Incompetent Venous Perforators
RANDOLPH TODD C. JONES and LOWELL S. KABNICK
Presentation
A 68-year-old man presents to the office with recurrent edema, pain, and ulceration of the right lower extremity. The patient is well known and has a long history of venous disease: Deep Venous Thrombosis (DVT), superficial venous insufficiency, and venous ulcers. He has had several endovenous thermal ablations involving his superficial axial veins, including the right small and great saphenous veins. In addition, he underwent intravascular ultrasound (IVUS) with percutaneous transluminal angioplasty (PTA) and stenting of the right common and external iliac veins for significant stenosis (77% area reduction) and Intraluminal scarring. Until his presentation today, his ulcer had been healed.
On physical exam, he is afebrile and his vital signs are within normal limits.
The patient has bilateral lower extremity pitting edema, which is significantly worse on the right. Most notably, there is an area of ulceration just superior to the medial malleolus measuring 3.5 cm × 6 cm in diameter (Fig. 1). The ulcer bed is moist, clean, and with no overt signs of infection. There is mild epidermal erythema, hyperpigmentation, and induration. His dorsalis pedis and posterior tibial pulses are 2+, equal, and bilateral.

FIGURE 1 Typical appearing venous stasis ulcer of the lower extremity. Note the hyperpigmentation surrounding the ulcer, and its location on the medial malleolus.
Differential Diagnosis
Lower extremity ulcer etiologies are numerous. Patients presenting with lower extremity ulceration require workup for both venous and arterial insufficiencies. Before proceeding with any ulcer therapy, malignancy and arterial ulcer etiologies must be excluded. Biopsy may be necessary to identify the root cause.
In the above patient, consideration for recurrent DVT, in-stent restenosis, and/or stent occlusion should be ascertained before proceeding with further evaluation and treatment.
Workup
The evaluation of all patients with lower extremity ulceration includes identifying the causal factor(s) of the ulceration and excluding other more morbid and potentially life-threatening etiologies. After arterial, traumatic, or infectious etiologies are excluded, the exact nature and extent of peripheral venous insufficiency is determined.
Understanding venous anatomy of the lower extremities is paramount to accurate diagnosis and optimal treatment of superficial venous reflux. This is further emphasized by the fact that the perforating veins are numerous, occur at relatively regular anatomic locales in the lower extremities (Fig. 2), and can often be missed, even by the most experienced ultrasonographers. Of note, the short and long saphenous veins have since been renamed the “small saphenous” and “great saphenous” veins, respectively. In addition, the named perforating veins have fallen out of favor for more descriptive anatomic nomenclatures such as the medial thigh, popliteal, and posterior tibial perforators. The importance of knowing the locations of the various perforators and understanding that incompetent perforating veins (IPVs) can be a major source of recurrent varicose veins and venous ulcers cannot be overemphasized.
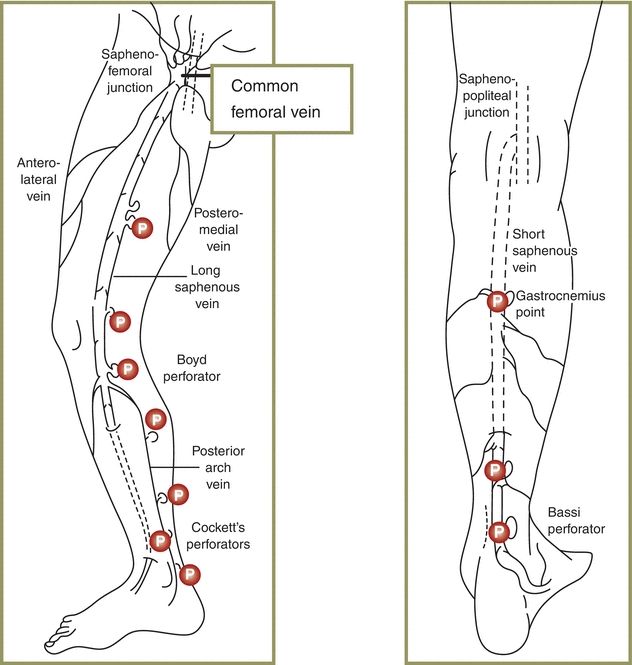
FIGURE 2 This diagram of the various perforating and axial veins of the thigh and leg uses older nomenclature.
Duplex ultrasound has a high degree of diagnostic accuracy, low cost, and widespread availability. Presently, ultrasound is considered by most as the gold standard for diagnosis of peripheral venous insufficiency and DVT. Using duplex ultrasound for perforator investigation, we can document the location, diameter, degree of reflux, and its connection to any superficial tributaries that might be contributing to varicosities, advanced skin changes, or ulceration (Figs. 3 and 4).
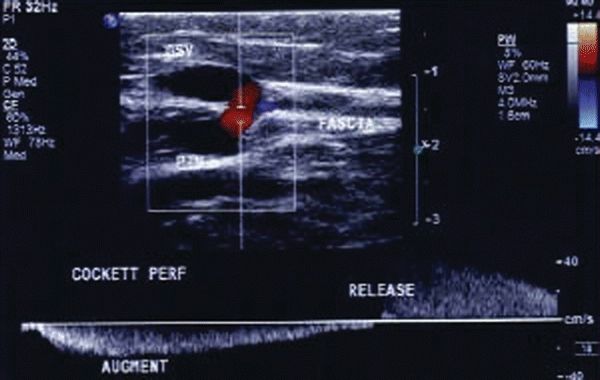
FIGURE 3 Color flow Doppler image of a refluxing perforating vein.
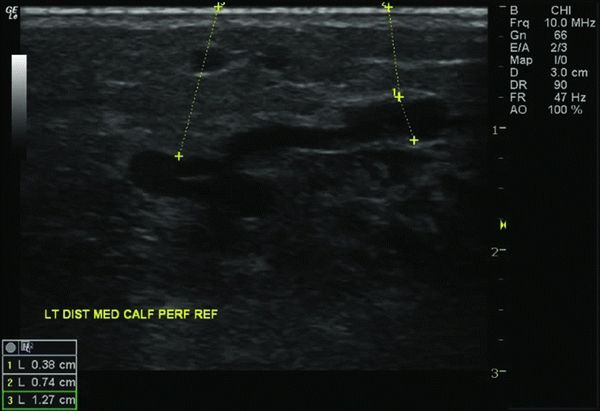
FIGURE 4 An incompetent perforating vein with a diameter of 3.8 mm.
Typically, when using duplex imaging for perforator size determination, the diameter is measured horizontally at the level where the perforator exits the fascia (Fig. 4). Some venous interventionalists prefer to measure the size where the perforator is largest, which is usually just superficial to where it exits the muscular fascia. Refluxing perforators need to be a minimum of 3.5 mm in diameter with duration of reflux lasting greater than 0.5 seconds to be considered of hemodynamic significance.
CEAP and Venous Clinical Severity Scores (VCSS) should be documented on all patients with symptomatic superficial or deep venous insufficiency. Additionally, the clinical score of the CEAP classification is of particular importance, as it is a key component of the American Venous Forum (AVF) and Society for Vascular Surgery (SVS) guidelines for perforator treatment.
The duration of a nonhealing ulcer is very important in determining treatment options. In some cases, lower extremity ulcers may have been present for several months and even years. The patient may have had no prior treatment for the ulcer(s), or the ulcer may have been refractory to medical and/or surgical therapies. In either case, it is necessary to rule out both infection and malignancy. In the presence of significant pain and surrounding erythema, one must consider the possibility of infection, which may be present even in the absence of a purulent exudate or a surrounding cellulitis. In this scenario, cultures should be taken. A painless ulcer that has been refractory to conservative medical or surgical therapy may be of malignant etiology. Biopsy of any suspicious lower extremity ulcer should be considered.
Diagnosis and Treatment
A thorough history and physical examination are an essential part of any patient encounter. In particular, emphasis should be placed on obtaining a pertinent history of the patient’s symptomatology, prior procedures (or prior treatment of venous insufficiency), superficial venous thrombophlebitis, or deep venous thrombophlebitis. The exact dimensions of the ulcer(s), as well as their anatomic location (measured as the number of centimeters from the heel of the foot), should be documented. These measurements will be of importance in tracking the patient’s progress and determining the need for procedural intervention(s).
Duplex ultrasound is of vital importance in the diagnosis and treatment of incompetent venous perforators. The contribution of IPVs to ambulatory venous hypertension is significant. Up to 70% of IPVs are of hemodynamic significance, and nearly half (45%) of IPVs are not abolished with saphenous ablation. Surgical therapy for superficial venous reflux has not been shown to improve the rate of ulcer healing, but it has been shown to decrease the incidence of recurrence.
Perforator Treatment Guidelines
The current indications for incompetent perforator interruption according to the AVF and SVS are as follows: (1) The patient must have C5 or C6 disease (either an active venous ulcer or a healed ulcer); (2) the perforator must have demonstrable reflux of 0.5 seconds or greater; (3) the perforator must be greater than 3.5 mm in diameter, measured where it exits the muscular fascia; and (4) the perforator must be anatomically related to the area of the ulcer or healed ulcer.
Surgical Approach
There are several efficient ways of interrupting IPVs. Each technique has its individual advantages and disadvantages. Proper technique selection is essential to clinical success.
Open perforator ligation using ultrasound guidance to hook the perforator or a communicating tributary is a technique that can be quite useful in some patients with C3 or C4a disease. This procedure can be done in combination with ambulatory phlebectomy of any associated varicosities; however, it may be of limited utility in a patient with more advanced disease such as lipodermatosclerosis (C4b) or an active or healed ulcer. Healing of wounds around a previous or active ulcer bed is unpredictable at best, and making an incision (however small) into this area is not recommended.
Endovenous techniques include ultrasound-guided chemical, laser, and radiofrequency ablation. Common steps to all three techniques include the use of duplex ultrasound to gain needle access to the perforator (Fig. 5) or a communicating tributary in close proximity, after which the chosen ablative device is introduced into the vein via a catheter or directly through the needle access.
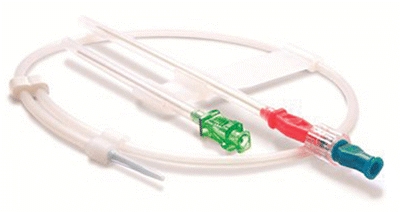
FIGURE 5 An 0.018″ microintroducer set, which includes a 21-g needle, 0.018″ guidewire, and a 4-French introducer sheath.



