 | 0.117 |
| Systolic blood pressure (mm Hg) | 130 ± 29 | 131 ± 32 | 0.611 |
| Heart Rate (beats/min) | 73 ± 19 | 76 ± 20 | 0.014 |
| Complete revascularization | 245 (58%) | 787 (55%) | 0.327 |
| Angiographic success | 405 (97%) | 1,343 (94%) | 0.210 |
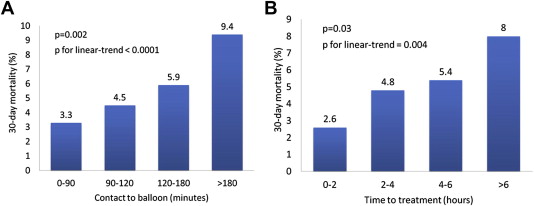
Time intervals are listed in Table 3 . The group with DT experienced fewer delays in all time intervals to accomplish PPCI. The percentage of patients experiencing contact-to-balloon intervals <90 minutes was significantly higher with the DT strategy (33.3% vs 27.2%, p = 0.016). The same result was observed in the case of contact-to-balloon interval <120 minutes (68% vs 49.3%, p <0.0001). The importance of achieving fewer delays is depicted in Figure 1 , in which a significant relation is shown between the 2 time intervals previously mentioned and 30-day mortality.
| Variable | DT (n = 425) | Emergency Department (n = 1,434) | p Value |
|---|---|---|---|
| Time to contact (minutes) | 69 (32–135) | 120 (56–208) | <0.0001 |
| Contact-to-balloon delay (minutes) | 105 (82–131) | 122 (88–170) | <0.0001 |
| Time to treatment (minutes) | 185 (133–263) | 255 (171–384) | <0.0001 |
Patients in the DT group experienced lower rates of death at 30 days (3% vs 6%, p = 0.049), 6 months (5.6% vs 8.6%, p = 0.045), and the end of follow-up (9.4% vs 14.4%, p = 0.008). DT was associated with lower 30-day mortality after adjustment for relevant prognostic variables (adjusted odds ratio 0.6, 95% confidence interval 0.42 to 0.99). After a median follow-up period of 2.4 years (interquartile range 1.6 to 3.2), a Cox regression analysis showed that DT was independently associated with better long-term survival (adjusted hazard ratio 0.71, 95% confidence interval 0.50 to 0.99). All variables included in unadjusted and adjusted analysis are listed in Table 4 , and Cox-derived survival curves are shown in Figure 2 . An analysis of patients with early presentation, anterior wall myocardial infarctions, cardiogenic shock on admission, and known diabetes mellitus demonstrated a beneficial effect of DT across all subgroups, although statistical significance was achieved only in patients with anterior wall myocardial infarctions. Kaplan-Meier survival curves and survival analysis are shown in Figure 3 .
| Variable | Unadjusted HR | 95% CI | p Value | Adjusted HR | 95% CI | p Value |
|---|---|---|---|---|---|---|
| Direct transfer | 0.63 | 0.45–0.89 | 0.009 | 0.71 | 0.50–0.99 | 0.043 |
| Women | 1.29 | 0.96–1.73 | 0.094 | 0.85 | 0.62–1.16 | 0.295 |
| Age >75 yrs | 2.78 | 2.15–3.60 | <0.0001 | 3.10 | 2.35–4.04 | <0.0001 |
| Killip class IV | 9.47 | 6.66–13.46 | <0.0001 | 9.42 | 6.4–13.86 | <0.0001 |
| Angiographic success | 0.26 | 0.20–0.38 | <0.0001 | 0.47 | 0.32–0.68 | <0.0001 |
| Anterior wall myocardial infarction | 1.70 | 1.32–2.19 | <0.0001 | 1.74 | 1.35–2.24 | <0.0001 |
| Time to contact (h) | 1.03 | 0.99–1.07 | 0.147 | 1.01 | 0.97–1.10 | 0.607 |
| Diabetes mellitus | 2.26 | 1.72–2.97 | <0.0001 | 1.92 | 1.45–2.54 | <0.0001 |
| Left ventricular ejection fraction | 0.96 | 0.95–0.97 | <0.0001 | 0.96 | 0.94–0.97 | <0.0001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


