Although stenting has been used as a treatment option for aortic coarctation (CoA) at increasingly younger ages, limited information is available on the long-term follow-up of stent implantation for CoA in pediatric patients. A total of 74 patients with CoA (mean age 8 ± 3 years) underwent stent implantation; 42 were treated for isolated native CoA and 32 for recurrent CoA. A total of 87 stents were implanted (bare metal stents in 71 patients and covered stents in 3 patients). Redilation of a previously implanted stent was performed in 32 patients. Immediately after stenting, the peak systolic pressure gradient decreased from 68 ± 16 mm Hg to 8 ± 5 mm Hg (p <0.05), and the CoA diameter increased from 5 ± 3 mm to 16 ± 3 mm (p <0.05). The most important procedural complication was aneurysm formation in 1 patient that was successfully treated with implantation of a covered stent. No early or late deaths occurred and no evidence was found of late aneurysm formation during a follow-up period of 6 years. Late stent fracture was observed in 3 patients. At the end of follow-up, no cases of recoarctation were identified on multislice computed tomography or magnetic resonance imaging, and 67 (85%) of the 74 patients were normotensive, receiving no medications. In conclusion, stent implantation is an effective and safe treatment alternative to conventional surgical management for the treatment of CoA in selected pediatric patients.
Transcatheter stent implantation for coarctation of the aorta (CoA) has evolved as a very important treatment modality in this clinical entity with excellent short-term results reported in children and adults. Limited information is available, however, on the long-term follow-up of stenting for CoA in children. The present study reports the initial and 6-year results for 74 pediatric patients who underwent stent implantation for CoA.
Methods
The medical records of 74 consecutive patients from 2 cardiac centers in Greece, who underwent stent implantation for CoA from May 2001 to August 2005 and who had completed 6 years of follow-up, were analyzed retrospectively. Patients with hypoplasia of the transverse and/or distal aortic arch and those with complex CoA (complete atresia) were excluded from the study. Hypoplasia was defined as a ratio of the diameter of the aortic arch and isthmus to the diameter of the descending aorta at diaphragm of <0.6. Native CoA or recoarctation was diagnosed when an arm-to-leg systolic pressure gradient (measured by cuff sphygmomanometry) of ≥20 mm Hg was present (with or without systemic hypertension), and CoA was confirmed by magnetic resonance imaging (MRI) or multislice computed tomography (MSCT). Arterial hypertension was defined as systolic blood pressure greater than the 95th percentile for blood pressure for age, height, and gender. The stents were implanted in the context of a protocol approved by the ethical committees of the participating hospitals, with treatment options determined by institutional/interventionalist preference. Informed parental consent was obtained for each patient.
All patients underwent cardiac catheterization and biplane aortography under general anesthesia. The procedure of stenting for CoA has been previously described in detail. In brief, stents (Palmaz 4014, Palmaz 308, and Genesis XD, Johnson & Johnson International Systems, Warren, New Jersey, or Cheatham Platinum, Numed, Hopkinton, New York) dilatable to a large aortic diameter were implanted using 8F to 12F sheaths. In 15 patients with a body weight <20 kg, the Genesis XD stents were crimped on low-profile, 8- to 10-mm balloons (percutaneous transluminal angioplasty balloons, Cordis, Johnson & Johnson) introduced through 6F to 7F sheaths to reduce the risk of damaging the femoral artery. The stents were further dilated to a larger diameter using 10- to 12-mm balloons that were introduced through a 7F sheath. In 18 patients (8 with severe CoA, 7 with tortuous and long-segment CoA, and 3 with bicuspid aortic valve and aneurysmal dilation of the ascending aorta), the procedure was staged and guided using the antegrade monitoring technique.
The diameter of the balloon was equal to, or 1 mm greater than, the diameter of the proximal aortic isthmus but not greater than the diameter of the aorta at the level of diaphragm as measured using biplane aortography. The initial balloon/CoA diameter ratio was ≤4:1 to avoid aortic complications. A ratio of >3.5:1 was used in patients with moderate CoA. A larger balloon was used when a diameter of ≥1 mm of the proximal aortic isthmus was not achieved at the initial dilation. After the procedure, repeat aortography and pressure measurements distal and proximal to the stented segment were obtained. A satisfactory early result was defined as a postprocedural pressure gradient of <20 mm Hg.
The patients were discharged 1 to 2 days after the procedure and were administered aspirin 3 to 5 mg/kg/day for 6 months. They were re-evaluated clinically at 1 and 3 months after the procedure and then serially every 6 months. Follow-up included arm-to-leg pressure measurements, echocardiographic Doppler studies, and biplane chest radiography.
All patients were followed up for 6 years after the procedure. Overall, 68 patients underwent a treadmill exercise test according to the Bruce protocol at the end of the 6-year follow-up period. Patients who had undergone stent implantation before 2005 (when no MSCT facility was available at our institutions) underwent MRI, including brain 3-dimensional magnetic resonance angiography at 1, 3, and 5 years after stent placement. The patients who were studied after 2005 underwent a preprocedural brain MRI and MSCT evaluation at 1 month and 3 and 6 years after stent implantation. A satisfactory late result was defined as the absence of restenosis (aortic diameter across the stents equal to the diameter of the proximal isthmus) using MRI or MSCT, as well as an arm-to-leg pressure gradient <20 mm Hg, as measured by cuff spygmomanometry.
The results are expressed as the mean ± SD or median (range), as appropriate. Pre- and post-stent implantation comparisons were made using the paired Wilcoxon test. A p value <0.05 was considered significant.
Results
A total of 74 patients (54% males) underwent stent implantation for CoA. The mean age was 8 ± 3 years, and the median body weight was 28 kg (range 16 to 54). Forty-two patients had isolated native CoA and 32 recurrent CoA (20 patients had undergone a single surgical repair, 6 surgical repair and balloon dilation, and 6 balloon dilation). Of the 74 patients, 62 had discrete CoA and 12 had tubular stenosis; 30 patients had a bicuspid aortic valve. Overall, 62 patients (84%) were hypertensive, all receiving antihypertensive medications. Preprocedural brain 3-dimensional magnetic resonance angiography did not reveal the presence of aneurysms of the circle of Willis in this patient population.
A total of 87 stents were implanted. Palmaz 4014 and Palmaz 308 stents were placed in 17 and 15 patients, respectively. Genesis XD stents were implanted in 28 patients, and Cheatham platinum bare metal stents in 11 patients. Covered stents were used in 3 patients (2 with an associated aneurysm and 1 with a traumatic aneurysm). Six patients with tubular long segment stenosis had 2 stents simultaneously placed. The mean initial balloon/CoA diameter ratio was 3.2 ± 0.8. After stent implantation, the peak systolic pressure gradient decreased from 68 ± 16 mm Hg to 8 ± 5 mm Hg (p <0.05). The CoA diameter at the stented area increased from 5 ± 3 mm to 16 ± 3 mm (p <0.05).
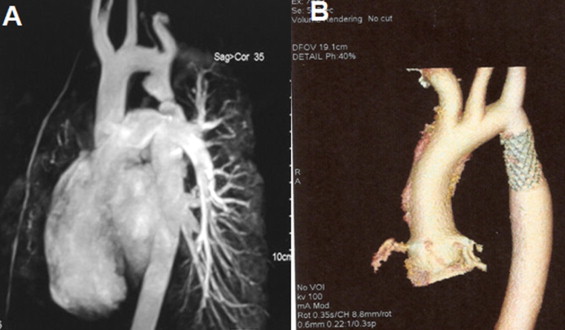
Two procedural complications occurred during the present study. One patient developed a traumatic aneurysm that was treated with covered stent implantation. The other patient developed a femoral pseudoaneurysm requiring surgical repair. Hematoma at the site of access occurred in 6 patients. Transient loss of the arterial pulse occurred in 7 patients. No late aortic aneurysms or recoarctation were identified by MSCT ( Figure 1 ) during the 6-year follow-up period. The mean MSCT-measured diameter of the CoA site was 17 ± 2 mm. The sphygmomanometric peak systolic blood pressure difference between the arms and legs was 4 ± 3 mm Hg. No patient had absent or low-volume distal pulses during follow-up, and no collaterals were present on MSCT. No evidence was found of aneurysms of the circle of Willis on contrast-enhanced magnetic resonance angiography of the brain. Redilation of a previously implanted stent was performed in 32 patients. Of these, 18 patients were initially assigned for staged dilation and underwent elective redilation of the stents to a larger aortic diameter equal to the diameter of the proximal aortic isthmus (≤19 mm) using high-pressure balloons 1 to 2 years after the initial procedure ( Figure 2 ) . Fourteen patients <8 years of age with growth-related restenosis (size–mismatch between the stented segment and the proximal and distal aortic segments) and an arm/leg pressure gradient >20 mm Hg underwent stent redilation 5 to 6 years later. The peak systolic pressure gradient decreased from 23 ± 4 mm Hg to 6 ± 3 mm Hg. No aortic complications were observed because of the redilation procedures. Mild neointimal hyperplasia within the stent was observed on chest radiographs in 16 of the 32 stents at redilation.
At the end of the follow-up period, 63 (85%) of 74 patients were normotensive (normal blood pressure at rest and normal exercise blood pressure responses within an expected range for normal patients) and receiving no medications. Three patients had late fractures of 2 Genesis XD and 1 Cheatham Platinum stents, as diagnosed by chest radiography or MSCT. Two of these patients with significant restenosis and multiple stent fractures were successfully treated with the placement of 2 additional stents ( Figure 3 ) .




