Many cardiac conditions cause electrical impulses to be conducted abnormally through the ventricular myocardium, producing changes in QRS complexes and T waves. Therefore, it is important to understand the conditions that can mimic or complicate the diagnosis of bundle-branch block (BBB) or fascicular block (intraventricular conduction abnormalities). These are as follows:
1. The left and right ventricles are not in an enlarged state that would prolong the time required for their activation and recovery (see Chapter 5).
2. Myocardial ischemia or infarction is not present or is of insufficient magnitude to disrupt the spread of the activation and recovery waves (see Chapter 9).
3. There is rapid impulse conduction through the right- and left-ventricular Purkinje networks so that the endocardial surfaces are activated almost simultaneously (as discussed later in this chapter).
4. There are no accessory pathways for conduction from the atria to the ventricles (see Chapter 7).
BUNDLE-BRANCH AND FASCICULAR BLOCKS 
Because the activation of the ventricular Purkinje system is not represented on the surface electrocardiogram (ECG), abnormalities of its conduction must be detected indirectly by their effects on myocardial activation and recovery. ECG waveforms (see Fig. 1.14) are reproduced with the addition of specific QRS complex abnormalities in Figure 6.1. A conduction disturbance within the right bundle branch (RBB) causes right-ventricular activation to occur after left-ventricular activation is completed, producing an R′ deflection in lead V1 (see Fig. 6.1). A delay in conduction through the left bundle branch (LBB) markedly postpones left-ventricular activation, resulting in an abnormally prominent S wave in lead V1 (see Fig. 6.1).

Conduction delays in the left-bundle fascicles or between the Purkinje fibers and the adjacent myocardium may alter the QRS complex and T wave (Fig. 6.2). A conduction disturbance in the common bundle (Bundle of His) has similar effects on the entire distal Purkinje system and therefore does not alter the appearance of the QRS complex or T wave.
Block of an entire bundle branch requires that its ventricle be activated by myocardial spread of electrical activity from the other ventricle, with prolongation of the overall QRS complex. Block of the entire RBB is termed “complete right-bundle-branch block” (RBBB), and block of the entire LBB is termed “complete left-bundle-branch block” (LBBB). In both of these conditions, the ventricles are activated successively instead of simultaneously. The other conditions in which the ventricles are activated successively occur when one ventricle is preexcited via an accessory atrioventricular (AV) pathway (see Chapter 7) and when there are independent ventricular rhythms (see Chapters 15 and 19). Under these conditions, there is a fundamental similarity in the distortions of the ECG waveforms: the duration of the QRS complex is prolonged and the ST segment slopes into the T wave in the direction away from the ventricle in which the abnormality is located. Figure 6.3 compares QRS morphologies in lead V1 when the two ventricles are activated successively rather than simultaneously.
A ventricular conduction delay with only slight prolongation of the QRS complex due to slowed conduction through the bundle branches could be termed incomplete RBBB or incomplete LBBB. However, it is important to remember from Chapter 5 that enlargement of the right ventricle may produce a distortion of the QRS complex that mimics incomplete RBBB (see Fig. 5.10B), whereas enlargement of the left ventricle may produce a prolongation of the QRS complex that mimics incomplete LBBB (see Fig. 5.9A). Because the LBB has multiple fascicles, another form of incomplete LBBB could be produced by a disturbance in one of its major fascicles.
The ventricular Purkinje system is considered trifascicular. It consists of the RBB and the anterior and posterior portions of the LBB. The proximal RBB is small and compact and may therefore be considered either a bundle branch or a fascicle. The proximal LBB is also compact but is too large to be considered a fascicle. It remains compact for 1 to 2 cm and then fans into its two fascicles.1 As Demoulin and Kulbertus2 have shown in humans, there are multiple anatomic variations in these fascicles among individuals. The left ventricle has been opened (Fig. 6.4) to reveal the LBB and its fascicles as originally presented in Figure 1.7C. Note the anterior and posterior fascicles of the LBB are also designated superior and inferior, respectively, because these terms indicate their true anatomic positions. Based on their anatomic locations, the two fascicles are termed the left anterior fascicle (LAF) and left posterior fascicle (LPF; see Fig. 6.4). The LAF of the LBB courses toward the anterosuperior papillary muscle, and the LPF of the LBB courses toward the posteroinferior papillary muscle. There are also Purkinje fibers that emerge from the LBB that proceed along the surface of the interventricular septum (sometimes termed the left septal fascicle) and initiate left-to-right spread of activation through the interventricular septum.
Rosenbaum and coworkers3 described the concept of blocks in the fascicles of the LBB, which they termed “left anterior and left posterior hemiblock.” However, these two kinds of block are more appropriately termed left anterior fascicular block (LAFB) and left posterior fascicular block (LPFB). Isolated LAFB, LPFB, or RBBB is considered unifascicular block. Complete LBBB or combinations of RBBB with LAFB or with LPFB are bifascicular blocks, and the combination of RBBB with both LAFB and LPFB is considered trifascicular block.
The term unifascicular block is used when there is ECG evidence of blockage of only the RBB, LAF, or LPF. Isolated RBBB or LAFB occur commonly, whereas isolated LPFB is rare. Rosenbaum and coworkers3 identified only 30 patients with LPFB, as compared with 900 patients with LAFB.
Right-Bundle-Branch Block
Because the right ventricle contributes minimally to the normal QRS complex, RBBB produces little distortion of the QRS complex during the time required for left-ventricular activation. Figure 6.5 illustrates the minimal distortion of the early portion and marked distortion of the late portion of the QRS complex (in lead V1) that typically occurs with RBBB. The activation sequence of the interventricular septum and the right- and left-ventricular free walls contribute to the appearance of the QRS complex in lead V1 (see Fig. 6.5). Normal intraventricular conduction requires only two sequential 0.04-second periods, whereas a third is required when RBBB is present. The minimal contribution of the normal right-ventricular myocardium is completely subtracted from the early portion of the QRS complex and then added later, when the right ventricle is activated after the spread of impulses from the left ventricle through the interventricular septum to the right ventricle. This produces a late prominent positive wave in lead V1 termed R′ because it follows the earlier positive R wave produced by the normal left-to-right spread of activation through the interventricular septum (see Fig. 6.5; Table 6.1).
RBBB has many variations in its ECG appearance (Fig. 6.6A–C). In Figure 6.6A, the RBBB is considered “incomplete” because the duration of the QRS complex is only 0.10 second; but in Figure 6.6B and C, the RBBB is considered “complete” because the duration of the QRS complex is ≥0.12 second.

Left Fascicular Blocks
Normal activation of the left-ventricular free wall spreads simultaneously from two sites (near the insertions of the papillary muscles of the mitral valve). Wavefronts of activation spread from these endocardial sites to the overlying epicardium. Because the wavefronts travel in opposite directions, they neutralize each other’s influence on the ECG in a phenomenon called cancellation. When a block in either the LAF or LPF is present, activation of the free wall proceeds from one site instead of two. Because the cancellation is removed, the waveforms of the QRS complex change, as described below (Tables 6.2 and 6.3). A schematic diagram of the left ventricle viewed from its apex upward toward its base is illustrated in Figure 6.7.
Left Anterior Fascicular Block
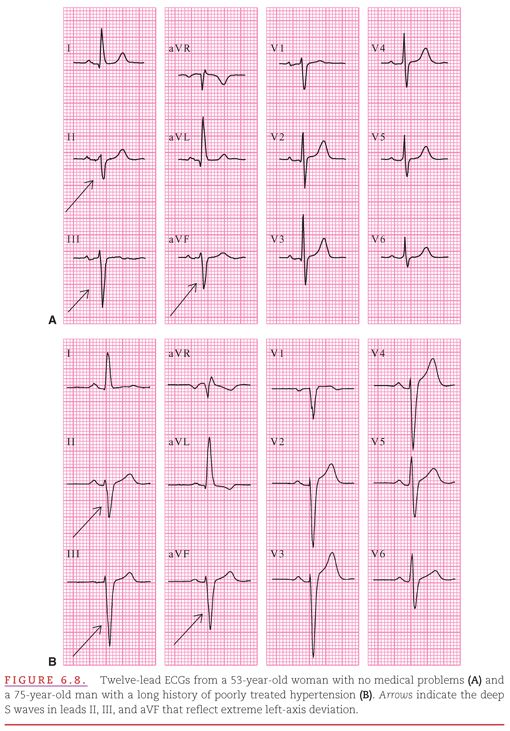
If the LAF of the LBB is blocked (see Fig. 6.7B), the initial activation of the left-ventricular free wall occurs via the LPF. Activation spreading from endocardium to the epicardium in this region is directed inferiorly and rightward. Because the block in the LAF has removed the initial superior and leftward activation, a Q wave appears in leads that have their positive electrodes in a superior-leftward position (i.e., lead I) and an R wave appears in leads that have their positive electrodes in an inferior-rightward position (i.e., lead aVF) (see Fig. 6.8). Following this initial period, the activation wave spreads over the remainder of the left-ventricular free wall in a superior-leftward direction, producing a prominent R wave in lead I and a prominent S wave in lead aVF. This change in the left-ventricular activation sequence produces a leftward shift of the axis of the QRS complex to at least −45 degrees. The overall duration of the QRS complex may be within the normal range but is usually prolonged by 0.02 second from the patient’s baseline.4
Left Posterior Fascicular Block
If the LPF of the LBB is blocked (see Fig. 6.7C), the situation is reversed from that in LAF block, and the initial activation of the left-ventricular free wall occurs via the LAF. Activation spreading from the endocardium to the epicardium in this region is directed superiorly and leftward. Because the block in the LPF has removed the initial inferior and rightward activation, a Q wave appears in leads with their positive electrodes in an inferior-rightward position (i.e., lead aVF) and an R wave appears in leads with their positive electrodes in a superior-leftward direction (i.e., lead I). Following this initial period, the activation spreads over the remainder of the left-ventricular free wall in an inferior/rightward direction, producing a prominent R wave in lead aVF and a prominent S wave in lead I. This change in the left-ventricular activation sequence produces a rightward shift of the axis of the QRS complex to ≥+90 degrees.5 The duration of the QRS complex may be normal or slightly prolonged (Fig. 6.9).

The consideration that LPFB may be present requires that there be no evidence of right-ventricular hypertrophy (RVH) from either the precordial leads (see Fig. 6.9) or from other clinical data. However, even the absence of RVH does not allow diagnosis of LPFB because RVH can produce the same pattern as LPFB in the limb leads and RVH is much more common than LPFB.
The term bifascicular block
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


