Hookah (water pipe) smoking is a major new understudied epidemic affecting youth. Because burning charcoal is used to heat the tobacco product, hookah smoke delivers not only nicotine but also large amounts of charcoal combustion products, including carbon-rich nanoparticles that constitute putative coronary vasoconstrictor stimuli and carbon monoxide, a known coronary vasodilator. We used myocardial contrast echocardiography perfusion imaging with intravenous lipid shelled microbubbles in young adult hookah smokers to determine the net effect of smoking hookah on myocardial blood flow. In 9 hookah smokers (age 27 ± 5 years, mean ± SD), we measured myocardial blood flow velocity (β), myocardial blood volume (A), myocardial blood flow (A × β) as well as myocardial oxygen consumption (MVO 2 ) before and immediately after 30 minutes of ad lib hookah smoking. Myocardial blood flow did not decrease with hookah smoking but rather increased acutely (88 ± 10 to 120 ± 19 a.u./s, mean ± SE, p = 0.02), matching a mild increase in MVO 2 (6.5 ± 0.3 to 7.6 ± 0.4 ml·minute −1 , p <0.001). This was manifested primarily by increased myocardial blood flow velocity (0.7 ± 0.1 to 0.9 ± 0.1 second −1 , p = 0.01) with unchanged myocardial blood volume (133 ± 7 to 137 ± 7 a.u., p = ns), the same pattern of coronary microvascular response seen with a low-dose β-adrenergic agonist. Indeed, with hookah, the increased MVO 2 was accompanied by decreased heart rate variability, an indirect index of adrenergic overactivity, and eliminated by β-adrenergic blockade (i.v. propranolol). In conclusion, nanoparticle-enriched hookah smoke either is not an acute coronary vasoconstrictor stimulus or its vasoconstrictor effect is too weak to overcome the physiologic dilation of coronary microvessels matching mild cardiac β-adrenergic stimulation.
Hookah (water pipe) smoking is a major new understudied epidemic affecting more than 100 million people worldwide. Hookah is increasingly popular among young adults because of the combination of dried fruit and tobacco making a sweet-flavored product, unregulated expansion of hookah cafes near college campuses enabling freshman and sophomores to enjoy the bar scene before the legal alcohol drinking age, and social media claims that the smoke is detoxified as it passes through the water pipe—a spurious belief that is endorsed by most hookah smokers. The smoke contains many chemicals that could acutely alter myocardial blood flow. Nicotine delivery with either medicinal nicotine or cigarette smoking increases blood pressure (BP) and heart rate ; in young adults, the resultant increase in myocardial oxygen demand (MVO 2 ) is matched by a proportional increase in myocardial blood flow. Hookah smoking also acutely increases BP and heart rate —and thus MVO 2 —and decreases heart rate variability (HRV), suggesting sympathovagal imbalance. Because burning charcoal is used to heat the tobacco product, hookah smoke also delivers large amounts of charcoal combustion products, including carbon-rich nanoparticles that constitute putative coronary vasoconstrictor stimuli and carbon monoxide (CO), a known coronary vasodilator. Thus, the goal of this study was to determine the net effect of hookah smoking on myocardial blood flow using myocardial contrast echocardiography (MCE) perfusion imaging.
Methods
The research protocol was approved by the Institutional Review Board at Cedars-Sinai Medical Center. We recruited 28 overtly healthy habitual hookah smokers who do not smoke cigarettes. All subjects provided their written informed consent to participate and agreed to abstain from hookah smoking for 72 hours before study. Inclusion criteria were: age 18 to 39 years; no cardiopulmonary disease; no diabetes; no history of illicit substance use; BP <140/90 mm Hg; BMI <35 kg m 2 ; heart rate at rest <100 beats/min; normal electrocardiogram (ECG) and 2D echocardiogram; and smoked hookah >12 times in the past 12 months. Exclusion criteria (in addition to not meeting inclusion criteria) were: smoked any cigarettes in the past 12 months or >100 cigarettes per lifetime; end-expiratory CO >10 ppm before study (indicating noncompliance with the requisite 72-hour period of hookah abstinence); prescription medication other than oral contraceptives; positive pregnancy test; psychiatric illness; any other condition that the physician investigators deem participation unsafe; and, before the MCE protocol, suboptimal echocardiographic images.
Subjects smoked hookah while seated semi-upright in a custom-built plexiglass smoking chamber, housed in the Cedars-Sinai Hypertension and Vascular Biology Clinical Research Center ( Figure 1 ). A fan within the exhaust system continuously removed air through a vent in the ceiling. Multiple airtight rubber ports on the front and side panels allow wires and tubing to be connected to recording equipment outside the chamber. Subjects rested comfortably on a padded outpatient procedure chair while they smoked ad lib for 30 minutes.
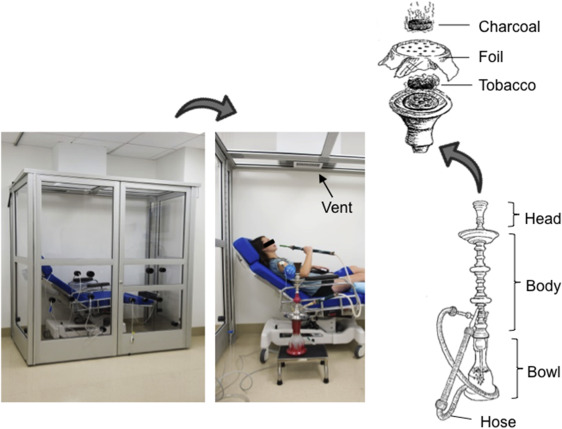
The traditional water pipe ( Figure 1 ) consisted of a chrome body fitted into a glass base with 1,360 ml of water placed into the base. Twelve grams of the most popular brand of hookah tobacco (Starbuzz Tobacco, Inc, Anaheim, California) was placed inside the pipe’s ceramic head, which was covered with a piece of aluminum foil. The aluminum foil was perforated using a “screen pincher,” which standardized the number and size of holes in the foil. The tobacco was then heated with 2 20 × 20–mm natural charcoal briquettes (Coco Nara 100% Natural Coal).
Heart rate was measured continuously before, during, and after the 30-minute hookah smoking sessions and recorded/displayed in real time using a PowerLab A-D Converter (ADInstruments, Colorado Springs, Colorado). Heart rate was measured by a cardiotachometer triggered by the R wave of the ECG and recorded at 1,000 Hz. BP was measured using a validated oscillometric sphygmomanometer (Datascope Mindray Passport V, Mindray North America, Mahwah, New Jersey). Respiratory excursions were monitored with a pneumobelt placed around the thorax (Pneumotrace; UFI, Morro Bay, California) to measure respiratory rate before and immediately after hookah smoking.
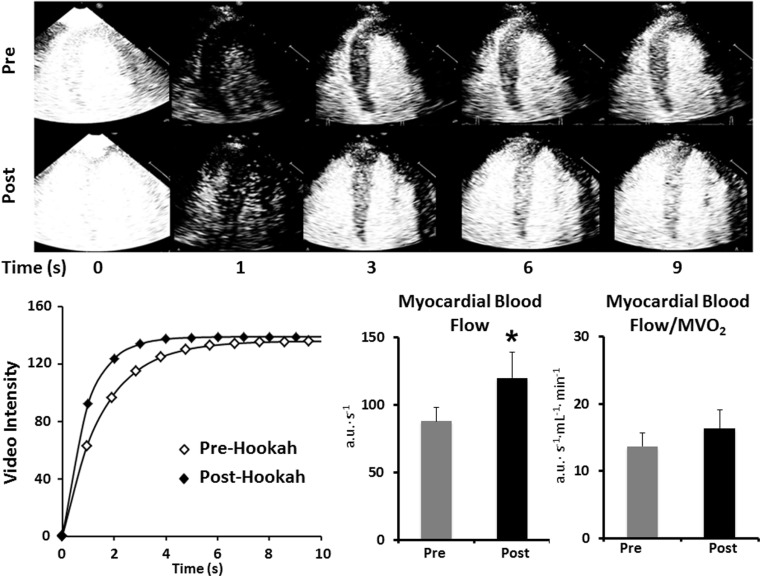
MCE was performed with continuous intravenous (i.v.) infusion of lipid-shelled perflutren-containing microbubbles by one experienced sonographer (XT) as previously described, using proved methods to minimize variability. Contrast-enhanced 2-dimensional transthoracic echocardiography was performed using a phased-array probe interfaced with an imaging system (iE33; Philips Medical Systems, Andover, Massachusetts). One vial (1.3 ml) of lipid-shell octafluoropropane microbubbles (Definity; Lantheus Medical Imaging, North Billerica, Massachusetts) was diluted to a total volume of 30 ml in normal saline solution and administered intravenously with an infusion pump (Medfusion 3500 Syringe Pump; Smiths Medical ASD Inc, St. Paul, Minnesota) at a rate of 1.0 ml/min. After myocardial Definity concentration reached steady state, microbubbles within the imaging sector were destroyed with a high (0.8) mechanical index ultrasound pulse, and the rate of replenishment was interrogated with low (0.1) mechanical index imaging. Only end-systolic frames were used for analysis. Gain, depth, transmit focus, and postprocessing were optimized at the beginning of the study and held constant throughout. Imaging was performed in the apical 4-chamber view, with the septum focused in the middle of the window.
Image analysis was performed offline by a single experienced operator (SS) using an established method. Briefly, a large region of interest was placed over the midventricular septum of 10 to 15 consecutive end-systolic images beginning with the immediate postdestruction frame. Plots of time versus background-subtracted acoustic intensity were then generated and fit to the exponential function y = A (1−e βt ), where y is the acoustic intensity at time (t), A is the plateau where acoustic intensity represents myocardial blood volume, and β is the mean microbubble (i.e., blood flow) velocity through the microcirculation (referred to as myocardial blood flow velocity and expressed in acoustic intensity units per second). Data are reported as the mean of 3 separate plots of microbubble destruction, refill time versus acoustic intensity, each satisfying all the following criteria: (1) adequate destruction of microbubbles after high mechanical index pulse by visual inspection; (2) focus of the septum in the middle of the window throughout the entire destruction-refill observation period; and (3) a consistent imaging plane. Myocardial blood flow was calculated as the product of myocardial blood volume (A) and blood flow velocity (β). In our laboratory, the coefficient of variation is 3% for myocardial A, and 13% for both myocardial β and myocardial perfusion (A·β), documenting test–retest reproducibility.
To evaluate left ventricular (LV) systolic function and to estimate cardiac work as a reflection of MVO 2 , we performed contrast-enhanced imaging in both the parasternal and apical widows. Apical 4-chamber and 2-chamber images were acquired, with the endocardial surface traced manually at end diastole and end systole for measurement of LV end-diastolic and end-systolic volumes, respectively, using the modified Simpson method. All data were reported as the average of at least 3 cardiac cycles acquired with the breath held at end expiration. Stroke volume was calculated as end-diastolic volume subtracted by the end-systolic volume, and cardiac output was calculated as the heart rate multiplied by the stroke volume. Ejection fraction was calculated as stroke volume divided by end-diastolic volume. LV end-systolic single point elastance was calculated as end-systolic pressure (0.9 × systolic BP) divided by end-systolic volume. MVO 2 was calculated as the rate pressure product by the validated equation: (7.2 × 10 −4 ) × (heart rate × systolic BP) + 1.42 and also reflected in total myocardial work: (heart rate × systolic BP × stroke volume).
To parse sympathetic versus parasympathetic mediation of the increase in MVO 2 evoked by hookah, we used 2 complementary approaches: (1) HRV and, in a subset of subjects, and (2) i.v. propranolol at a dose (0.2 mg/kg) that provides near-maximal steady-state β-adrenergic blockade for ≥60 minutes. The HRV was derived from the continuous ECG according to recommended standards using LabChart software (LabChart 7.0, ADInstruments). Mean values were calculated for 5 consecutive minutes before and immediately after hookah smoking. Time and frequency domain measurements were calculated by established standards, which state that vagal activity is the major contributor to high frequency component (HF 0.15 to 0.40 Hz) and that disagreement exists with respect to the low frequency component (LF 0.04 to 0.15 Hz), with some studies suggesting that LF, when normalized for total power, is a quantitative marker of sympathetic control of heart rate, whereas others view LF as reflecting both sympathetic and vagal activity. Thus, ratio of LF to HF power is considered to reflect sympathovagal balance.
Expired CO and plasma nicotine concentrations were measured immediately before and after 30 minutes of hookah smoking to characterize the smoking exposure. End-tidal CO was measured with a CO meter (Micro Smokerlyzer; Bedfont Scientific Ltd.; Kent, United Kingdom). Plasma nicotine levels were assayed in the Clinical Pharmacology Laboratory at San Francisco General Hospital by gas chromatography with nitrogen-phosphorus detection, using 5-methylnicotine and 1-methyl-5-(2-pyridyl)-pyrrolidin-2-one (“ortho-cotinine”) as internal standards. This method has been modified for simultaneous extraction of nicotine with determination using capillary gas chromatography. The limits of quantitation are 1 ng/ml for nicotine.
We used paired t tests for comparisons between data obtained before and after 30 minutes of hookah smoking. Data were considered statistically different when p <0.05; there was no adjustment for testing of multiple variables. Results are reported as mean ± SE, unless otherwise specified.
Results
Of 55 potential subjects who were screened for participation, 27 were excluded for the following reasons: suboptimal echocardiographic image quality for MCE (n = 10); exhaled CO >10 ppm on screening (n = 2); a history of cigarette smoking (n = 8); and a medical history of chronic systemic illness including asthma or diabetes (n = 7). The characteristics of the remaining 28 study subjects are presented in Table 1 . This racially diverse group of young adults, including 8 women and 20 men, had a mean age of 27 years (range, 19 to 39 years). They smoked hookah on average twice weekly, with each session lasting on average 102 minutes (range, 60 to 240 minutes).
| Variable | N or mean ± SD |
|---|---|
| Female/ Male | 8/20 |
| Age (years) | 27 ± 5 |
| Body Mass Index (kg·m 2 ) | 25.0 ± 4.0 |
| Non-Hispanic White | 9 |
| Non-Hispanic Black | 14 |
| Hispanic | 1 |
| Asian | 1 |
| Native Hawaiian/ Pacific Islander | 1 |
| Middle-Eastern Origin | 2 |
| Level of Education Attained | |
| High school | 6 |
| College | 20 |
| Graduate | 2 |
| Hookah Smoking History | |
| Number of Hookah Sessions per week | 2 ± 2 |
| Session Duration (minutes) | 102 ± 60 |
| Age of Hookah Smoking Onset (years) | |
| ≤ 17 | 5 |
| 18-24 | 19 |
| 25-29 | 3 |
| 30-39 | 1 |
In total, we tested acute effects of hookah smoking on: (1) myocardial perfusion imaging by MCE and 2-dimensional echocardiographic indexes of LV systolic function in the 9 subjects with optimal echocardiographic image quality and (2) HRV—because of its inherently large intersubject variability—in 21 subjects, of whom, 4 returned on a separate day to repeat the protocol after β-adrenergic blockade with i.v. propranolol. Two subjects participated in both MCE and HRV protocols. Heart rate and BP were measured in all subjects.
The effect of hookah smoking on myocardial blood flow is presented in Table 2 and Figure 2 . In these subjects, myocardial blood flow velocity increased, whereas myocardial blood volume remained unchanged. As a result, myocardial blood flow (and conductance) increased by 36%. The ratio of myocardial perfusion to MVO 2 was unaffected by hookah smoking, indicating proportionate increases in oxygen delivery and demand. Hookah smoking had no effect on several systolic phase indexes, including LV ejection fraction, LV end-systolic elastance, or LV stroke work, whereas LV total work increased modestly ( Table 2 ).
| Pre-Hookah | Post-Hookah | p-value | |
|---|---|---|---|
| Myocardial Contrast Echocardiography | |||
| Myocardial A, a.u. | 133 ± 7 | 137 ± 7 | 0.45 |
| Myocardial β, s -1 | 0.7 ± 0.1 | 0.9 ± 0.1 | 0.01 |
| Myocardial blood flow (A·β), a.u.·s -1 | 88 ± 10 | 120 ± 19 | 0.02 |
| Myocardial conductance, a.u.·mmHg -1 | 1.1 ± 0.2 | 1.5 ± 0.3 | 0.04 |
| Myocardial blood flow /MVO2, a.u.· s -1 ·mL -1 · min -1 | 14 ± 2 | 16 ± 3 | 0.18 |
| Conductance/ MVO2, a.u.·mmHg -1 ·ml·min -1 | 0.2 ± 0.03 | 0.2 ± 0.04 | 0.28 |
| Indices of LV work and Oxygen Demand | |||
| LV Stroke volume, mL | 66 ± 5 | 66 ± 4 | 0.93 |
| LV End-systolic volume, mL | 41 ± 4 | 39 ± 2 | 0.55 |
| LV End-diastolic volume, mL | 107 ± 9 | 105 ± 6 | 0.75 |
| LV Ejection Fraction, % | 62 ± 1 | 62 ±1 | 0.74 |
| LV end-systolic elastance, mmHg·mL -1 | 2.7 ± 0.3 | 2.8 ± 0.2 | 0.56 |
| LV stroke work (x10 -3 ), mmHg·mL -1 | 2.9 ± 0.5 | 2.6 ± 0.3 | 0.45 |
| LV total work, mmHg·mL -1 ·beats.min -1 | 166.2 ± 22 | 202.3 ± 23 | 0.02 |
| MVO 2 , ml·min -1 | 6.48 ± 0.24 | 7.60 ± 0.38 | 0.001 |
| Hemodynamics | |||
| Heart Rate. beats·min -1 | 62 ± 2 | 71 ± 4 | 0.01 |
| Systolic Blood Pressure, mmHg | 114 ± 4 | 122 ± 5 | 0.01 |
| Diastolic Blood Pressure, mmHg | 62 ± 3 | 66 ± 5 | 0.07 |
| Mean Arterial Pressure , mmHg | 79 ± 3 | 84 ± 5 | 0.01 |
| Cardiac Output, L·min -1 | 4.0 + 0.3 | 4.6 + 0.3 | 0.02 |
| Systemic Vascular Resistance, dyn·s/cm 5 | 1679 ± 172 | 1503 ± 128 | 0.17 |

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


