The structural and functional characteristics of left atrial appendage (LAA) in patients with atrial fibrillation (AF) with previous stroke remain incompletely elucidated. This study investigated whether a larger LAA orifice is related to decreased LAA flow velocity and stroke in nonvalvular AF. The dimension, morphology, and flow velocity of LAA were compared in patients with nonvalvular AF with (stroke group, n = 67, mean age 66 ± 9 years) and without ischemic stroke (no-stroke group, n = 151, mean age 56 ± 10 years). Compared with no-stroke group, the stroke group had larger LA dimension (4.7 ± 0.8 vs 4.2 ± 0.6 cm, p <0.001), larger LAA orifice area (4.5 ± 1.5 vs 3.0 ± 1.1 cm 2 , p <0.001), and slower LAA flow velocity (36 ± 19 vs 55 ± 20 cm/s, p <0.001). LAA flow velocity was negatively correlated with LAA orifice size (R = −0.48, p <0.001). After adjustment for multiple potential confounding factors including CHA 2 DS 2 -VASc score, persistent AF, and LA dimension, large LAA orifice area (odds ratio 6.16, 95% confidence interval 2.67 to 14.18, p <0.001) and slow LAA velocity (odds ratio 3.59, 95% confidence interval 1.42 to 9.08, p = 0.007) were found to be significant risk factors of stroke. In patients with LAA flow velocity <37.0 cm/s, patients with large LAA orifice (>3.5 cm 2 ) had greater incidence of stroke than those with LAA orifice of ≤3.5 cm 2 (75% vs 23%, p <0.001). In conclusion, LAA orifice enlargement was related to stroke risk in patients with nonvalvular AF even after adjustment for other risk factors, and it could be the cause of decreased flow velocity in LAA.
In this study, we hypothesized that increased orifice size of the left atrial appendage (LAA) is related to decreased flow velocity in the LAA and stroke in patients with atrial fibrillation (AF). To test this hypothesis, we analyzed the geometry, dimensions, and flow velocity of LAA using multidetector computed tomography (MDCT) and transesophageal echocardiography (TEE) in a series of patients with nonvalvular AF with and without ischemic stroke. We also evaluated whether large LAA orifices were related to decreased flow velocity of LAA and stroke in patients with nonvalvular AF.
Methods
The study protocol was approved by the Institutional Review Board of Severance Hospital, Seoul, Korea, and complied with the tenets of the Declaration of Helsinki. Written informed consent was obtained from all patients. From February 2008 to February 2011, 67 consecutive, patients with nonvalvular AF with ischemic stroke were enroled in this study (stroke group). Ischemic stroke was confirmed by brain CT and magnetic resonance imaging. All patients underwent 64-channel MDCT (Sensation 64; Siemens Medical Solutions, Forchheim, Germany) and TEE. The no-stroke group included 151 patients with nonvalvular AF without previous history of stroke and who underwent MDCT and TEE preparing for ablation of AF. This study included only patients with nonvalvular AF who were not taking anticoagulants at the time of their stroke, or at the time of cardiac MDCT for patients without a history of stroke, to prevent possible confounding effects. Patients <18 years of age were excluded. LAA velocity may be different between AF and sinus rhythm. Therefore, we included patients who showed the same rhythm during MDCT and TEE examination. Furthermore, we excluded patients who had undergone cardioversion therapy within 3 weeks before the TEE or CT, because LAA velocity may be affected by recent cardioversion.
The CHADS 2 (congestive heart failure, hypertension, age >75, diabetes mellitus, and previous stroke or transient ischemic attack) and CHA 2 DS 2 -VASc (congestive heart failure, hypertension, age >75, diabetes mellitus, and previous stroke or transient ischemic attack, vascular disease, age >65, women) scores of each patient were calculated. For the stroke group, we excluded the points for current stroke in the CHADS 2 and CHA 2 DS 2 -VASc scoring system. Congestive heart failure was defined as clinical heart failure (stage C or D) according to the 2009 Focused Update Incorporated Into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults. Hypertension was defined as systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg at 2 or more visits or medical history of hypertension. Dyslipidemia was defined by fasting triglyceride plasma levels ≥150 mg/dl and/or fasting total cholesterol ≥200 mg/dl and/or low-density lipoprotein-C ≥130 mg/dl and/or high-density lipoprotein-C <40 mg/dl or current use of lipid-lowering medications such as hydroxymethylglutaryl-CoA reductase inhibitors, bile acid sequestrants, and fibric acid derivatives. AF was classified as paroxysmal AF that self-terminates within 7 days and persistent AF that either lasts longer than 7 days or requires termination by cardioversion, either with drugs or by direct current cardioversion.
TEE was performed with a 5-MHz multiplane transesophageal transducer connected to an ultrasound system (iE33; Philips Medical Systems, Andover, Massachusetts). After local pharyngeal anesthesia with lidocaine spray, the patient was placed in the left lateral position, and the transesophageal transducer was inserted into the esophagus. The LAA was observed in 0°, 45°, 90°, and 135° to detect spontaneous echocontrast or thrombus. Then, a sample volume was placed at the middle portion of the LAA, and peak velocities of flow out of the LAA (emptying velocity) were measured. LAA peak emptying velocities were determined during 10 cardiac cycles, and the average value was used for analyses.
Contrast-enhanced cardiac CT scans were performed using a 64-slice MDCT (Somatom Sensation 64; Siemens Medical Solutions, Forchheim, Germany). A bolus of 60 to 80 ml iopamidol (Iopamiro 370; Bracco, Italy) was injected into an antecubital vein at a flow rate of 5 ml/s and then followed by a 50 ml saline chasing bolus at 5 ml/s. The start delay was defined by bolus tracking in the ascending aorta, and the scan was automatically initiated 5 seconds after reaching the contrast threshold of 140 H. Scans were performed using the following parameters: retrospective electrocardiographic-gated acquisitions, 80 to 120 kVp, 500 to 700 mAs depending on patient size, and 64 × 0.6 mm slice collimation. Scans were performed from the tracheal bifurcation to the diaphragm. The field of view was adjusted according to the size of the heart. The cardiac CT was reconstructed at the end-systolic and the mid-diastolic phases using a slice thickness of 0.75 mm, an increment interval of 0.5 mm, and a medium-smooth convolution kernel of B36f. We used end-systolic CT images for this study.
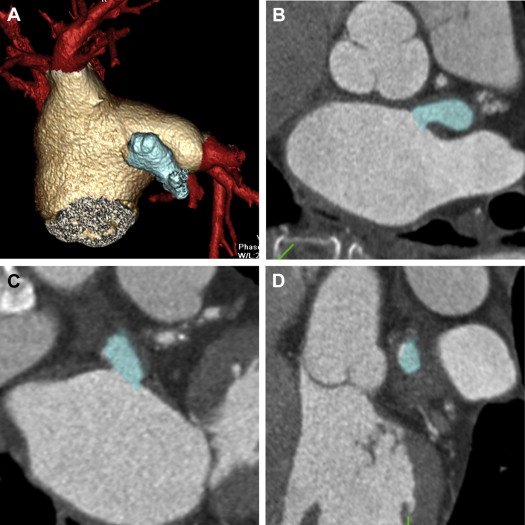
Two experienced radiologists (YJK and HJL, with 4 years and 8 years of experience with cardiac MDCT, respectively) measured the LAA long (D1) and short (D2) diameters by using the CT images and associated software (Vitrea; Toshiba, Japan). The LAA orifice was manually transected by multiplanar reformatted images. The size of the LAA orifice was defined by its narrowest portion. Then, cross-sectional views for LAA were produced by creating a plane perpendicular to the transverse multiplanar reformatted image ( Figure 1 ). Because the LAA orifice is elliptical in shape, we used the formula 0.785 × D1 × D2 as a surrogate value for the area.
LAA morphology was classified by the method reported by Di Biase et al. The Cactus LAA had a dominant central lobe with secondary lobes extending from the central lobe in both superior and inferior directions. The Chicken Wing LAA had an obvious bend in the proximal or middle part of the dominant lobe or folding back of the LAA anatomy on itself at some distance from the perceived LAA ostium. The Windsock LAA had 1 dominant lobe of sufficient length as the primary structure. Variations of this LAA type arise with the location and number of secondary or even tertiary lobes arising from the dominant lobe. The Cauliflower LAA had limited overall length with more complex internal characteristics. Variations of this LAA type have a more irregular shape of the LAA ostium (oval vs round) and a variable number of lobes with lack of a dominant lobe.
Continuous variables that were normally distributed are reported as mean ± SD and were compared using Student t test. Categorical variables were reported as count (percentage) and were compared using Fisher’s exact test. To identify risk factors of stroke, we first used univariate regression analysis and then included statistically significant variables into a multivariate logistic regression model. A receiver operating characteristic curve was computed for the completed prediction model, and we chose a probability threshold for predicting the likelihood of a stroke. The Statistical Package for the Social Sciences (SPSS 18.0; SSPS Inc., Chicago, Illinois) was used to perform all statistical evaluations. p Values <0.05 were considered statistically significant.
Results
Table 1 lists a comparison of clinical characteristics between the stroke and no-stroke groups. The stroke group was older and had a greater prevalence of co-morbidities and higher CHADS 2 and CHA 2 DS 2 -VASc scores than the no-stroke group. The CHADS 2 and CHA 2 DS 2 -VASc scores were calculated according to the clinical status before stroke onset. Body mass index was lower in the stroke group than that in the no-stroke group. E/E′ ratio was significantly higher in the stroke group than that in the no-stroke group. Reasons for withholding anticoagulant therapy in the stroke group included stroke as the presenting symptom of AF (41%), low-risk patients (24%), unawareness (6%), physician discretion (19%), patient preferences (6%), history of bleeding (2%), and unknown reasons (2%). This study included patients who underwent TEE and CT during the same rhythm. In total, 137 (63%) patients had undergone TEE and CT during AF.
| Characteristics | Stroke | p Value | |
|---|---|---|---|
| No (n = 151) | Yes (n = 67) | ||
| Age (yrs) | 56 ± 10 | 66 ± 9 | <0.001 |
| Women | 33 (22) | 19 (28) | 0.30 |
| Paroxysmal AF | 98 (65) | 31 (48) | 0.02 |
| Persistent AF | 53 (35) | 36 (52) | 0.02 |
| Body mass index (kg/m 2 ) | 25 ± 3 | 24 ± 3 | 0.03 |
| Heart failure | 4 (3) | 3 (5) | 0.48 |
| Hypertension ∗ | 67 (44) | 46 (69) | 0.001 |
| Diabetes mellitus | 16 (11) | 17 (25) | 0.005 |
| Previous stroke | 0 | 0 | — |
| Dyslipidemia † | 33 (22) | 16 (24) | 0.74 |
| CHADS 2 score | 0.8 ± 1.0 | 1.6 ± 1.0 ‡ | <0.001 |
| CHA 2 DS 2 -VASc score | 1.0 ± 1.1 | 2.0 ± 1.3 ‡ | <0.001 |
| Ejection fraction (%) | 63.0 ± 7.5 | 64.1 ± 9.4 | 0.40 |
| E/E′ | 9.9 ± 4.1 | 12.6 ± 4.6 | 0.001 |
| Aspirin use | 78 (52) | 34 (51) | 0.90 |
∗ Hypertension was defined as systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg at 2 or more visits or medical history of hypertension.
† Dyslipidemia was defined by fasting triglyceride plasma levels ≥150 mg/dl and/or fasting total cholesterol ≥200 mg/dl and/or low-density lipoprotein-C ≥130 mg/dl and/or high-density lipoprotein-C <40 mg/dl, or current use of lipid-lowering medication.
Table 2 lists LA and LAA parameters measured by MDCT and TEE. The stroke group had larger LA dimensions and larger LA volume than the no-stroke group. LAA orifice area, LAA depth, and LAA volume were also significantly larger in the stroke group. LAA emptying velocity was lower in the stroke group than the no-stroke group. There was no significant difference in the number of LAA lobes between the 2 groups. Morphologic types of LAA were not significantly different between the 2 groups. In the same study period, 24 patients with nonvalvular AF and on anticoagulation developed ischemic stroke and underwent cardiac MDCT and TEE. When we added this population to the stroke group, the MDCT and TEE parameters did not change significantly ( Supplemental Table 1 ).
| Variable | Stroke | p Value | |
|---|---|---|---|
| No (n = 151) | Yes (n = 67) | ||
| LA features measured by MDCT | |||
| LA anterior-posterior dimension (cm) | 4.2 ± 0.6 | 4.7 ± 0.8 | <0.001 |
| LA volume (cm 3 ) | 144 ± 39 | 177 ± 53 | <0.001 |
| LAA features measured by MDCT | |||
| LAA orifice area (cm 2 ) | 3.0 ± 1.1 | 4.5 ± 1.5 | <0.001 |
| LAA depth (cm) | 2.6 ± 0.6 | 2.9 ± 0.7 | 0.02 |
| LAA volume (cm 3 ) | 13 ± 5 | 17 ± 7 | <0.001 |
| LAA lobe | 1.3 ± 0.5 | 1.3 ± 0.5 | 0.73 |
| LAA morphology type | 0.99 | ||
| Chicken wing | 77 (51) | 33 (49) | |
| Windsock | 42 (28) | 20 (30) | |
| Cactus | 17 (11) | 7 (10) | |
| Cauliflower | 15 (10) | 7 (10) | |
| TEE | |||
| LAA emptying velocity (cm/s) | 55 ± 20 | 36 ± 19 | <0.001 |
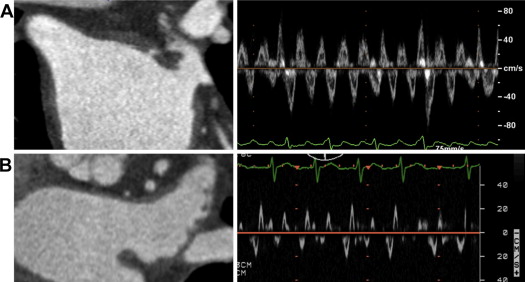
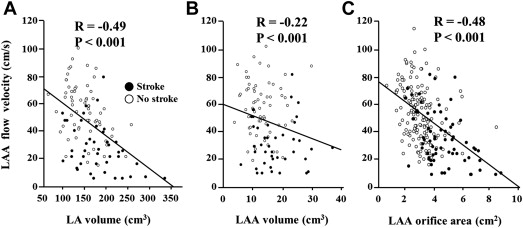
LAA orifice area was small, and LAA flow velocity was normal in no-stroke group ( Figure 2 ). However, stroke group showed an enlarged LAA orifice and decreased LAA flow velocity ( Figure 2 ). Figure 3 shows the relation between LAA flow velocity and the structural characteristics of LAA and LA. LAA flow velocity was shown to have a negative correlation with LAA orifice area (R = −0.48, p <0.001), LAA volume (R = −0.22, p <0.001), and LA volume (R = −0.49, p <0.001) ( Figure 3 ). Moreover, LAA flow velocity was negatively correlated with E/E′ ratio (R = −0.31, p <0.001). The LAA flow velocity of <37.0 cm/s predicted stroke with a sensitivity of 60% and a specificity of 81% with an area under the curve of 0.75. The LAA orifice area of >3.5 cm 2 predicted stroke with a sensitivity of 79% and a specificity of 78% with an area under the curve of 0.82.