Chapter 26 Imaging in Women
INTRODUCTION
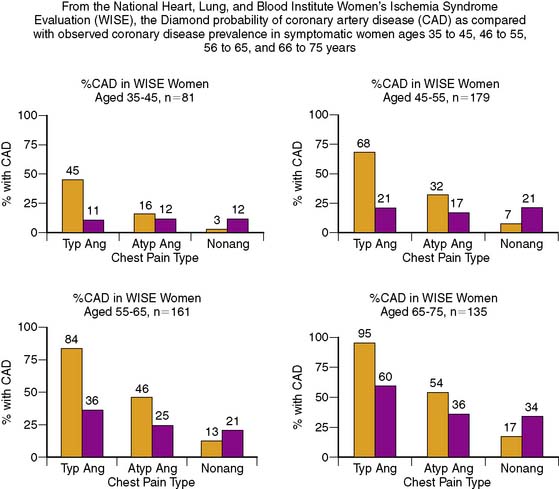
Despite recent declines in the rates of cardiovascular deaths in women, cardiovascular disease (CVD) is the leading cause of mortality in women.1 In the United States, more than 500,000 women each year will die of CVD, mostly coronary artery disease (CAD), more than in men (Fig. 26-1).1 This is not just a disease of aging women. Ischemic heart disease is the number one killer of women at all ages, and the mortality for younger women is greater than for men. Women younger than age 75 have higher in hospital mortality post myocardial infarction (MI), and until the age of 60 have higher 2-year post-MI mortality.2,3 There is a gap between these staggering statistics and a woman’s perception of her own health risk. With campaigns aimed at increasing awareness of the risk of heart disease in women, the recognition of heart disease as a women’s issue has improved, but in an American Heart Association (AHA) survey, only 13% of women identified CVD as their own greatest risk.4 Only 38% of these women reported that they had had a discussion with their physician about their risk for CVD, thus providing an opportunity for education and assessment.4
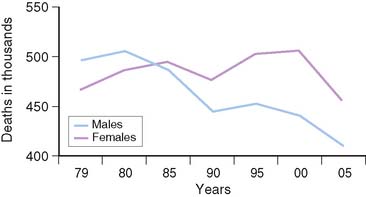
Figure 26-1 Cardiovascular disease mortality trends for males and females, United States (1979–2005).
(From NCHS and NHLBI.)
Women often experience typical symptoms of CAD, but there are gender differences in both how women present with acute coronary syndromes and the symptoms they report. Despite the fact that women present more commonly with unstable angina than with ST elevation MI, they have a higher mortality than men.5–9 Women appear to have less plaque rupture leading to ST elevation MI, and more plaque erosion resulting in unstable angina. In autopsy studies, women have less evidence of obstructive disease until the 7th decade of life.10 Two-thirds of women have fatal MI without recognized prodromal symptoms as their initial presentation of CAD.1 There is evidence that there are gender differences in pain perception, and this may contribute to the lack of specificity of typical anginal symptoms in women.11,12 Contributing to the challenge in diagnosing CAD in women is the variability in the reporting of chest pain as the predominant symptom in women who present with CAD. In one study, Milner et al. reviewed 550 individuals (41% women) who had evidence of ischemia or MI and found that both men and women reported chest pain with equal frequency.13 Women, however, were more likely to report an increased number of symptoms that were atypical, such as mid back pain, nausea, vomiting, dyspnea, palpitations, and indigestion. This increased symptomatology likely contributes to the difficulty in obtaining an accurate diagnosis of CAD in women. Other studies support the higher frequency of atypical symptoms and less chest pain prior to presentation as well as at the time of diagnosis. Women were more likely to describe back pain, jaw pain, rest pain, pain related to mental stress, and pain that awoke them from sleep.14–16 In a recent study, 515 women were surveyed 4 to 6 months post MI, and 43% did not describe any chest discomfort at the time of their MI.17 They did, however, report atypical prodromal symptoms, including unusual fatigue, sleep disturbance, and shortness of breath during the month before their MI, with only a minority reporting chest discomfort (29.7%).17 This variation in presentation and symptomatology has contributed to the difficulty in diagnosing heart disease in women and missed opportunities to diagnose and treat women with CAD.
Traditional risk factors for CAD are similar in men and women, but certain risk factors such as dyslipidemia and the presence of diabetes play a more important role in women. Elevated LDL levels play a central role in the development of CAD in both men and women, as evidenced by the linear relationship between LDL levels and risk for CAD. This is particularly true in women younger than 65 years of age.18–20 For women, the risk associated with elevated triglycerides has been shown to be an independent predictor of risk for CAD.21 Additionally, low HDL levels in women convey a greater risk than in men. For every 1 mg/dL increase in HDL, the risk of CAD decreases 3% in women, compared to 2% in men.22 Notably, the risk for death from CAD was more than two times higher in women with HDL levels below 50 mg/dL compared to those with levels above 60 mg/dL.18 Postmenopausal lipid levels are more atherogenic, with higher LDL and triglyceride levels and lower HDL levels.23,24
Although diabetes has a prevalence of 5% to 10% in both men and women, the risk for CVD is markedly higher in women. In a 20-year follow-up of the Framingham data, nondiabetic women had half the mortality rate of men.25 Those with diabetes had death rates equal to men, a disproportionate increase in mortality.
Metabolic syndrome, characterized by central obesity, hypertension, impaired glucose tolerance, low HDL-C, and elevated triglycerides affects almost a quarter of U.S. women.26 This dysmetabolic state increases the risk for the development of atherosclerosis and subsequent cardiovascular events.27 In women with suspected ischemia, Marroquin and investigators for the Women’s Ischemia Syndrome Evaluation (WISE) showed that there was a greater burden of atherosclerotic disease in those with metabolic syndrome compared to normal-metabolic women with angiographic evidence of disease (Fig. 26-2).27 This evidence illustrates the increased risk associated with the dysmetabolic state and alerts us to focus on preventive strategies in women at risk.
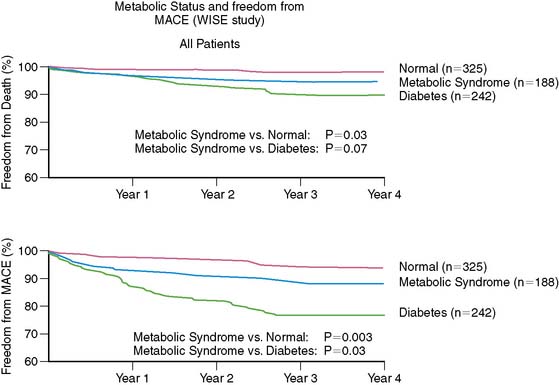
Figure 26-2 Event-free survival by metabolic status.
(From Marroquin OC, Kip KE, Kelley DE, et al., for the Women’s Ischemia Syndrome Evaluation Investigators: Metabolic syndrome modifies the cardiovascular risk associated with angiographic coronary artery disease in women: A report from the Women’s Ischemia Syndrome Evaluation, Circulation 109:714–721, 2004.)
While public awareness regarding the detrimental effects of tobacco appears to be increasing, the Surgeon General reported in 2001 that the overall rate of cigarette use in women is on the rise, particularly in younger, less educated women.28 The Nurses’ Health Study showed increased cardiovascular mortality with cigarette use, which declined after 10 years with smoking cessation.29,30 Age-adjusted mortality rates were substantially increased in women with diabetes who also smoked. In comparison to nonsmokers, the relative risk (RR) of smokers of 1 to 14 cigarettes a day was 0.92.29 This risk increased in a dose-dependent manner to an RR of 1.95 for those with a history of over 50 pack-years.29 For diabetic patients who smoked more than 15 cigarettes a day, the RR of a cardiovascular event was 7.67.30
DIAGNOSING CORONARY ARTERY DISEASE IN WOMEN
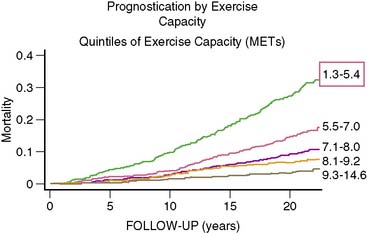
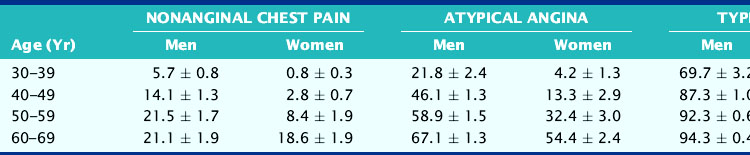
Diagnosis of CAD can be challenging in women, given the lower prevalence of obstructive disease, greater symptomatology, and lower functional capacity. Establishing the pretest likelihood of disease in a women is key in the diagnosis of CAD, balancing the probability of false positives when the disease prevalence is low with the need to avoid unnecessary additional and/or invasive testing. Diamond and Forrester analyzed the pretest probability of CAD as well as sensitivity and specificity in patients undergoing exercise electrocardiography.31 The prevalence of coronary disease by angiography was stratified into asymptomatic, nonanginal, atypical, and typical angina categories. Table 26-1 demonstrates interaction of gender and age with type of symptoms. Using this type of strategy can help further refine the likelihood of disease and hence direct the most appropriate testing, such as cardiac catheterization for high-risk individuals and exercise tolerance testing for low-risk individuals. In the WISE study, this strategy was found to overestimate the degree of obstructive disease (Fig. 26-3).32
Table 26-1 The Effect of Age and the Presence of Symptoms on the Probability of Underlying Coronary Artery Disease in Men and Women
There is growing recognition that women can have anginal symptoms, evidence of ischemia by exercise or noninvasive testing, but no evidence of obstructive disease at the time of cardiac catheterization. In the WISE study, women who had evidence of ischemia on phosphorus-31 nuclear magnetic resonance spectroscopy stress testing and no evidence of obstructive CAD had higher rates of hospitalization for anginal symptoms, repeat catheterization, and overall costs.32 Additional information from the WISE study showed that coronary microvascular dysfunction is seen in almost half of women with chest pain and nonobstructive disease.33 This group of women present a challenge in both diagnosis and treatment.
Exercise Tolerance Testing
In symptomatic women in whom the presence of CAD is uncertain, exercise tolerance testing (ETT) is the simplest and least expensive testing modality. In certain populations, such as women with a low likelihood of CAD and low disease prevalence, this test is appropriate and is supported by current guidelines. In this group, a negative exercise electrocardiographic response with normal hemodynamics has been associated with a high negative predictive value.34
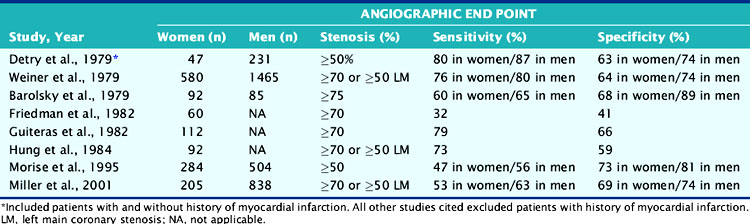
A major limitation of ETT is its compromised diagnostic accuracy (Table 26-2). A meta-analysis reported by Kwok and colleagues reported 15 studies with a sensitivity of 61% (range, 46% to 79%) and specificity of 69% (range, 51% to 86%).35 These testing results suggest a limited value of ETT alone in the appropriate diagnosis of CAD in women. Additionally, the increased age in women on presentation is concomitant with functional impairment. This results in reduced exercise capacity and inability to complete a diagnostic stress test. Other factors contribute to ETT being suboptimal: resting ST-T wave changes in hypertensive women, lower electrocardiogram (ECG) voltage, and hormonal factors.36–41 For example, endogenous estrogen has a digoxin-like effect, resulting in a false-positive ECG response, particularly midcycle when estrogen levels are highest.42 In an effort to determine the most cost-effective way to identify women at high risk for CVD, the What is the Optimal Method for Ischemia Evaluation in Women (WOMEN) Study is being conducted with intermediate- and high-risk women with chest pain or equivalent symptoms suggestive of ischemic heart disease. The study’s objective is to determine whether exercise ECG has the same negative predictive value for risk detection as gated myocardial perfusion single-photon emission computed tomography (SPECT) in women.43 Currently, use of the Framingham Risk Score (FRS) to predict the presence of disease may underestimate the degree of atherosclerosis. In the Multi-Ethnic Study of Atherosclerosis (MESA), 32% of women classified as low risk by FRS had evidence of coronary artery calcium indicative of atherosclerotic disease.44 These women also had higher rates of coronary artery disease and cardiovascular events.
Table 26-2 Sensitivity and Specificity of Exercise Tolerance Testing in the Diagnosis of Coronary Artery Disease
Women with diabetes are of particular concern. It has been recognized that such patients are at heightened risk for premature as well as accelerated atherosclerosis, MI, and cardiac death.1 It has also been reported that ECG is less reliable in diabetic patients,45 so in diabetic women, ETT alone may be particularly misleading (see Chapter 22).
Despite these limitations, if exercise testing is to be used in women, interpretation of the test should include factors in addition to ST-T segment depression.46,47 This should include parameters such as changes in ST/heart rate and the Duke Treadmill Score. Despite the described limitations, it should be also noted that the American Heart Association/American College of Cardiology (AHA/ACC) Guidelines recommend exercise testing in women with intermediate likelihood of CAD.48 Generally, optimal diagnostic stress testing is assumed when a patient achieves 85% or greater of predicted maximal heart rate. However, in deconditioned women, a hyperexaggerated response may yield a rapid and marked increase in heart rate. The test should be continued, and if a female patient cannot achieve at least 5 metabolic equivalents (METs) of exercise, they should be considered a candidate for pharmacologic myocardial perfusion imaging.38 Women with lower functional capacity have been found to have higher prevalence of cardiovascular risk factors, angiographic evidence of CAD, and adverse events compared to those with higher functional capacity.49 Functional capacity is associated with better prognostic value than electrocardiographic evidence of ischemia.50 Exercise capacity is an important predictor of cardiovascular outcome in women, and unless functional capacity is significantly limited, all stress testing should be done with exercise (Fig. 26-4).38
Stress Myocardial Perfusion Imaging in Women
Stress myocardial perfusion imaging (MPI) was first developed to offset the limitations of ETT in the accurate diagnosis and location of CAD in patients. Using exercise as the stress modality, radionuclide perfusion imaging with thallium (Tl)-201 has been shown to have on average a sensitivity of 83% and specificity of 88% using planar imaging.51 This represents approximately 20% to 25%, improvement in diagnostic accuracy in comparison to ETT alone. However, a considerable number of laboratories are now using SPECT and technetium (Tc)-99m-based imaging agents. SPECT imaging studies have been shown to be more accurate than planar imaging in the diagnosis of CAD and in separating single-vessel from multivessel disease.51
Of considerable importance, Stratman and colleagues demonstrated for all levels of exercise that Tc-99m-sestamibi SPECT imaging was significantly more sensitive in the detection of CAD than ECG with exercise data alone.52 Several studies have noted improved diagnosis of multivessel disease in comparison with planar methods. Unfortunately, few studies are available in women alone.
Pharmacologic Myocardial Perfusion Imaging (See Chapter 15)
An important advantage of MPI is the ability to assess patients unable to complete adequate exercise. For such patients unable to achieve 85% maximally predicted heart rate, the diagnostic utility of the exercise ECG falls precipitously.53–54 In such circumstances, MPI with pharmacologic stress provides an important and diagnostically useful alternative (see Chapter 14).
It has been estimated that 35% to 40% of all stress MPI is performed with pharmacologic stress. The most common pharmacologic type is that of vasodilator stress with either dipyridamole or adenosine. Pharmacologic vasodilator stress MPI has been shown to be comparable between dipyridamole and adenosine using either planar or SPECT imaging.55 Similar results have been reported with Tc-99m imaging agents.56
For women, Amanullah and colleagues found high sensitivity and moderate specificity ranges with adenosine in women despite their symptom complex. The sensitivity and specificity in nonanginal versus anginal symptoms was 93% and 69% versus 92% and 83%, respectively.56 They then compared sensitivity and specificity with respect to pretest probability of CAD. The sensitivity ranged from 82% and increased to 95% with a high-likelihood status. Given the fact that woman’s symptoms are more difficult to decipher clinically, these data support the use of adenosine MPI in evaluating symptomatic patients for CAD. Studies using another vasodilator, dipyridamole, have shown a sensitivity of 87% in women for detecting single-vessel disease.55 A retrospective review of women and men who underwent dipyridamole with 99mTc-sestamibi and cardiac catheterization surprisingly demonstrated an improved sensitivity for detecting left anterior descending (LAD) disease in women compared to men.57 These findings suggest the diagnostic accuracy of pharmacologic stress MPI is high regardless of the agent and should be used in women unable to exercise.
Dobutamine is an alternative for women with contraindications to vasodilator stress (reactive airway disease). This agent depends on a chronotropic response, and data suggest a similar accuracy to vasodilators. However, as with exercise, the accuracy of dobutamine is heart-rate dependent.58
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree