Chapter 34 Imaging Patients with Chest Pain in the Emergency Department
INTRODUCTION
At the other end of the spectrum are patients with atypical and noncardiac chest discomfort who can be safely sent home. However, these patients represent only a small minority of patients with potential acute coronary syndrome (ACS). The majority of patients presenting with chest pain have an initial evaluation that is insufficient to either diagnose or exclude myocardial ischemia, and thus further evaluation is required. This group accounts for nearly two-thirds of ED chest pain patients.1,2
Standard tools and techniques currently used for the evaluation of all chest pain patients include the ECG, the history, and myocardial markers. The ECG is the first test performed for the evaluation of patients with potential myocardial ischemia. Although the presence of ischemic ECG findings can identify patients who will benefit from more aggressive pharmacologic and interventional treatment, diagnostic ECG changes are present in only a minority of patients with ACS.3 The history can be useful for risk stratifying patients into higher- and lower-risk groups, but in most cases, the substantial overlap prevents it use for determining who can be safely discharged from the ED.3
Another key component in the evaluation of chest pain patients are myocardial markers, particularly the troponins, which are considered the gold standard for diagnosing MI. Current recommendations are that all patients presenting with chest pain in the ED should undergo cardiac biomarker sampling, with repeat or serial sampling 6 to 8 hours later in those with initially negative markers (class I), with troponin being the preferred marker.3 However, as with the ECG, there are important limitations. First, all markers have a time-dependent rise and fall from their release to detection in the bloodstream, which takes at least 2 to 4 hours after MI onset. Second, by definition, markers of necrosis require myocardial damage to be released; therefore, they will be negative in patients who have ischemia only.
Because of these limitations, the standard evaluation process for patients who have a nonischemic ECG and a low-risk presentation typically involves admission to a chest pain observation area where serial biomarkers are performed to exclude MI. If negative, the patient subsequently undergoes provocative testing (typically treadmill testing without imaging) and is discharged if negative. If any part of the evaluation is positive, the patient is admitted for further evaluation. This approach has limitations because a significant minority of patients have an intermediate likelihood of coronary artery disease, or an abnormal rest ECG, or are unable to exercise adequately,4 limiting the number of chest pain patients eligible for an observational admission.
ACUTE MYOCARDIAL PERFUSION IMAGING
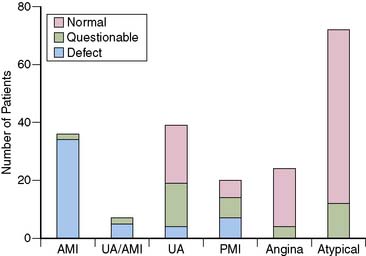
The first studies to evaluate the ability of rest MPI to identify ACS in chest pain patients were performed in the 1970s. Wackers et al.5 found a high diagnostic accuracy when planar thallium-201 (201Tl) imaging was performed in 203 patients admitted for possible MI. Images were abnormal in all 34 patients who had MI, as well as in 27 of the 47 (58%) patients who had unstable angina. (Fig. 34-1). In contrast, none of the 98 patients diagnosed with stable angina or atypical chest pain had abnormal studies. Others, also using 201Tl in chest pain patients, subsequently confirmed these results.6
Although imaging of chest pain patients using 201Tl appeared to be a promising tool, a number of limitations precluded its widespread adoption. Planar imaging has a lower sensitivity for detecting small areas of ischemia and ischemia in the posterior distribution, an area not often associated with diagnostic ECG changes. Because of its energy characteristics, relatively rapid redistribution, and imaging limitations in large patients, 201Tl is not an optimal agent for acute imaging. Although some attempted to overcome the logistical problems by using portable gamma cameras placed in the ED,7,8 these efforts were unsuccessful.
The development of single-photon emission computed tomography (SPECT) imaging, in combination with the availability of the technetium-labeled myocardial perfusion agents and their superior image quality, subsequently led to observational studies, followed by clinical trials demonstrating the utility of acute ED MPI. Technetium-99m (99mTc)-labelled sestamibi and tetrofosmin are taken up by the myocardium in proportion to blood flow, similar to thallium, but they lack significant redistribution.9 Therefore, patients can be injected while experiencing symptoms and imaged up to several hours later, making it possible to perform high-quality SPECT imaging outside of the ED setting in the absence of dedicated equipment.
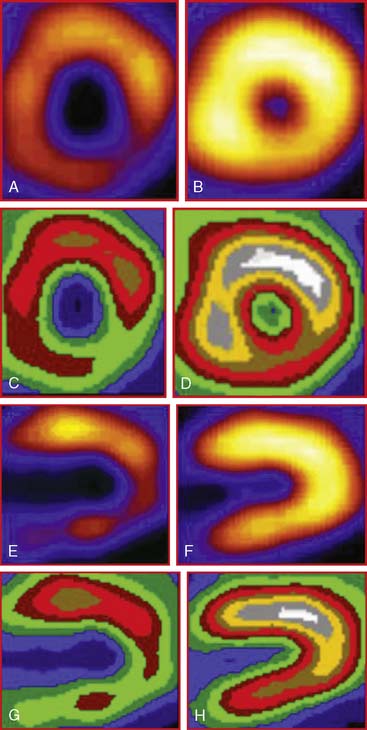
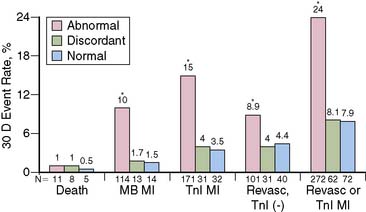
The favorable energy and dosimetry of 99mTc allows for gated reconstructions, an advantage not available at that time with 201Tl imaging. The ability to quantitate ejection fraction10 adds an additional prognostic component, identifying patients who may have unsuspected systolic dysfunction. More important, correlating wall motion and thickening with perfusion defects can be used to determine whether a defect reflects true ischemia or infarction or is the result of artifact or tissue attenuation.11 In the setting of acute infarction or ischemia, wall motion is typically abnormal; in contrast, an apparent perfusion defect in the presence of normal wall motion and thickening on gated SPECT usually indicates an artifact such as tissue attenuation (Fig. 34-2). The ability to perform simultaneous wall motion and perfusion significantly improves specificity12 and is particularly valuable in the acute setting where serial images are not available. Theoretically a patient could be injected during symptoms, and if imaged after symptom resolution, the wall-motion abnormality could resolve, and the defect could be misinterpreted as resulting from attenuation rather than ischemia. However, this appears to be infrequent in practice. Kontos et al. reported that for 2286 consecutive patients who were admitted for exclusion of ischemia following acute rest MPI, the proportion of patients who had troponin I (TnI) elevations (4.0 vs 3.5%), creatine kinase (CK)-MB MI (1.7 vs 1.5%), or who underwent revascularization (5.5 vs 5.2%), was not different between those who had normal perfusion and function and those who had perfusion defects but had normal wall motion in that area. In contrast, those who had perfusion defects associated with abnormal wall motion were significantly more likely to have TnI elevations (15%), CK-MB MI (10%), and undergo revascularization (17%) (Fig. 34-3).12 A potential explanation is that the severity of ischemia that occurs with an ACS event is associated with underlying myocardial stunning13,14 and persistence of wall motion abnormalities.
The combination of perfusion and wall motion has prognostic value. In a recent multicenter study reported by Kaul et al., perfusion plus regional function provided significantly greater diagnostic and prognostic value when compared to perfusion alone for predicting outcomes in 163 patients with possible ACS.15
DIAGNOSTIC VALUE
Sensitivity in Acute Myocardial Infarction
The first studies to demonstrate the high diagnostic accuracy using SPECT imaging with sestamibi for evaluating chest pain patients were performed in select populations of admitted patients. In a proof-of-concept study, Christian et al. performed early MPI in 14 patients without ST-segment elevation (most of whom had ST-segment depression) who were diagnosed with MI and who later underwent coronary angiography.16 Abnormal studies were found in 13 of the 14 patients. The amount of myocardium at risk averaged 20% ± 15% (range 2% to 53%) of the left ventricle, and half had either the left circumflex or a ramus branch as the culprit artery.
In one of the first studies to evaluate ED patients, Hilton et al. imaged 102 patients who presented to the ED with typical angina and a nonischemic ECG.17 Only 1 of the 70 patients with a normal MPI had an event, compared to 2 of the 15 with an equivocal MPI (13%), and 12 of the 17 (71%) with abnormal MPI. In a multivariate analysis, the only independent predictor of cardiac events was abnormal MPI.
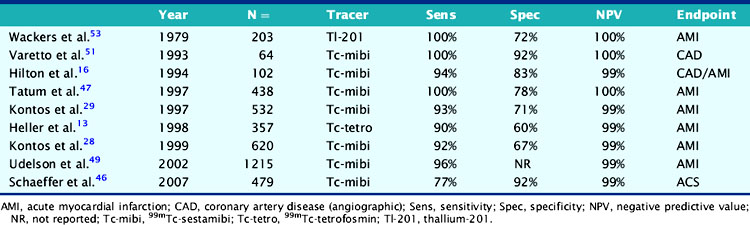
Numerous subsequent studies that included single-center and multicenter observational studies, as well as a randomized trial, were performed in large numbers of heterogenous patients undergoing an ED chest pain evaluation. They consistently found a high sensitivity (90% to 100%) for detecting acute MI (Table 34-1). Because sensitivity is not perfect, the results of acute MPI cannot be interpreted in isolation but must be placed in context with the clinical evaluation. However, infarcts that are present despite normal acute MPI are typically small, non-Q-wave infarcts and associated with an uncomplicated clinical course.
Table 34-1 Diagnostic Accuracy of Rest Myocardial Perfusion Imaging in Patients with Acute Chest Pain Syndrome and Normal or Nonischemic Rest Electrocardiograms
In contrast to most diagnostic tools that have not been evaluated in a randomized trial, the ability to safely discharge a patient after negative acute MPI was confirmed in the Emergency Room Assessment of Sestamibi for Evaluating Chest Pain (ERASE) study.18 A total of 2475 patients were randomized to routine care or ED MPI, in which patients were injected with sestamibi in the ED and then underwent acute imaging, with the results called back to the ED physician.18 All patients, whether admitted or discharged, underwent subsequent marker analysis and further diagnostic evaluation with either stress testing or coronary angiography. There was no difference between the two groups, in the percentage of ACS patients with MI (97% versus 96%) or unstable angina (83% versus 81%) who were admitted with one MI patient from each group discharged from the ED. However, there was a significantly lower admission rate and a higher rate of direct discharge from the ED in the ED MPI arm of the study compared to the standardized care arm. Importantly, this was a consistent effect seen at six of the seven institutions involved in the trial.
These results were confirmed in a subsequent smaller randomized trial. Candell-Riera et al. randomized 222 low-risk chest pain patients to either acute rest MPI or conventional management in the ED. Fewer patients undergoing rest MPI were admitted (18% versus 33%; P < 0.03), and overall ED time was shorter (13 ± 6 versus 16 ± 9 hours; P < 0.01).19
A limitation of the mentioned studies is that acute MPI was performed predominantly in low-risk patients, so relatively small numbers of patients who had MI were included in any one study, resulting in an imprecise estimate of sensitivity. To address this, Kontos et al. analyzed results from 141 consecutive patients who underwent ED MPI and were subsequently diagnosed with CK-MB MI.20 Overall sensitivity was 89% (95% CI: 83% to 94%), consistent with prior studies but with smaller confidence intervals. Similar to prior studies, patients with negative MPI had small MIs, with an average peak CK of 313 ± 227 U/L, compared to 590 ± 620 U/L (P < 0.001) in those with positive MPI. In addition, nonsignificant disease was found in the majority of patients with negative MPI who underwent coronary angiography.
Acute Coronary Syndrome Without Myocardial Infarction
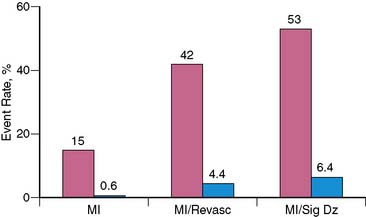
Although specificity of acute MPI appears low when MI is the only end point considered, this in part relates to one of its important advantages, the ability to identify patients who have ischemia alone. Bilodeau et al.21 imaged 45 patients without a history of MI who were admitted for unstable angina. The presence of a perfusion defect had a high accuracy (sensitivity 96%, specificity 79%) for predicting angiographic coronary disease in patients injected during an episode of pain, compared to a sensitivity of only 65% for the ECG. In another study Kontos et al. found that in 532 patients admitted after acute rest MPI in the ED, acute MI, as assessed by CK-MB elevations, was present in only 15% of patients with positive MPI (Fig. 34-4).22 However, the majority of patients with positive MPI had an end point consistent with ACS, including acute MI, subsequent revascularization, or significant coronary disease (>70% stenosis) on coronary angiography. Considering these as positive end points improved positive predictive value to 53%.
NEGATIVE PREDICTIVE VALUE AND PROGNOSIS
The negative predictive value in clinical studies has been consistently high and has typically exceeded 99% (see Table 34-1).18,23–26 The high negative predictive value for excluding significant ischemia allows effective identification of those who can be evaluated in lower-intensity settings other than the coronary care unit (CCU) or who can be discharged home. Patients with negative MPI have a low risk for both short- and long-term cardiac complications as well. Hilton et al.17 found that patients with normal MPI had an excellent prognosis, with no late events at 90-day follow-up. Similarly, Tatum et al. reported that patients with negative acute MPI had a cardiac event rate of only 3% during the subsequent year.26
INCREMENTAL DIAGNOSTIC VALUE
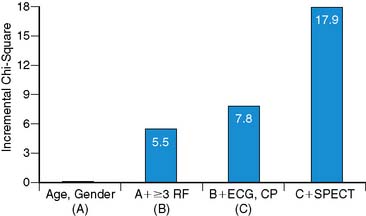
In the current cost-conscious environment, even though a new test may offer high diagnostic value, an additional requirement before adoption is that it also provides significant incremental value over the current standard of care. Kontos et al. found that in a multivariate analysis, abnormal MPI was the most important independent predictor of MI or revascularization in 532 patients who underwent acute ED MPI.22 Similarly, Heller et al. found that that abnormal SPECT was the most important multivariate predictor of MI in 357 patients who underwent acute MPI. In addition, acute MPI added significant incremental diagnostic value after consideration of demographic, clinical, and ECG variables (Fig. 34-5).23
In an interesting intent-to-treat survey study, Knott et al. performed acute MPI in 120 ED patients.27 The requesting physician completed a questionnaire before imaging, asking what the proposed management would be had the test not been available. They found there would have been a 34% reduction in overall hospital admissions and a 59% reduction in planned CCU admissions. Interestingly, overall CCU admissions were not reduced, because 17 patients initially considered low risk were admitted to the CCU after MPI was found to be abnormal, indicating a more appropriate utilization of resources.
COST-EFFECTIVENESS
Despite the application of relatively complex and expensive technology, ED MPI can be cost effective if the number of patients admitted is decreased.23,28,29,30 Several observational studies have confirmed that cost reductions occur when rest MPI is used as an integral part of patient management. In addition, a preliminary analysis from the ERASE study confirms that using ED MPI as a key part of the initial diagnostic strategy was indeed cost-effective, since costs were reduced a mean $70 per patient.31
Costs are reduced by a number of mechanisms. One obvious mechanism is discharging more low-risk patients directly from the ED rather than the patient being admitted or undergoing a more prolonged observation. Second, by identifying patients with atypical symptoms and a nonischemic ECG who have MI, inappropriate discharges can be averted. A third mechanism is more appropriate selection of diagnostic procedures, reducing the rate of coronary angiography in low-risk patients.27,28
Comparison with Troponin
Because most of the studies evaluating the use of acute MPI were performed in the 1990s, CK or CK-MB were typically used to diagnose MI. However, because of its high sensitivity and specificity for detecting myocardial necrosis, current guidelines recommend that cardiac troponin should be the diagnostic standard for MI.32 Since approximately 3% to 4% of the left ventricle must be ischemic to allow detection by MPI,33 it would be expected that use of a more sensitive cardiac marker such as troponin would identify more patients who have necrosis than would acute MPI. This has been supported by a number of small studies that reported that although the sensitivity of MPI was high, it was significantly lower than that of TnI or TnT.25,34
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree