A multisite observational study of sexual activity-related outcomes in patients enrolled in the TRIUMPH registry during hospitalization for an acute myocardial infarction (AMI) was conducted to identify patterns and loss of sexual activity 1 year after hospitalization for AMI. Gender-specific multivariable hierarchical models were used to identify correlates of loss of sexual activity including physician counseling. Main outcome measurements included “loss of sexual activity” (less frequent or no sexual activity 1 year after an AMI in those who were sexually active in the year before the AMI) and 1-year mortality. Mean ages were 61.1 years for women (n = 605) and 58.6 years for men (n = 1,274). Many were sexually active in the year before and 1 year after hospitalization (44% and 40% of women, 74% and 68% of men, respectively). One third of women and 47% of men reported receiving hospital discharge instructions about resuming sex. Those who did not receive instructions were more likely to report loss of sexual activity (women, adjusted relative risk 1.44, 95% confidence interval 1.16 to 1.79; men, adjusted relative risk 1.27, 95% confidence interval 1.11 to 1.46). One year mortality after AMI was similar in those who reported sexual activity in the first month after AMI (2.1%) and those who were sexually inactive (4.1%, p = 0.08). In conclusion, although many patients were sexually active before AMI, only a minority received discharge counseling about resuming sexual activity. Lack of counseling was associated with loss of sexual activity 1 year later. Mortality was not significantly increased in patients who were sexually active soon after their AMI.
The Translational Research Investigating Underlying Disparities in Acute Myocardial Infarction Patients’ Health Status (TRIUMPH) study is a national, multisite, prospective longitudinal study that followed patients for 12 months after hospitalization for an AMI. We developed a substudy of the TRIUMPH study to specifically investigate sexual activity before and after AMI, the frequency of receipt of counseling after AMI and its association with sexual activity, and the association of 1-year mortality with sexual activity after AMI.
Methods
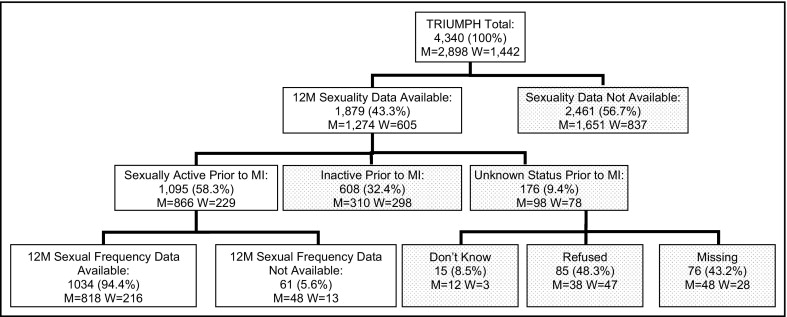
The TRIUMPH study design has been previously described and enrolled 4,340 adult patients (≥18 years old) from April 2005 through December 2008 from 24 hospitals across the United States. This substudy (n = 1,879; 1,274 men and 605 women) was initiated in September 2007 when a sexuality module was added ( Figure 1 ). Inclusion of the sexuality module was prompted by the August 2007 publication of the first comprehensive United States population data on, and methods for eliciting, sexual activity and function in middle-age and older adults from the 2005 through 2006 National Social Life, Health, and Aging Project (NSHAP). The study was conducted with written informed consent and approval of all participating sites’ and investigators’ institutional review boards.
Baseline data were collected through bedside interviews with trained staff within 24 to 72 hours of the index AMI and supplemented with medical record abstractions for the index hospitalization. These include data on patients’ sociodemographic characteristics, depressive symptoms, physical function, and disease severity. Depression was assessed using the 9-item Patient Health Questionnaire (PHQ-9) ; patients were classified as having moderate depression if their score was ≥10. Physical functioning was assessed using the 12-item Short-Form Health Survey Physical Composite Score (SF-12 PCS), with a higher score representing better physical functioning over the previous 4 weeks. Elements of the Global Registry of Acute Coronary Events (GRACE) Risk Score (age, heart rate, systolic blood pressure, initial creatinine, congestive heart failure, ST-segment deviation, previous MI, percutaneous coronary intervention, and cardiac enzymes) were prospectively collected at baseline and used to predict 6-month mortality in survivors of acute coronary syndrome; a higher GRACE risk score is associated with increased risk. Follow-up data were obtained by telephone interviews at 1 month and 6 and 12 months. The sexuality module included a 5-item sexual activity and communication assessment administered by telephone interviewers at 1 month and 12 months after enrollment.
Sex or sexual activity was defined for study participants, as in the NSHAP study, as “any mutually voluntary activity with another person that involves sexual contact, whether or not intercourse or orgasm occurs.” “Pre-AMI sexual activity” was measured using the yes/no question: “Did you have sex or sexual activity at any time in the 12 months before having a heart attack?” “Post-AMI sexual activity” was measured at 1 month and 12 months using the yes/no question: “Have you had sex or sexual activity since having a heart attack?” Patients who reported sexual activity before AMI were asked: “Compared to how things were in the 12 months before having a heart attack, have you had sex more frequently since your heart attack, with about the same frequency … or less frequently …” (“don’t know” and “refused” were also coded). To model sexual outcomes at 12 months in those reporting sexual activity before AMI, patients were coded for multivariable regression analysis as (1) having “loss of sexual activity” if they reported no or less frequent sexual activity at 12 months after the AMI or (2) the “reference group” if they maintained or reported an increased frequency of sexual activity.
Whether patients received discharge instructions about “when to resume sexual activity” after the index AMI was assessed by patient interview. Discussion with a physician about sex during the period after hospitalization was assessed using the dichotomous “Have you ever discussed sex with your doctor since your heart attack?,” adapting a similar question from the NSHAP, the 2005 through 2006 national benchmark study of sexuality in older United States adults. Item refusal rates for the sexual activity items ranged from 3.6% to 5.2%.
Inclusion criteria for analysis required receipt of the sexuality module (all patients who had not yet completed 12-month follow-up or who enrolled in TRIUMPH after the substudy was initiated in September 2007) and completion of the 12-month follow-up interview (n = 1,879, 1,274 men and 605 women). Unadjusted analyses evaluated gender differences in sociodemographic characteristics, health, sexual activity before and after AMI, and communication with a physician about sex using t tests for continuous variables and chi-square tests for categorical variables.
In the subset of patients who reported sexual activity before AMI (n = 1,095, 866 men and 229 women), gender-specific and combined multivariable regression analysis was used to assess risk factors for loss of sexual activity 12 months after AMI. The main variables of interest were those that could be modified by the physician including discharge instructions and physician discussions about sex. Models were adjusted for age, marital status, PHQ-9 (dichotomized as ≥10 vs <10), SF-12 PCS, and GRACE score. Individual co-morbidities were not included in the model because of the limited sample size. Because the outcome was not rare, we used a modified Poisson regression model with robust SEs to directly estimate relative risk. A random effect for site and site-centered covariates were used to adjust for confounding by site.
Modeling of 12-month sexual activity outcomes used patients’ 12-month recall of receiving discharge instructions and of discussion with a physician about sex. The 12-month recall of receiving discharge instructions was used in lieu of the 1-month variable to maximize the sample size for this analysis. Three hundred fifty-two patients completed their 1-month interview before introduction of the sexuality module into the TRIUMPH study. To assess for possible recall bias on the discharge instruction variable, patients’ 1- and 12-month recall about receipt of discharge instructions were compared to discharge instructions documented in the baseline chart (when available). This analysis was also stratified by gender and sexual activity status.
Survival time for all patients who completed the sexuality module at 1 month (n = 1,130) was derived as the interval from a patient’s 1-month interview date to death from any cause. Mortality data from any cause were assessed through the Social Security Administration Death Master File. Vital status data were available for >99% of the cohort based on a matching algorithm for social security number, date of birth, and name. Patients still alive 1 year later were censored. Kaplan–Meier survival estimates were calculated in patients who had completed the 1-month sexuality module and were stratified by whether they had been sexually active since their AMI. Log-rank tests were used for comparisons between these groups. Multivariable adjustment for potential confounders was limited because of the small number of events (n = 40); therefore, the multivariable Cox proportional hazards models were simply adjusted for baseline physical function (SF-12 PCS). As a validity check, the same analyses were repeated adjusting for the GRACE score, which includes baseline age.
The p values are 2-sided and were evaluated at a significance level of 0.05. All analyses were conducted using SAS 9.2 (SAS Institute, Cary, North Carolina) and R 2.10.1.
Results
The TRIUMPH study enrolled 4,340 patients, 1,879 of whom received the sexuality module ( Figure 1 ). Baseline characteristics by gender are listed in Table 1 . Women were older and less likely to be married than men and had higher rates of depression, lower physical functioning scores, and higher 6-month mortality risk scores than men. Many patients were sexually active at baseline and at 12 months. In married women, sexual activity rates were significantly higher at baseline (65%) and at 12 months (62%).
| Overall | Men | Women | p Value | |
|---|---|---|---|---|
| (n = 1,879) | (n = 1,274) | (n = 605) | ||
| Characteristics measured at baseline | ||||
| Age (years), mean ± SD | 59.4 ± 11.7 | 58.6 ± 11.0 | 61.1 ± 12.8 | <0.001 |
| Race | <0.001 | |||
| White/Caucasian | 1,330 (71.0%) | 964 (75.9%) | 366 (60.7%) | |
| Black/African-American | 405 (21.6%) | 209 (16.5%) | 196 (32.5%) | |
| Other | 138 (7.4%) | 97 (7.6%) | 41 (6.8%) | |
| Married | 1,066 (56.9%) | 819 (64.4%) | 247 (41.0%) | <0.001 |
| Depression † | 306 (17.4%) | 177 (14.7%) | 129 (23.2%) | <0.001 |
| 12-Item Short-Form Health Survey Physical Composite Score, ‡ mean ± SD | 43.3 ± 12.2 | 44.8 ± 11.9 | 40.1 ± 12.1 | <0.001 |
| Global Registry of Acute Coronary Events score, § mean ± SD | 99.1 ± 27.7 | 97.5 ± 27.4 | 102.5 ± 28.1 | <0.001 |
| Characteristics measured at 12 months | ||||
| Sex before acute myocardial infarction | 1,095 (64.3%) | 866 (73.6%) | 229 (43.5%) | <0.001 |
| Sex since acute myocardial infarction | 1,013 (59.6%) | 803 (68.3%) | 210 (40.0%) | <0.001 |
| Received instructions | 787 (42.9%) | 585 (46.8%) | 202 (34.6%) | <0.001 |
| Discussed sex with physician ‖ | 439 (33.6%) | 378 (39.1%) | 61 (17.9%) | <0.001 |
⁎ All percentages were calculated excluding missing data, “don’t know,” and “refused” response options from the denominator.
† Depression defined as a 9-item Patient Health Questionnaire score ≥10.
‡ Range 0 to 100; a higher score represents better physical functioning.
§ Range 1 to 263; a higher score represents a higher mortality risk at 6 months after myocardial infarction.
‖ Missing information for this variable (30.4%) was due to a skip pattern error in interviews of patients who reported no sexual activity before or since their myocardial infarction; missing information did not vary by gender, age, marital status, or health status. Missing information on this item in those who were sexually active before their myocardial infarction (subset included in multivariable models) was 3%.
Patients who were sexually active in the year before their AMI were significantly more likely than those who were inactive to report receiving discharge instructions about resuming sex (men 54% vs 32%, p <0.001; women 58% vs 23%, p <0.001). Married patients were significantly more likely than unmarried patients to receive discharge instructions about resuming sexual activity (men 51% vs 40%, p <0.001; women 44% vs 28%, p <0.001). In the 12 months of follow-up, 38% of sexually active patients (41% of sexually active men and 24% of sexually active women, p <0.001) discussed sex with their physician. Unmarried sexually active patients were significantly less likely to have discussed sex with a physician after their AMI (33% unmarried vs 40% married, p = 0.03). This marital status difference was similar in men and women. Patients’ 1- and 12-month recall about receipt of discharge instructions were compared to discharge instructions documented in the baseline chart (when available). There was no difference in recall by gender or sexual activity status.
Of patients reporting sexual activity before AMI, 48% of men and 59% of women reported less frequent sexual activity in the 12 months after the AMI ( Table 2 ), and 11% of men and 13% of women reported no sexual activity in the subsequent year. Some patients who were sexually inactive in the year before their AMI initiated sexual activity in the year after (9.1% of men, 4.0% of women). In multivariable analysis, significant predictors of loss of sexual activity for men included not receiving discharge instructions about resumption of sex, having a discussion with a doctor about sex since the AMI, and a lower baseline SF-12 Physical Function Score. The only significant predictor of loss of sexual activity for women was not having received discharge instructions about sex. Age, marital status, depression, and GRACE score were not significant predictors of loss of sexual activity in men or women ( Figure 2 ). Multivariable analysis was repeated combining men and women in a single model and no significant interaction between gender and receiving discharge instructions in predicting loss of sexual activity was found.
| Sexual Frequency Since AMI | Men | Women | ||||
|---|---|---|---|---|---|---|
| More/Same | Less/None | p Value | More/Same | Less/None | p Value | |
| (n = 427) | (n = 391) | (n = 88) | (n = 128) | |||
| Characteristics measured at baseline | ||||||
| Age (years), mean ± SD | 55.3 ± 9.9 | 57.0 ± 10.1 | 0.013 | 53.8 ± 11.1 | 53.7 ± 11.1 | 0.954 |
| Race | 0.001 | <0.001 | ||||
| White/Caucasian | 349 (82.1%) | 278 (71.5%) | 68 (77.3%) | 69 (54.3%) | ||
| Black/African-American | 51 (12.0%) | 79 (20.3%) | 19 (21.6%) | 46 (36.2%) | ||
| Other | 25 (5.9%) | 32 (8.2%) | 1 (1.1%) | 12 (9.4%) | ||
| Married | 309 (72.4%) | 271 (69.5%) | 0.365 | 65 (74.7%) | 72 (56.7%) | 0.007 |
| Depression † | 40 (9.9%) | 54 (14.8%) | 0.036 | 17 (19.8%) | 24 (20.2%) | 0.944 |
| 12-Item Short-Form Health Survey Physical Composite Score, ‡ mean ± SD | 48.5 ± 10.1 | 44.0 ± 12.5 | <0.001 | 44.1 ± 11.8 | 40.1 ± 11.8 | 0.019 |
| Global Registry of Acute Coronary Events score, § mean ± SD | 87.8 ± 23.6 | 95.0 ± 25.8 | <0.001 | 86.5 ± 22.8 | 88.5 ± 23.6 | 0.549 |
| Characteristics measured at 12 months | ||||||
| Sex since acute myocardial infarction | 426 (100%) | 330 (85.5%) | <0.001 | 85 (97.7%) | 109 (85.2%) | 0.002 |
| Received instructions | 259 (61.2%) | 185 (47.7%) | <0.001 | 60 (69.0%) | 65 (52.4%) | 0.016 |
| Discussed sex with physician | 162 (38.5%) | 168 (44.1%) | 0.107 | 25 (28.7%) | 26 (20.3%) | 0.154 |
⁎ All percentages were calculated excluding missing data, “don’t know,” and “refused” response options from the denominator.
† Depression defined as a 9-item Patient Health Questionnaire score ≥10.
‡ Range 0 to 100; a higher score represents better physical functioning.
§ Range 1 to 263; a higher score represents a higher mortality risk at 6 months after myocardial infarction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


