The population of adults with congenital heart disease (ACHD) in the United States is growing rapidly with concomitant increases in care costs. We sought to define the variables having the greatest influence on annual cost of inpatient care in patients with ACHD in the United States. To do so, we conducted a retrospective analysis of admissions in patients >18 years old with a 3-digit International Classification of Disease, Ninth Revision , code of 745 to 747 from the State Inpatient Databases of Arkansas (2008 to 2010), California (2003 to 2012), Florida (2005 to 2012), Hawaii (2006 to 2010), Nebraska (2003 to 2011), and New York (2005 to 2012). We selected variables we believed would have the greatest effect on care costs and built a series of multivariable regression models grouping patients by congenital lesion to examine the relative contribution of the specified variables to total annual inpatient cost. We analyzed a total of 68,314 patients aged 57 ± 18.6 years, 51% of whom were women. The multivariable regression model had an overall R 2 of 0.35. Readmission was responsible for 10.3% of annual inpatient cost among all patients with ACHD and had the greatest effect on inpatient care cost for each congenital lesion except Eisenmenger syndrome and conotruncal abnormalities, for both of which it was the second most significant contributor. Other major contributors to annual inpatient care costs included length of stay and operative procedures. In conclusion, rehospitalization is the most significant contributor to annual inpatient cost for individual patients with ACHD in the United States, regardless of underlying anatomy.
A part of the recent increase in health care cost attributable to cardiovascular disease is due to growth in the adult congenital heart disease (ACHD) population . As the size of the ACHD population has increased, so too have inpatient health care expenditures associated with provision of their care. With aging of this population, there is evidence that the importance of ACHD as a contributor to overall US health care expenditures will continue to increase. The first step in decreasing costs and improving efficiency in ACHD care is the identification of high-yield targets for intervention. In the present study, we examined the contribution of several variables to annual inpatient cost in patients with ACHD, with the goal of better understanding which have the greatest influence on inpatient spending in this population.
Methods
For this analysis, we used State Inpatient Databases (SID) that are part of the Healthcare Cost and Utilization Project. We specifically used the SIDs for Arkansas (2008 to 2010), California (2003 to 2012), Florida (2005 to 2012), Hawaii (2006 to 2010), Nebraska (2003 to 2011), and New York (2005 to 2012). We selected these SIDs because they uniquely track hospitalizations in individual patients longitudinally, whereas data from other states track hospitalizations without tracking patients. The dates used were the most complete and up to date available at the time of analysis in April 2015. The primary outcome was financial burden accrued over a 12-month period for care of individual patients with ACHD in the states investigated. The present study was approved by the institutional review board at the Washington University School of Medicine.
As a first step, we identified patients in the databases with ACHD by selecting patients in the SIDs with an age >18 years and with a 3-digit International Classification of Disease, Ninth Revision, diagnosis code of 745 (bulbus cordis anomalies and anomalies of cardiac septal closure), 746 (other congenital anomalies of heart), or 747 (other congenital anomalies of circulatory system). To this group of patients, we applied a validated hierarchical algorithm described by Broberg et al to categorize patients based on anatomy. Any patients who failed to be classified according to this algorithm were excluded to increase the probability that all patients included in fact had ACHD. We then excluded patients with an index hospitalization within the first or last 12 months of the investigated period, so that we were certain that the index hospitalization was not a rehospitalization following one to which we were blind and that a full 12-month follow-up post-index was available for every patient. We excluded all patients for whom there was no cost data available and trimmed the top and bottom 1% of patients based on total annual cost as likely to be outliers. This treatment of the data resulted in a total of 68,314 patients whose data were analyzed.
We next identified clinical and demographic characteristics that we thought were likely to have the greatest impact on inpatient care costs in ACHD. We then compared the prevalence of these variables in patients above versus below the overall median cost using Student’s 2-sample t test and chi-square tests for continuous and categorical data, respectively. Using these data, we further narrowed the list of variables to be included in our model. The final list of variables derived in this manner included hospital readmission within 12 months, age, gender, length of stay, operative procedures, bacterial infection, diabetes without complications, anemia, coagulopathy, hypertension with complications, coronary artery disease, pulmonary vascular disease, arrhythmia, congestive heart failure, peripheral vascular disease, reactive airway disease, acute renal failure, chronic kidney disease, complications of medical or surgical procedures, and aortic valve surgery.
Comparisons of length of stay and cost at the time of index admission between patients who were and were not readmitted were compared using t tests. All significance tests were 2 sided with type I error set to 5%, that is, α = 0.05.
We next constructed a series of multivariable regression models to examine our primary outcome of interest: total cost. Total cost was defined as the index cost and, if readmission occurred, the summed cost of all readmissions within 1 year of the index visit. A different model for each congenital lesion group was constructed using the same set of pre-identified variables. We looked specifically at the eta-squared statistic and p value for each independent variable in each model to see the proportion of total cost for which each variable was responsible across all congenital lesion groups. The sample size of each model changed because of the varying number of subjects in each group. The reference value is zero (“no”) for each dichotomous variable included in the models. The eta-squared statistics, 95% confidence intervals, and p-values were reported from these models, and all significance tests were 2 sided with type I error set to 5%, that is, α = 0.05. All analyses conducted in SAS, v9.4 (SAS Institute Inc., Cary, North Carolina).
Results
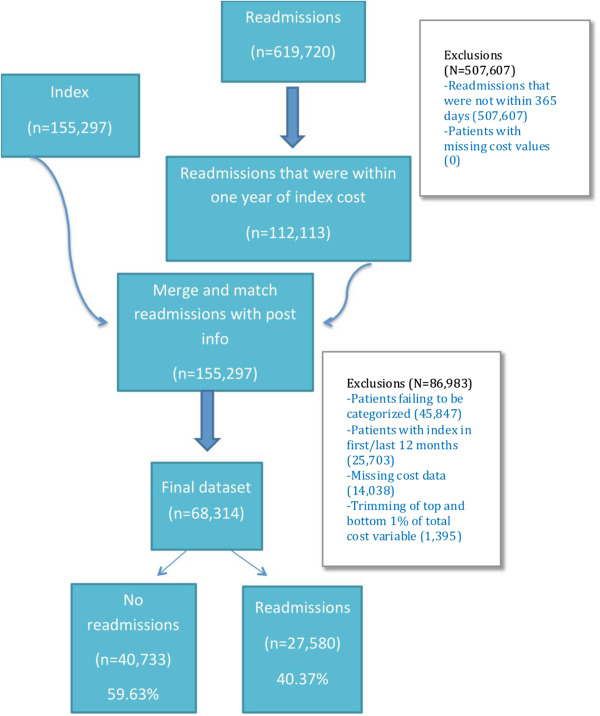
Our initial query of the SIDs resulted in 155,297 index admissions and 619,720 readmissions in patients >18 years with a 3-digit International Classification of Disease, Ninth Revision , code of 745, 746, or 747. After applying exclusion criteria, a final sample size of n = 68,314 patients was achieved as graphically depicted in Figure 1 . Demographic information for the study population may be found in Table 1 . A total of 27,580 patients experienced at least 1 readmission within 12 months of any index admission, whereas 40,733 did not. Patients who experienced a readmission had a 1.7 days longer average length of stay at the time of their index admission (6.7 vs 8.4 days; 95% confidence interval 1.75 to 2.03, p <0.001) but had lower costs at the time of their index admission ($23,037 vs $22,476, p <0.001). The average cost of a readmission was $15,863 ± $20,186 and the average length of stay at readmission was 6.3 ± 12.6 days. The average number of readmissions among patients who were readmitted was 2.0 ± 1.7 and 90% of readmissions were unplanned, whereas 85% of index admissions were unplanned. The cost of an unplanned readmission was $15,573 ± $20,031, whereas the cost of a planned readmission was $18,077 ± $20,759.
| Variable | N=68314 |
|---|---|
| Age at index admission | 57.2±18.6 |
| Female | 34,581 (51%) |
| Homeless | 475 (1%) |
| White | 47,146 (70%) |
| Black | 6,188 (9%) |
| Hispanic | 8,506 (12%) |
| Asian/Pacific islander | 2,291 (3%) |
| Native American | 174 (0%) |
| Other | 2,618 (4%) |
| Primary Payer | |
| Medicare | 28,875 (42%) |
| Medicaid | 8,524 (12%) |
| Private Insurance | 25,758 (38%) |
| Self-pay | 2,395 (4%) |
| No charge | 497 (1%) |
| Other | 2,259 (3%) |
| Cardiac Lesion | |
| Eisenmenger syndrome | 230 (<1%) |
| Single Ventricle | 1,452 (2%) |
| Transposition of the great arteries | 1,110 (2%) |
| Conotruncal abnormality | 521 (1%) |
| Atrioventricular canal defect | 534 (1%) |
| Ebstein anomaly | 484 (1%) |
| Pulmonary stenosis | 1,573 (2%) |
| Anomalous pulmonary venous return | 45 (0%) |
| Coarctation | 978 (1%) |
| Shunts | 46,039 (67%) |
| Subaortic stenosis | 455 (1%) |
| Congenital aortic stenosis | 10,840 (16%) |
| Anomalous coronary artery | 6,058 (9%) |
| Other congenital anomaly | 4,517 (7%) |
| Surgical operation during follow-up | 14,414 (40%) |
| Atrial septal defect repair | 8,347 (12%) |
| Ventricular septal defect repair | 446 (1%) |
| Mitral valve operation | 2,668 (4%) |
| Aortic valve operation | 7,158 (10%) |
| Tricuspid valve operation | 533 (1%) |
| Pulmonary valve operation | 358 (1%) |
| Electrophysiology study/ablation | 1,898 (3%) |
| Permanent pacemaker/Implantable cardiac defibrillator | 2,828 (4%) |
| Ventricular assist device (percutaneous) | 23 (0%) |
| Heart transplant | 41 (0%) |
| Heart/Lung transplant | 4 (0%) |
| Totally anomalous pulmonary venous connection repair | 38 (0%) |
| Atrioventricular canal defect repair | 94 (0%) |
| Tetralogy of Fallot repair | 22 (0%) |
| Transposition of the great arteries repair | 22 (0%) |
| Atriopulmonary Fontan | 29 (0%) |
| Total cavo-pulmonary anastomosis Fontan | 23 (0%) |
| Systemic-pulmonary arterial shunt | 6 (0%) |
| Truncus repair | 3 (0%) |
| Infundibulectomy | 21 (0%) |
Among patients who were not readmitted, 45% had an operation at the time of their index admission, whereas this was the case for only 33% of those who went on to be readmitted. Only 25% of patients who were readmitted underwent an operative procedure at the time of a readmission.
The multivariable regression model derived using the selected variables had an overall R 2 of 0.35. All variables and the magnitude of their contribution to overall annual ACHD inpatient cost can be found in Table 2 .
| Variable | Eta-Square | Variable Rank |
|---|---|---|
| Readmission | 0.1033 | 1 |
| Age | 0.0008 | 13 |
| Sex (Female) | 0.0013 | 11 |
| Length of Stay | 0.0094 | 4 |
| Operative Procedure | 0.0513 | 2 |
| Bacterial Infection | 0.0113 | 3 |
| Diabetes without complications | 0.0004 | 16 |
| Anemia | 0.0023 | 10 |
| Coagulopathy | 0.0033 | 9 |
| Hypertension with complications or secondary | 0.0001 | 18 |
| CAD | 0 | 19 |
| Pulmonary heart disease | 0.0013 | 11 |
| Arrhythmia | 0.0007 | 14 |
| Congestive heart failure | 0.0064 | 8 |
| Peripheral vascular disease | 0.0006 | 15 |
| Reactive airway disease | 0 | 19 |
| Acute renal disease | 0.0069 | 7 |
| Chronic renal disease | 0.0003 | 17 |
| Complications of surgery or medical care | 0.0094 | 4 |
| Aortic valve operation | 0.0082 | 6 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


