Pathologic conditions associated with inflammation show an inverse correlation between high-density lipoprotein cholesterol (HDL-C) and inflammatory biomarker levels. Our aim was to investigate, in patients with acute coronary syndrome (ACS), whether very low HDL-C levels are associated with inflammatory biomarkers. In a cross-sectional study, we included 6,134 patients with ACS; they were classified as having very low (<30 mg/dl), low (30 to 39.9 mg/dl), and normal HDL-C (≥40 mg/dl) levels. We analyzed the association of different categories of HDL-C levels with serum levels of inflammatory biomarkers, high-sensitivity C-reactive protein (hs-CRP), albumin, and white blood cell count at admission. Overall, 18.5% of patients had very low HDL-C levels. Patients with very low HDL-C levels, compared to patients with low or normal HDL-C levels, had the highest hs-CRP (median 17.8 [interquartile range 7.2 to 54.5] vs 12.6 [5.6 to 33.9] vs 12.0 [5.4 to 36.9] mg/L, respectively, p <0.001) and the lowest albumin levels (median 3.6 [IQR 3.3 to 4.0] vs 3.8 [3.5 to 4.0] vs 3.8 [3.5 to 4.1] g/dl, respectively, p <0.001). White blood cell count did not differ significantly (p = 0.40). The multivariate analysis showed that albumin ≤3.5 g/dl (odds ratio 2.16, 95% confidence interval 1.88 to 2.49, p <0.001) and hs-CRP ≥10 mg/L (odds ratio 1.35, 95% confidence interval 1.17 to 1.55, p <0.001) were independent predictors of very low HDL-C levels. Patients with very low HDL-C levels had the highest inhospital mortality rates compared with the other groups. In conclusion, in patients with ACS, hs-CRP and serum albumin were associated independently with very low HDL-C levels.
Besides atherosclerosis, other conditions with clear inflammatory components, such as systemic lupus erythematosus, rheumatoid arthritis, Kawasaki disease, ankylosing spondylitis, and critically ill patients, have been associated with significantly reduced high-density lipoprotein cholesterol (HDL-C) levels, and investigators have shown an inverse correlation between HDL-C levels and the levels of inflammatory cytokines. However, few studies have assessed the relation between HDL-C levels and biomarkers of inflammation across the acute coronary syndrome (ACS) spectrum. The aim of our study was to evaluate whether very low HDL-C levels are associated with inflammatory biomarkers, including high-sensitivity C-reactive protein (hs-CRP), white blood cell (WBC) count, and serum albumin, in a retrospective cross-sectional study of patients with ST-elevation myocardial infarction (STEMI) or non–ST-elevation ACS (NSTE-ACS).
Methods
In this retrospective cross-sectional study, the following data, ranging from October 1, 2005, to December 31, 2013, were gathered from the database of the Coronary Care Unit of the National Institute of Cardiology, Mexico City: baseline demographic data, medical history, laboratory test, and coronary angiography results. Patients with a diagnosis of ACS were identified and classified as having either an STEMI or NSTE-ACS, on the basis of clinical characteristics, electrocardiographic changes, and biochemical markers of cardiac necrosis, according to the standard definitions of the American College of Cardiology.
In our study, on the basis of the available data, we included, as inflammatory biomarkers, hs-CRP, WBC count (positive acute-phase markers), and serum albumin (negative acute-phase markers), which are known acute-phase reactants in inflammatory disorders. For the purpose of our analysis, patients were included if serum levels of total cholesterol (TC), low-density lipoprotein cholesterol, HDL-C, triglycerides (TG), and inflammatory biomarkers (hs-CRP, WBC count, and serum albumin) were determined within the first 24 hours of admission. Patients with a suspected ongoing infection at admission, by clinical, laboratory, or image investigations, and patients with an autoimmune disease or cancer previously diagnosed or documented during their current hospitalization were not eligible for study inclusion.
Additionally, depending on the HDL-C levels recorded during hospital admission, patients were categorized into HDL-C level subgroups, defined as very low (<30 mg/dl), low (30–39.9 mg/dl), and normal (≥40 mg/dl), on the basis of guidelines of the National Cholesterol Education Program Adult Treatment Panel III.
Coronary angiography was performed in the hemodynamics laboratory and analyzed by interventional cardiologists from our institution. Significant coronary disease was defined as a ≥50% luminal diameter narrowing in each of the three major coronary arteries or of the left main coronary artery. Furthermore, the extent of coronary artery disease was categorized according to the number of affected vessels, as one-vessel, two-vessel, or three-vessel disease, and left main coronary artery.
The primary aim was to evaluate the association between HDL-C levels and biomarkers of inflammation in patients with STEMI or NSTE-ACS. The rate of in-hospital mortality for HDL-C level subgroups was recorded.
All categorical data were summarized as frequencies and percentages. All continuous variables were tested and confirmed to have a non-normal distribution as determined by the Kolmogorov–Smirnov test. Continuous variables were reported as medians and 25th and 75th percentiles (interquartile ranges [IQRs]). Differences in baseline characteristics across HDL-C groups at study entry were assessed, either using the chi-square or Fisher’s exact tests in the case of categorical variables or the Kruskal–Wallis or Mann–Whitney U tests, as appropriate, for continuous variables. The strengths of correlation between HDL-C levels and the inflammatory biomarkers hs-CRP, WBC count, and serum albumin were assessed using the Spearman’s rank correlations. Stepwise logistic regression analysis was performed to adjust for factors associated with very low HDL-C levels. Candidate covariates included in the multivariate analysis were those associated with very low HDL-C levels in a univariate analysis, which included all variables in the baseline characteristics and serum hs-CRP concentrations of ≥10 mg/L, WBC count of ≥10 × 10 3 /μl, and serum albumin levels of ≤3.5 g/dl, that had a value of p ≤0.05. These inflammatory biomarkers were dichotomized according to previously established cut-offs. Odds ratios (ORs) with 95% confidence intervals (CIs) were calculated for variables in both univariate and multivariate analyses. Separate regression models were estimated for STEMI and NSTE-ACS. Using the normal HDL-C level as referent, multivariate regression model was performed to determine the risk of inhospital mortality by HDL-C levels, unadjusted and after adjustment for age ≥65 years, gender, hs-CRP ≥10 mg/L, WBC count of ≥10 × 10 3 /μl, and serum albumin levels of ≤3.5 g/dl.
Results were reported using 2-tailed significance; statistical significance was set at p ≤0.05. All analyses were performed using SPSS version 13 statistical software (Chicago, Illinois).
Results
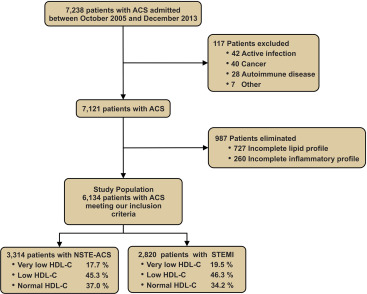
During the study period, 7,238 patients were admitted with a final diagnosis of ACS, of whom 1,104 patients were not eligible for subsequent analyses and therefore excluded ( Figure 1 ).
Among the 6,134 patients analyzed, 1,136 (18.5%) had very low (<30 mg/dl), 2,809 (45.8%) low (30 to 39.9 mg/dl), and 2,189 (35.7%) normal (≥40 mg/dl) HDL-C levels. Patients with very low HDL-C levels were younger, more often men, had higher body mass index, and were significantly more likely to have a history of current smoking, diabetes, heart failure, and renal dysfunction, compared with patients with higher HDL-C levels. In addition, TC and low-density lipoprotein cholesterol levels were lower in patients with very low HDL-C levels (p <0.001; Table 1 ).
| Variable | High-density Lipoprotein Cholesterol (mg/dl) | ||||
|---|---|---|---|---|---|
| Overall (n = 6,134) | < 30 (n = 1,136) | 30-39.9 (n = 2,809) | ≥ 40 (n = 2,189) | P- Value | |
| Age median, (IQR) (years) | 61 (53-69) | 59 (51-67) | 60 (52-68) | 62 (54-70) | <0.001 |
| Men | 79.0% | 86.5% | 82.6% | 70.5% | <0.001 |
| Body mass index median, (IQR) (kg/m 2 ) | 27 (25-29) | 27 (25-29) | 27 (25-29) | 26 (24-29) | <0.001 |
| Current smoker | 28.8% | 33.1% | 30.3% | 24.6% | <0.001 |
| Hypertension | 59.2% | 57.3% | 58.8% | 60.7% | 0.14 |
| Dyslipidemia | 45.6% | 42.7% | 47.5% | 44.8% | 0.01 |
| Diabetes Mellitus | 38.9% | 41.7% | 39.7% | 36.4% | 0.005 |
| Previous MI | 30.1% | 29.7% | 29.8% | 30.7% | 0.73 |
| Previous heart failure | 8.3% | 10.0% | 7.4% | 8.5% | 0.02 |
| Previous stroke | 2.7% | 2.9% | 2.7% | 2.5% | 0.72 |
| Renal dysfunction ∗ | 6.1% | 8.1% | 5.2% | 6.3% | 0.002 |
| Previous CABG | 5.0% | 4.1% | 4.9% | 5.6% | 0.19 |
| Previous PCI | 15.1% | 15.2% | 15.5% | 14.6% | 0.71 |
| Previous statin | 30.5% | 29.4% | 31.0% | 30.2% | 0.57 |
| Initial lipid values | |||||
| Total cholesterol, median (IQR) (mg/dL) | 163 (133-195) | 137 (112-170) | 164 (135-196) | 173 (146-202) | <0.001 |
| HDL-C median, (IQR) (mg/dL) | 36 (31-43) | 26 (23-28) | 35 (32-37) | 45 (42-51) | <0.001 |
| LDL-C median, (IQR) (mg/dL) | 98 (73-123) | 82 (62-108) | 100(76-125) | 102 (78-126) | <0.001 |
| Triglycerides, median, (IQR) (mg/dL) | 145 (108-193) | 149 (111-205) | 153 (116-200) | 130 (99-177) | <0.001 |
∗ Renal dysfunction, creatinine depuration was ≤30 ml/min at the time of admission.
In the overall population studied, 4,637 patients underwent coronary angiography. Of note, although not statistically significant, a trend of multivessel disease in patients with very low HDL-C levels was observed (p = 0.08; Table 2 ).
| HDL-Cholesterol (mg/dl) | |||||
|---|---|---|---|---|---|
| (n = 4,637) | < 30 (n = 822) | 30-39.9 (n = 2,163) | ≥ 40 (n = 1,652) | P -value ∗ | |
| Number of Narrowed Coronary Arteries † | |||||
| None | 8.7% | 7.9% | 8.1% | 9.7% | 0.08 |
| 1 | 41.6% | 38.6% | 42.5% | 41.9% | |
| 2 | 28.6% | 31.0% | 27.6% | 28.7% | |
| 3 | 21.1% | 22.5% | 21.8% | 19.6% | |
| Left main narrowing ‡ | 7.1% | 7.5% | 6.6% | 7.6% | 0.3 |
∗ p-Values are for trends across high-density lipoprotein categories.
† Narrowed Coronary Artery is defined as a significant stenosis ≥ 50% of a major epicardial artery (left anterior descending, left circumflex, and right coronary arteries).
‡ Left main narrowing refers to a significant stenosis ≥ 50% in the left main coronary artery.
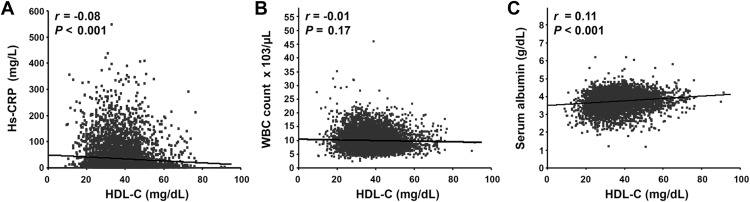
For the entire study population, Spearman’s rank correlation coefficient showed a weak, but statistically significant, inverse correlation between HDL-C and hs-CRP levels ( r = −0.08, p <0.001) and a positive, statistically significant correlation between HDL-C and serum albumin levels ( r = 0.11, p <0.001). No correlation was found between the WBC count and HDL-C levels ( r = −0.01, p = 0.17; Figure 2 ). Overall, baseline levels of hs-CRP were significantly higher in patients with very low HDL-C levels than in those with low and normal HDL-C levels (p <0.001), whereas the WBC count did not differ significantly (p = 0.40). In contrast, serum albumin values were lower in patients with very low HDL-C levels compared to patients with low and normal HDL-C levels (p <0.001; Table 3 ). Similar patterns of inflammatory biomarkers were observed in both STEMI and NSTE-ACS groups, with patients with very low HDL-C levels having the highest hs-CRP levels and lower serum albumin levels, compared with patients from other HDL-C categories.
| All ACS | HDL-Cholesterol (mg/dl) | ||||
|---|---|---|---|---|---|
| Overalln = 6,134 | < 30(n = 1,136) | 30-39.9(n = 2,809) | ≥ 40(n = 2,189) | P -Value | |
| Hs-CRP, median (IQR) (mg/L) | 13.2 (5.8-38.0) | 17.8 (7.2-54.5) | 12.6 (5.6-33.9) | 12.0 (5.4-36.9) | <0.001 |
| Albumin, median (IQR) (g/dL) | 3.8 (3.5-4.0) | 3.6 (3.3-4.0) | 3.8 (3.5-4.0) | 3.8 (3.5-4.1) | <0.001 |
| WBC count, median (IQR) (x10 3 /μL) | 9.4 (7.6-11.9) | 9.5 (7.6-12.2) | 9.4 (7.6-11.8) | 9.4 (7.5-11.8) | 0.40 |
| STEMI | n = 2,820 | (n = 550) | (n = 1,306) | (n = 964) | P – Value |
|---|---|---|---|---|---|
| Hs-CRP, median (IQR) (mg/L) | 21.1 (9.0-59.3) | 28.9 (12.0-85.0) | 20.0 (8.6-49.2) | 20 (8.4-59.5) | <0.001 |
| Albumin, median (IQR) (g/dL) | 3.7 (3.4-4.0) | 3.5 (3.2-3.9) | 3.7 (3.4-4.0) | 3.8 (3.5-4.0) | <0.001 |
| WBC count, median (IQR) (x10 3 /μL) | 10.9 (8.8-13.3) | 10.9 (8.6-13.6) | 10.8 (8.8-13.3) | 11.0 (8.8-13.3) | 0.88 |
| NSTE-ACS | n = 3,314 | (n = 586) | (n = 1,503) | (n = 1,225) | P – Value |
|---|---|---|---|---|---|
| Hs-CRP, median (IQR) (mg/L) | 9.4 (4.1-22.7) | 12.2 (4.8-32.1) | 9.2 (3.8-21.2) | 8.9 (4.1-22.0) | <0.001 |
| Albumin, median (IQR) (g/dL) | 3.8 (3.5-4.1) | 3.7 (3.4-4.0) | 3.8 (3.6-4.1) | 3.8 (3.5-4.1) | <0.001 |
| WBC count, median (IQR) (x10 3 /μL) | 8.4 (6.9-10.3) | 8.5 (7.0-10.4) | 8.4 (6.9-10.2) | 8.4 (6.9-10.2) | 0.36 |
Moreover, the levels of hs-CRP and WBC count in patients with STEMI were higher than in those patients with NSTE-ACS (p <0.001). In contrast, serum albumin levels were significantly lower in patients with STEMI than in those with NSTE-ACS (p <0.001) ( Table 3 ). In addition, the levels of HDL-C were lower in the STEMI, compared with the NSTE-ACS group (median 36 [IQR 31 to 42] vs 37 [31 to 43] mg/dl, respectively, p = 0.006).
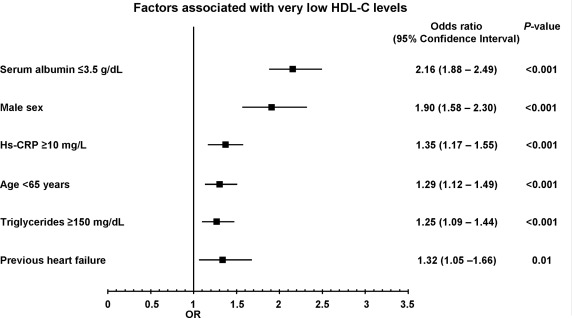
In the overall study population, the univariate analysis showed that serum albumin levels of ≤3.5 mg/dl (odds ratio [OR] 2.07, 95% confidence interval [CI] 1.81 to 2.37, p <0.001) and hs-CRP levels of ≥10 mg/L (OR 1.57, 95% CI 1.37 to 1.80, p <0.001) were associated with very low HDL-C levels, along with male gender, age <65 years, history of current smoking, diabetes, heart failure, renal dysfunction (glomerular filtration rate ≤30 ml/min on admission), body mass index ≥30 kg/m 2 , and TG levels of ≥150 mg/dl. WBC count was not associated with very low HDL-C levels (OR 1.03, 95% CI 0.91 to 1.18, p = 0.58).
The multivariate analysis showed that serum albumin levels of ≤3.5 mg/dl (OR 2.16, 95% CI 1.88 to 2.49, p <0.001) and hs-CRP levels of ≥10 mg/L (OR 1.35, 95% CI 1.17 to 1.55, p <0.001) remained independently associated with very low HDL-C levels, along with male gender, age <65 years, previous heart failure, and TG levels of ≥150 mg/dl ( Figure 3 ). In contrast, for separate regression models for STEMI and NSTE-ACS groups, serum albumin levels of ≤3.5 mg/dl and hs-CRP levels of ≥10 mg/L remained associated with very low HDL-C levels ( Table 4 ).
| Independent predictors | Odds ratio | 95% Confidence Interval | P- Value |
|---|---|---|---|
| STEMI | |||
| Serum albumin ≤3.5 g/dL | 2.31 | 1.90 to 2.82 | <0.001 |
| Men | 1.61 | 1.21 to 2.16 | 0.001 |
| Hs-CRP ≥10 mg/L | 1.40 | 1.11 to 1.76 | 0.005 |
| Current smoker | 1.25 | 1.03 to 1.52 | 0.02 |
| NSTE-ACS | |||
| Men | 2.18 | 1.70 to 2.79 | <0.001 |
| Serum albumin ≤3.5 g/dL | 1.97 | 1.61 to 2.42 | <0.001 |
| Age < 65 years | 1.42 | 1.17 to 1.73 | <0.001 |
| Hs-CRP ≥10 mg/L | 1.35 | 1.12 to 1.63 | 0.002 |
| TG ≥150 mg/dL | 1.33 | 1.10 to 1.61 | 0.002 |
| Previous heart failure | 1.40 | 1.07 to 1.83 | 0.01 |
Although our study was not designed for the analysis of mortality, in the overall study population, the in-hospital mortality rate was higher in patients with very low HDL-C levels than in those with low and normal HDL-C levels (7.0% vs 2.9% vs 3.0%, respectively, p <0.001). Similar differences were observed in the STEMI (10.9% vs 4.3% vs 4.8%, respectively, p <0.001) and NSTE-ACS (3.4% vs 1.7% vs 1.6%, respectively, p = 0.01) groups. In unadjusted analysis, very low HDL-C levels were associated with a 2.47-fold increase in the in-hospital mortality risk compared with patients from other HDL-C categories. After adjustment for age, gender, hs-CRP, serum albumin, and WBC count, an increased risk for death persisted ( Table 5 ).



