Introduction and historical perspective
Cardiovascular diseases (CVD), of which coronary heart disease (CHD) is the most common, are the major causes of death in middle-aged and older people in most developed countries and in many developing countries.1–3 Cardiovascular diseases result in substantial disability worldwide and contribute in large part to the escalating costs of healthcare, especially with an increasing aging population,4 and are predicted to be the leading cause of death and disability-adjusted life-years by 2020.5 A significant proportion of cardiovascular morbidity and mortality could be prevented through population strategies, and by making cost-effective clinical interventions accessible and affordable, both for people with established disease and for those at high risk of developing cardiovascular disease.6,7
This chapter is about integrating clinical approaches to prevention of cardiovascular disease for those with established atherosclerotic disease (secondary prevention) and those who are asymptomatic but at high risk of developing the disease (primary prevention).
The World Heart and Stroke Forum (WHSF) Guidelines Task Force of the World Heart Federation (WHF) recommends that every country develop a national policy on CVD prevention.8 This national policy should set priorities for public health and clinical interventions appropriate to the country, and be the foundation for developing national evidence-based clinical guidelines on CVD prevention.
While the causes of CVD are common to all parts of the world, the approaches to cardiovascular prevention at a societal or individual level will differ between countries for cultural, social, medical, and economic reasons. Although national guidelines will share common principles of CVD prevention – the need for patient priorities, absolute risk thresholds for treatment and treatment targets-they may differ in terms of the organization of preventive cardiology risk factor treatment thresholds and targets, and the availability and use of cardioprotective medications.
The World Health Organization report on prevention of coronary heart disease describes three strategies for prevention,1 which still apply today but for all atherosclerotic cardiovascular disease. These three strategies complement each other:
- a ‘population’ strategy-for altering, in the entire population, the lifestyle and environmental factors, and their social and economic determinants, that are the underlying causes of the mass occurrence of CVD
- a ‘high-risk’ strategy-identification of individuals at high risk of developing the disease, and action to reduce their risk factor levels
- secondary prevention-prevention of disease progression and recurrent cardiovascular events in patients with clinically established coronary or other atherosclerotic disease.
The secondary prevention strategy addresses those who have survived the development of symptomatic atherosclerotic disease-acute coronary syndromes, angina, transient cerebral ischemia, stroke, peripheral arterial disease-with the object of reducing the risk of recurrent cardiovascular events, improving quality of life and life expectancy. However, it is necessarily limited to survivors. The first manifestation of CVD can be sudden collapse and death, e.g. ventricular fibrillation in the context of acute myocardial infarction. In addition, among those who survive the initial ischemic insult, the resulting tissue damage may be so great that secondary prevention offers little gain. This is because prognosis is largely determined by the extent of cardiac or cerebral damage. Therefore, a high-risk primary prevention strategy is required.
The high-risk strategy identifies those asymptomatic individuals in the population who are apparently well but at high multifactorial risk of developing CVD, with the object of reducing their total CVD risk through lifestyle, risk factor and therapeutic management. However, its overall impact on the burden of disease in the population is limited because it only targets those at highest risk whereas the burden of CVD arises in those at modest risk where medical interventions are not appropriate.
Therefore, a population strategy, which tackles the major determinants of cardiovascular diseases at a societal level, is paramount and without such a strategy, these diseases will remain a major cause of ill health and premature death, regardless of the fact that secondary prevention and high-risk strategies do reduce cardiovascular morbidity and mortality for individuals.
Incidence, natural history, and prognosis
Secondary prevention
The first clinical presentation of atherosclerotic disease is with sudden death or, more commonly, a non-fatal event, principally of the coronary arteries, cerebral arteries or peripheral arteries. Whatever the affected arterial territory, the pathology of the disease is the same and is usually ubiquitous. Although the acute management will differ according to the affected arterial territory, the ways of preventing a recurrence are common to all manifestations of atherosclerosis – lifestyle (smoking cessation, eating a healthy diet and being physically active), the management of other risk factors (blood pressure, lipids and glucose) and the use of cardioprotective drugs, some of which have specific clinical indications, e.g. beta-blockers following myocardial infarction, based on evidence from randomized controlled trials.
All patients with atherosclerotic cardiovascular disease should be eligible for a comprehensive prevention program. Traditionally, such programs have focused on patients with coronary disease, especially those following myocardial infarction or revascularization, usually by cardiac surgery. Yet the benefits of prevention demonstrated in those who have had a myocardial infarction are as likely to be achieved in patients with angina pectoris, stroke or other atherosclerotic disease. So the new challenge is to provide preventive cardiology programs for all atherosclerotic disease patients.
High-risk strategy
Primary prevention of CVD in individuals has traditionally focused on single risk factors, such as “hypertension”, rather than multiple risk factors or the total risk approach and as a consequence, the potential benefits of total CVD risk reduction have not been achieved. Although there is a continuous relationship between blood pressure and the risk of developing CVD, the higher the blood pressure, the higher the risk. The term “hypertension” dichotomizes this distribution into those with a blood pressure consistently greater than a specified level, e.g. 140/90 mmHg, and those with a blood pressure less than this level which is commonly referred to as “normal”. The level of blood pressure defining “hypertension” is not based on the epidemiology of blood pressure and cardiovascular risk, but is rather deduced from randomized controlled trials which have shown evidence of benefit through reducing blood pressure in those with levels above, say, 140/90 mmHg. The consequence of this approach is that someone with a blood pressure of 142/92 mmHg is considered to be “hypertensive” and therefore receives blood pressure-lowering therapy, but another person of the same age and sex with a blood pressure of 138/88 mmHg is considered to be “nor-motensive” and therefore requires no treatment. Yet the total risk of developing CVD is not just a function of blood pressure but of all the cardiovascular risk factors taken together which are associated with a given level of blood pressure. This is called total cardiovascular risk. This term is used to describe the probability of a person developing an atherosclerotic cardiovascular event over a defined period of time.
The concept of total CVD risk assessment and management was first advanced by Jackson in 1993 in the context of treating “hypertension”; namely, the indication for treating blood pressure was not just a function of the blood pressure level but rather the absolute CVD risk, based on a combination of all risk factors, of which blood pressure was just one component.9 This was followed in 1994 and 1998 by the Joint European Societies’ recommendations which applied this principle of total coronary risk assessment to the management of all risk factors: blood pressure, lipids and diabetes.10,11 The European CHD risk charts, developed from a concept pioneered by Anderson,12 used age, sex, smoking status, blood cholesterol and SBP to estimate the 10 year risk of a first fatal or non-fatal coronary heart disease event. There were separate European charts for those with and without diabetes.
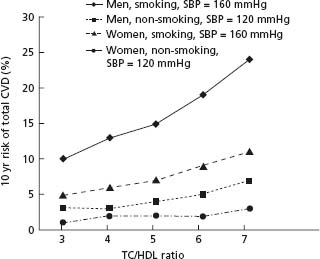
The importance of estimating total CVD risk before making a decision to intervene medically is illustrated in Figure 24.1. The figure illustrates that in a middle-aged man who is a non-smoker with a blood pressure of 120 mmHg, the absolute risk of developing fatal CVD progressively increases as the total cholesterol to HDL-cholesterol ratio rises from 3.0 to 7.0. However, at every level of this lipid ratio the absolute risk for a man of the same age who smokes cigarettes and has raised blood pressure is substantially higher. In fact, the chances of such a man developing CVD with a lipid ratio of 3.0 is actually higher than a lipid ratio of 7.0 in a non-smoking man with lower blood pressure. Although women are usually, age for age, at lower absolute risk of CVD than men, this advantage is lost at any level of the lipid ratio if the woman is a smoker with raised blood pressure.
Figure 24.1 The relationship of total cholesterol/HDL cholesterol ratio to 10-year fatal CVD events in men and women aged 60 years with and without risk factors, based on a risk function derived from the SCORE project. (Reproduced with permission from Graham et al.2)
The third and fourth editions of the Joint European Societies Guidelines published in 2003 and 200713,14 introduced a new system for cardiovascular risk estimation called SCORE (Systematic Coronary Risk Estimation), based on data from 12 European prospective cohort studies: 205,178 subjects with 2.7 million years of follow-up and 7934 cardiovascular deaths.15 Two charts were produced: one for high-risk regions and the other for low-risk regions of Europe (Figs 24.2, 24.3). SCORE estimates the 10-year risk of a first fatal atherosclerotic event, whether heart attack, stroke, aneurysm of the aorta or other fatal manifestation of atherosclerotic disease. All ICD (International Classification of Diseases) codes that could be due to atherosclerosis are included. One advantage of a risk score based on mortality is that it can be recalibrated if good-quality, up-to-date mortality and risk factor prevalence data are available for a country. The SCORE CVD mortality charts have been recalibrated for a number of European countries: Germany, Greece, Poland, Spain, Sweden, Cyprus, Bosnia/ Herzegovina and Russia. The electronic, interactive version of SCORE, called HEARTSCORE, is available from the European Society of Cardiology (www.escardioorg/heartscore).
Figure 24.2 SCORE chart: 10-year risk of fatal CVD in populations at high CVD risk based on the following risk factors: age, gender, smoking, systolic blood pressure and total cholesterol. (Reproduced with permission from Graham et al.2)
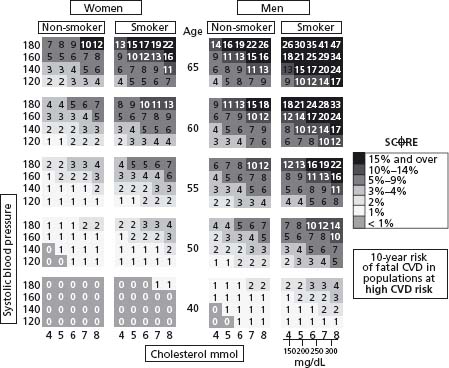
Figure 24.3 SCORE chart: 10-year risk of fatal CVD in populations at low CVD risk based on the following risk factors: age, gender, smoking, systolic blood pressure and total cholesterol. (Reproduced with permission from Graham et al.2)
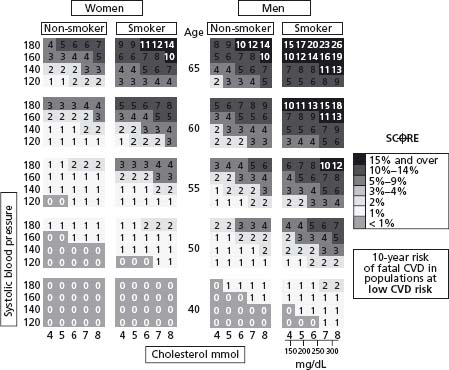
A 10-year CVD risk of 5% or more (red zone) for fatal events was defined in the 2003 Joint European Societies guidelines as high risk, and people at this level of risk should receive a professional lifestyle intervention and, if appropriate, drug therapies to reduce total CVD risk. Although an individual’ s treatment should be guided by their total CVD risk, the physician also needs to take account of other factors, e.g. co-morbidity and life expectancy, before committing a person to lifelong therapies.
In 2007 the WHO developed CVD risk prediction charts because equations derived from Caucasian populations are not necessarily valid to predict CVD risk in low-and middle-income countries.1 The Comparative Risk Assessment (CRA) Project, conducted by the WHO and described in the 2002 World Health Report, determined the burden of disease attributable to selected major risk factors, including smoking, Body Mass Index, high blood pressure, and high blood cholesterol.16 This project involved the standardized collection and assessment of risk factor prevalences by WHO epidemiologic subregion. Estimates of relative risk per unit increase in continuous risk factors, i.e. per mmHg for systolic blood pressure, were determined from the CRA project largely from prospective cohort studies. Absolute risk of a cardiovascular event was determined by scaling individual relative risk to population incidence rates of cardiovascular disease (coronary heart disease and stroke), estimated from the Global Burden of Disease Study. The probability of a cardiovascular event was extrapolated to a 10-year period. The new WHO/International Society of Hypertension (ISH) risk prediction charts are based on these data and there are charts with and without cholesterol, and for patients with and without diabetes.
In summary, the great strength of the total risk approach is that it provides a rational means of making decisions about intervening in a targeted way, thereby making best use of resources available to reduce cardiovascular risk. The traditional approach focused on single risk factors as if they were “diseases” and this way of thinking is still being promoted with the use of terms such as “pre-hypertension” or “pre-diabetes”. Many in the medical profession are reluctant to change from a unifactorial to a total risk approach because of their traditional medical training. The total risk approach also runs counter to the special interests of some professional societies, which focus on single risk factors, and the pharmaceutical industry and regulatory authorities which license drugs for single clinical indications. This unifactorial approach leads to people being labelled as “high risk” and for many this will be incorrect, leading to inappropriate use of drug therapies. In contrast, the total risk approach identifies that section of the population at highest risk of developing CVD. Such individuals have the most to gain from lifestyle and medical interventions to reduce their cardiovascular risk. So CVD risk scoring moves the focus of identification and treatment from individual risk factors to multiple risk factors. The intensity of interventions can then be matched to the level of total CVD risk. Research is required to validate the WHO regional risk prediction charts for each national population, and to confirm that using risk stratification methods in low-and middle-income countries results in benefits for both patients and the population as a whole.
Secondary prevention
Cardiac rehabilitation traditionally focused on physical rehabilitation but this specialty has gradually evolved into more comprehensive professional lifestyle programs – smoking cessation, making healthy food choices and becoming physically active – based on behavioral models of change. Risk factor management in terms of controling blood pressure, lipids and glucose to defined targets, and the use of cardioprotective drug therapies, is also now integral to this approach. Finally, the psychosocial and vocational support required to help patients lead as full a life as possible is also provided. This evolution in cardiac rehabilitation is reflected in the current WHO definition.17
“The rehabilitation of cardiac patients is the sum of activities required to influence favorably the underlying cause of the disease, as well as the best possible physical, mental and social conditions, so that they may, by their own efforts, preserve or resume when lost, as normal a place as possible in the community. Rehabilitation cannot be regarded as an isolated form of therapy but must be integrated with the whole treatment of which it forms only one facet.”
The original definition18 was changed in 1993 with the addition of the following words: “to influence favorably the underlying cause of the disease” – in short, all aspects of CVD prevention.
The overall preventive objective for patients who present with symptoms of coronary artery disease – stable angina, unstable angina or acute MI – is to reduce the risk of a further non-fatal event or death from cardiovascular disease. Cardiac rehabilitation was originally provided only for patients recovering from a myocardial infarction (MI) and those who had coronary artery bypass graft (CABG) surgery (or other forms of cardiac surgery). With the more recent emphasis on influencing the underlying causes of atherosclerotic disease, patients presenting with all forms of coronary artery disease, including unstable and stable angina, are now being included together with those who have other forms of atherosclerotic disease (e.g. transient cerebral ischemia or peripheral arterial disease) in cardiovascular prevention and rehabilitation programs. By addressing all aspects of lifestyle and risk factor management, and prescribing cardioprotective drug therapies, the risk of future cardiovascular events can be reduced in all these patients as evidenced by the meta-analyses.
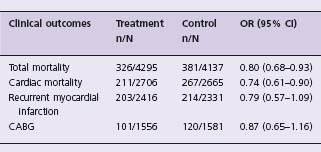
The scientific evidence from randomized controlled trials shows that exercise-based cardiac rehabilitation of coronary patients reduces both total and cardiac mortality. The main objective of the Cochrane systematic reviews and meta-analyses,19 last updated in 2004,20 was to determine the effectiveness of exercise only, or exercise as part of a comprehensive cardiac rehabilitation programme, on total and CHD mortality, morbidity, health-related quality of life (HRQoL) and modifiable cardiac risk factors of patients with coronary heart disease. The last review also addressed previous concerns regarding the applicability of this evidence to routine clinical practice. Trials with 6 or more months of follow-up were included if they assessed the effects of exercise training alone or in combination with psychologic or educational interventions. Altogether, 48 trials with a total of 8940 patients were included. Cardiac rehabilitation compared with usual care was associated with reduced all-cause mortality (odds ratio (OR) 0.80; 95% confidence interval (CI) 0.68 – 0.93) and cardiac mortality (OR 0.74; 95% CI 0.61 – 0.96) (Class I, Level A). There was no difference in recurrent myocardial infarction, CABG or PTCA (Class IIb, Level B) (Table 24.1).
Table 24.1 Pooled odds ratios (OR) and 95% confidence intervals (CI) for total and cardiac mortality, recurrent myocardial infarction, CABG and PTCA in patients with CHD randomly assigned to evidence-based cardiac rehabilitation versus usual care20
At follow-up the proportion of patients who reported smoking was significantly reduced with cardiac rehabilitation (OR 0.64; 95% CI 0.50 –0.83) (Class IIa, Level B). There was a significantly greater reduction in systolic blood pressure for those in cardiac rehabilitation (weighted mean difference,-3.2mmHg; 95% CI-5.4 to-0.9mmHg) but no difference in diastolic blood pressure (Class IIa, Level B). There was also a significantly greater reduction in total cholesterol concentration (weighted mean difference,-0.37 mmol/L (-14.3 mg/dL); 95% CI-0.63 to-0.11 mmol/L (- 24.3 to-4.2mg/dL)) and triglyceride concentration (weighted mean difference,-0.23mmol/L (-20.4mg/dL); 95% CI-0.39 to-0.07mmol/L (- 34.5 to-6.2mg/dL)) for those in cardiac rehabilitation, but no difference in low-density or high-density lipoprotein concentrations (Class IIa, Level B). With the exception of smoking, the other risk factor changes in favor of intervention were rather small, and therefore would have had a limited impact on clinical events. So the reduction in total and cardiac mortality observed in this meta-analysis can be largely attributed to lifestyle changes: increased physical activity, healthier diets and smoking cessation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


