Chapter 27 Imaging for Preoperative Risk Stratification
INTRODUCTION
The evaluation of preoperative cardiac risk in patients undergoing noncardiac surgery has been a challenging and important topic over the past 25 years. The incidence of perioperative cardiac mortality has declined in recent years, but the prevalence of both coronary artery disease (CAD) and noncardiac surgical procedures in the United States1,2 is predicted to significantly increase over the next 30 years. Therefore, preoperative evaluation for cardiac risk will continue to be an important issue for surgeons, cardiologists, and medical consultants.2–6
This chapter will review the use of nuclear cardiology myocardial perfusion imaging (MPI) for preoperative and long-term risk stratification, including recommendations from the recently revised 2007 Guidelines on Perioperative Cardiovascular Evaluation and Care for Noncardiac Surgery2 for which patients benefit from preoperative imaging. The recommendations for preoperative risk assessment in the current Guidelines are also included in the recent American College of Cardiology/American Heart Association SPECT (single-photon emission computed tomography) Appropriateness criteria.7 Although controlled prospective randomized clinical trials are lacking, there are many retrospective reports and a few meta-analyses that demonstrate the utility of MPI in this evaluation process. We will focus on the evaluation of ischemia and left ventricular (LV) function, both of which have been shown to have significant prognostic utility for cardiac events such as myocardial infarction (MI) or cardiac death8 in patients with CAD. The issues of perioperative medical therapy and revascularization will also be reviewed.
The 2007 revised Guidelines divide preoperative clinical cardiac risk assessment into five steps.2 Overall clinical risk is determined by individual patient risk factors, the risk of the surgical procedure, and the patient’s functional capacity. This initial clinical evaluation can determine which patients may warrant further risk stratification with stress MPI.
STEP THREE: DETERMINE WHETHER THE PLANNED PROCEDURE IS LOW-RISK SURGERY
The type of surgery has an important impact on perioperative risk. In Table 27-1,2 the major types of surgical procedures are divided into high-, intermediate-, and low-risk groups. High-risk surgery, with a combined perioperative MI/cardiac death rate greater than 5%, includes major vascular, aortic, and peripheral vascular surgery that often warrants preoperative assessment with MPI. Intermediate-risk surgery includes intrathoracic, intraperitoneal, orthopedic, prostate, and head/neck surgery. Low-risk surgery includes superficial, endoscopic, breast, cataract, and ambulatory surgery. An important change in the 2007 Guidelines is the recognition that preoperative MPI rarely changes management of patients undergoing low-risk surgery, even in patients with clinical risk factors and poor functional capacity. Therefore, low-risk procedures can generally be performed without additional preoperative imaging.
Table 27-1 Risk associated with Various Types of Surgery2
| High Surgical Risk: |
| Aortic and other major vascular surgery |
| Peripheral vascular surgery |
| Intermediate Surgical Risk: |
| Carotid endarterectomy |
| Head and neck surgery |
| Intraperitoneal and intrathoracic surgery |
| Orthopedic surgery |
| Prostate surgery |
| Low Surgical Risk: |
| Endoscopic procedures |
| Superficial procedures |
| Cataract surgery |
| Breast surgery |
| Ambulatory surgery |
STEP FOUR: ASSESS FUNCTIONAL CAPACITY
A key factor in the Guidelines for predicting perioperative cardiac risk is the patient’s functional capacity, which can be estimated from a careful history of daily activity or determined with exercise stress testing. The Duke Activity Status Index9 can be used to approximate the metabolic equivalents (METs) for many daily activities. If the patient can exceed 4 METs with daily activity without symptoms (climbs one to two flights of stairs, performs own housework, or exercises regularly), then that patient will typically have sufficient cardiovascular reserve to tolerate the stress of surgery. The 2007 revised Guidelines recognize that stress MPI is unlikely to alter management in asymptomatic patients with good functional capacity. In contrast, symptomatic patients or those with very limited functional capacity may have poor cardiovascular reserve, with worse perioperative and long-term outcomes after noncardiac surgery.
STEP FIVE: ASSESS CLINICAL RISK IN SYMPTOMATIC PATIENTS OR PATIENTS WITH POOR/UNKNOWN FUNCTIONAL CAPACITY
Although the clinical question that is often posed to the medical or cardiac consultant is whether or not to “clear” the patient for noncardiac surgery, the Guidelines2 suggest an overall conservative approach to the use of expensive tests and interventions. The real challenge is in symptomatic or mildly symptomatic patients who are being evaluated for elective surgical procedures. A detailed medical history, physical examination, and electrocardiogram (ECG) should include information about angina, prior MI, CHF, symptomatic arrhythmia, diabetes, peripheral vascular disease, and prior history of coronary angiography or revascularization procedures. Even in the presence of known CAD, the risk of perioperative death or MI is less than 1% in patients who have undergone revascularization within the previous 4 years.10 It is also reasonable to proceed to surgery if the patient has had a recent coronary angiogram or stress test that reveals favorable results with no change in clinical symptoms. However, the presence of cardiac symptoms or prior cardiovascular disease, as already noted, should alert the consulting physician to consider further noninvasive testing. This decision to consider further testing such as stress MPI in patients with poor functional capacity can be made based on clinical risk factors and surgical risk.
Clinical Risk Score
Since the initial report by Goldman et al.11 demonstrated the utility of a clinical risk score for prediction of perioperative risk, several authors have published similar clinical risk scores based on the presence of clinical cardiovascular disease, diabetes mellitus (DM), renal disease, or other medical comorbidities.11–13 The 2007 Guidelines incorporate the Revised Clinical Risk Index developed by Lee et al.13
Lee et al.13 evaluated a total of 4315 patients undergoing elective noncardiac surgery. They derived a simple clinical index of six factors that could predict perioperative cardiac events: The presence of high-risk surgery, a history of CAD, history of CHF, history of cerebrovascular disease, diabetes treated with insulin, and a serum creatinine above 2 mg/dL constitute a useful index for risk assessment. In a validation population, the authors noted that when zero to one of these six factors was present (74% of all patients), the postoperative cardiac event rate was less than 1%. In contrast, the event rate in patients with any two factors was 7% (18% of all patients), and in those patients with three or more factors (8% of all patients), the event rate was 11%. Therefore, the Revised Clinical Risk Index classified three-quarters of the patients as low risk. A decision to consider further testing such as stress MPI can be made based on the presence of the five clinical risk factors together with surgical risk (the sixth risk factor).
Surgical Risk
In addition to the patient’s clinical cardiac risk, the risk of the planned surgery (see Table 27-1) should be considered in the decision for preoperative MPI testing. As discussed, current Guidelines now recommend proceeding directly to low-risk surgery without preoperative imaging. High-risk vascular surgery or intermediate-risk surgery often warrants preoperative assessment with MPI when the patient’s clinical risk is increased and functional capacity is poor.
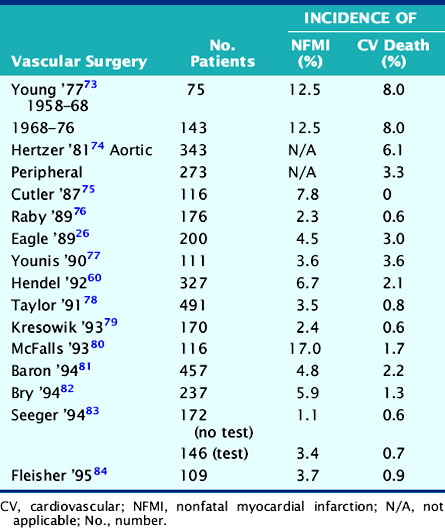
Vascular Surgery
Assessment of cardiac risk is of particular importance prior to elective peripheral vascular surgery, owing to the high prevalence (˜60%) of coexisting coronary artery disease.14,15 The incidence of nonfatal MI or cardiac death in this population is summarized in Table 27-2. These data show that although vascular procedures are considered high-risk surgery, the perioperative cardiac death rate for vascular surgery has fallen to less than 2% as a result of improved preoperative assessment and perioperative management. However, these data also show that although the rate of nonfatal perioperative MI has also decreased, it remains two- to threefold higher than perioperative cardiac death. Therefore, it appears that while preoperative assessment and perioperative management have resulted in a lower perioperative death rate, the ability to predict and prevent perioperative MI is more difficult. The observation that nonfatal perioperative MI is a powerful predictor of late cardiac events16–18 suggests the need to combine preoperative risk assessment with longer-term coronary management.
Transplant Surgery
The question of routine screening for all patients undergoing renal transplantation is primarily an issue of long-term cardiac prognosis. There is little immediate risk in performing transplant surgery, but it is clear that cardiac morbidity and mortality can have a significant impact on long-term postoperative survival. This seems to be especially true for patients with diabetes19 and can result in a policy of routine noninvasive stress imaging or coronary angiography in many patients before transplantation. Heston et al.20 have shown that an “expert system” using clinical risk predictors and thallium stress testing achieved an overall accuracy of 89% in predicting 4-year cardiac mortality among 189 renal transplant candidates. Other studies21,22 show that if there are no clinical risk predictors, such as a history of CHF, angina, insulin-dependent diabetes, age older than 50 years, or an abnormal ECG (excluding LV hypertrophy), no further cardiac evaluation is needed prior to renal transplantation.
In patients being evaluated for cardiac risk prior to liver transplantation, there has been little published experience. A study from Kryzhanovski and Beller23 suggests that perioperative cardiac risk is too low to warrant routine stress MPI or radionuclide angiography prior to liver transplantation. There were no cardiac events in 63 liver transplant procedures, and only one patient had a high-risk scan. Therefore, cardiac evaluations should be used in this patient subgroup only when there is clear evidence of coronary disease or when clinical risk factors are present.
THE DECISION TO OBTAIN PREOPERATIVE TESTING: A SHORTCUT APPROACH
After initial clinical assessment, a large group of patients with good functional capacity or those undergoing low-risk surgery can proceed to surgery without further testing. However, there remains a group of patients with clinical evidence of cardiovascular disease and poor functional capacity whose risk is uncertain or increased. Table 27-3 presents a shortcut approach to a large number of patients in whom the decision to recommend testing prior to surgery can be difficult. Basically, if all of the three listed factors are true, then the Guidelines suggest that noninvasive cardiac testing can be considered as part of the preoperative evaluation.
Table 27-3 Preoperative Risk: Shortcut Approach
RISK ASSESSMENT WITH PREOPERATIVE STRESS IMAGING
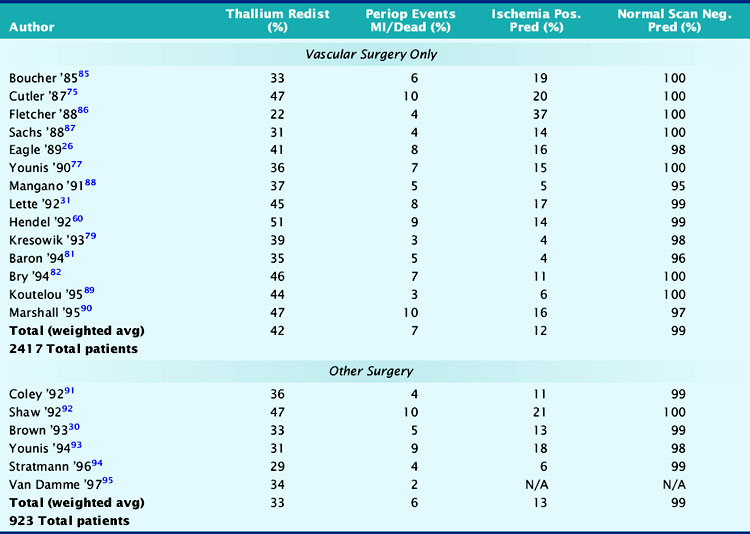
The utility of vasodilator (dipyridamole or adenosine) MPI imaging in more than 3000 patients is summarized in Table 27-4. In the upper section, all studies involved vascular surgery, and the incidence of thallium redistribution was 42%. The overall positive predictive accuracy of a reversible perfusion defect (ischemia) for prediction of perioperative MI or cardiac death is 12%. In the vascular surgery population, in which the prevalence of CAD is 60% to 70%, 38% (930/2417) of the patients have a normal stress perfusion scan. The average negative predictive accuracy is 99%, which indicates that a normal stress perfusion study is a powerful prognostic indicator.
The lower section of Table 27-4 summarizes similar results for patients with nonvascular surgery. Most patients in this section were studied because of increased clinical risk of CAD, and the overall event rate of 6% was similar to the vascular surgery group. It is interesting to note that although the incidence of thallium redistribution was somewhat lower, the positive and negative predictive values are similar to those noted in the vascular surgery group.
Shaw et al. reviewed the utility of preoperative noninvasive testing in a large meta-analysis.24 These authors reviewed stress imaging studies from 1985 to 1994 in which either dipyridamole thallium (n = 1994) or dobutamine echocardiography (n = 455) was used for perioperative risk stratification. Reversible perfusion defects were noted in 26% of patients, and perioperative nonfatal MI or cardiovascular death occurred in 9% of these cases. In contrast, 430 (22%) patients had normal perfusion scans with an event rate of 1.4%. Similar prognostic utility was noted in the dobutamine echocardiography studies. New wall-motion abnormalities during dobutamine-induced stress were noted in 39% of the patients, and 11% of these patients had a major cardiac event. In the 270 (61%) patients without new regional wall-motion abnormalities, the event rate was 0.4%. The authors of this meta-analysis concluded that (1) reversible perfusion defects have significant positive predictive accuracy, but the overall accuracy depends on the prevalence of CAD and clinical risk factors; (2) dobutamine-induced wall-motion abnormalities predict adverse outcomes, but the relatively small population size yields wider confidence limits; (3) the use of semiquantitative image analysis for MPI should improve its prognostic utility; and (4) fixed defects predict long-term cardiac events with an accuracy equal to reversible defects for perioperative events.
The issue of a possible gender difference in perioperative risk stratification was studied by Hendel et al.25 This study of 567 vascular surgery patients showed that, overall, perioperative and long-term cardiac events were similar for both men and women. Clinical predictors of cardiac risk were less useful in women versus men. ECG ST-segment depression with dipyridamole infusion predicted increased perioperative risk for men but not for women. An important finding was that multivariate analysis showed thallium redistribution to be an independent predictor of risk for both men and women.
Several authors have evaluated the use of clinical risk factors to identify the intermediate, risk patients who most benefit from preoperative stress MPI. Eagle et al.26 evaluated the utility of preoperative dipyridamole thallium MPI in 200 patients undergoing vascular surgery. In the 32% of patients at low clinical risk, with no DM or clinical risk factors for CAD, the perioperative rate of cardiac death, perioperative MI, pulmonary edema, or unstable angina was 3.1%. Thallium redistribution stratified the 54% of patients at intermediate risk (one or two risk factors) into a low-risk group with a perioperative event rate equal to that for patients with no risk factors and a high-risk group with a perioperative event rate of 30%. Therefore, these data support the current recommendation to reserve preoperative stress MPI for patients with clinical risk factors.
L’Italien et al. showed similar results in a multicenter analysis of over 1081 patients undergoing vascular surgery.27 In this study, clinically low-risk patients with a 3% perioperative event rate and high-risk patients with a 19% event rate were not more accurately risk stratified by preoperative dipyridamole thallium MPI. However, clinical assessment classified 51% of the patients as being at intermediate surgical risk, and stress thallium MPI effectively separated more than 80% of these intermediate-risk patients into low-risk or high-risk groups.
In a prospective clinical trial of patients undergoing abdominal aortic surgery, Vanzetto et al.28 identified patients at increased clinical risk based on the presence of two or more of the following predictors: age older than 70 years; history of MI, angina, CHF, DM, hypertension with LV hypertrophy; or a resting ECG that shows Q waves or ST-segment ischemia. Of 457 patients, 69% were classified as low risk and underwent surgery without preoperative stress testing. There was a 4% event rate in patients with one risk factor and a rate of approximately 2% in patients without any CAD risk predictors. One hundred forty-seven (32%) of the patients were classified as increased risk, and subsequently, 134 of these 147 patients underwent surgery after dipyridamole SPECT thallium scans. On the basis of these clinical criteria alone, 9% of the higher-risk patients had cardiac events. The perioperative rate of cardiac death or MI was 13% in patients with abnormal perfusion scans, compared to 1.9% in those with normal MPI. It is also important to add that Vanzetto et al.28 performed a multivariate analysis that showed that the number of ischemic segments was the single best predictor of perioperative events.
In another study of preoperative cardiac risk assessment, Bartels et al.29 evaluated a strategy that emulated the ACC/AHA recommendations for cardiac risk. Clinical risk classifications were assigned to 201 patients who were to undergo major vascular surgery. Approximately 10% of the patients were defined as high risk based on the presence of major clinical predictors of cardiac risk, 40% at intermediate risk, and the remaining 50% at low risk. All the low-risk patients and the intermediate-risk patients (52%) with a functional capacity of greater than 5 METs based on a questionnaire (Duke Activity Status Index)9 proceeded directly to major aortic surgery without further testing. The remaining intermediate-risk patients (48%) who had a functional capacity of less than 5 METs on the questionnaire underwent noninvasive testing (40%) or intensified medical care (60%) before surgery. In the high-risk group, approximately half underwent noninvasive testing, and the other half received intensified medical treatment. Subsequently, five (6%) intermediate risk and two (9%) high-risk patients underwent preoperative coronary angiography, resulting in one coronary bypass procedure and two cancellations of further elective surgery. Cardiac events occurred in 5% of the high-risk group and in 9% of the intermediate-risk group patients. The low-risk group had an event rate of 2%.
Patients with a mildly abnormal preoperative MPI study can generally undergo surgery with medical treatment for coronary disease. However, when preoperative stress MPI indicates very high risk of a perioperative cardiac complication, the Guidelines recommend evaluation with coronary angiography. Identification of patients at the highest cardiac risk with stress MPI is based on detection of a large area of multivessel ischemia together with markers of LV dysfunction such as LV dilation, increased thallium lung uptake, and reduced left ventricular ejection fraction (LVEF). Brown et al.30 showed that ischemic defect size detected with dipyridamole thallium MPI correlated with surgical risk. A large reversible scan defect and DM identified patients at highest risk for perioperative cardiac events. Lette et al.31
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree