Hypertension: Context and Management
Heather Cohen Henri
Peter Rudd
Hypertension is a major cardiovascular risk factor that directly contributes to coronary artery disease, stroke, congestive heart failure (CHF), renal failure, and peripheral arterial disease (1). Optimal management of the condition depends on careful diagnosis, nonpharmacologic and pharmacologic treatment, parsimonious selection of tests, and practice efficiency.
Over the natural history of hypertension, early endothelial dysfunction and elevations of cardiac output usually evolve to increased peripheral vascular resistance, reflecting an array of genetic, environmental, and homeostatic factors. Early perturbations may be slight and reversible; subsequent chronic changes tend to be larger, slower, and irreversible.
Successful reduction in blood pressure (BP) and other cardiovascular risk factors can dramatically reduce the incidence of cerebrovascular and coronary morbidity and mortality, especially for individuals with the highest elevations of BP, those with multiple risk factors, and the elderly. Nonpharmacologic therapy may be sufficient for mild elevations in BP in patients without other risk factors. The large array of antihypertensive drug options necessitates individualization for particular patients and a thoughtful balance of antihypertensive efficacy, patient cost and convenience, and compelling indications and contraindications.
Introduction
During middle and older age, BP is strongly and directly related to vascular and overall mortality (2). Hypertension is the most common diagnosis cited in office visits to American physicians (3). BP-lowering agents are the most widely used prescription drugs among adults over age 65 (4). In 1998, Americans spent an estimated $109 billion in direct medical care costs attributable to hypertension and its complications (5).
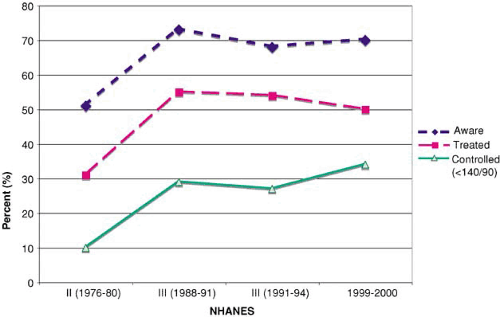
Of the known cardiovascular risk factors, hypertension is the most prevalent. It occurs in 65% of the U.S. population over age 60. In 2000, there were about 58 million Americans who could benefit from antihypertensive intervention. Hypertension’s prevalence increases with age, from 7% in individuals age 18 to 39 to 65% in individuals over age 59 (6). Most cases of uncontrolled hypertension occur in adults who do have access to health care and relatively frequent contact with physicians (7). Nevertheless, the percentage of hypertensives consistently controlled with medications has remained low: 25% (1988 to 1991) to 31% (1999 to 2000) (6). Figure 7.1 illustrates awareness, treatment and control of hypertension by gender and race/ethnicity from the NHANES 1999–2000 survey. Over the past decade, the prevalence of hypertension increased by about 10%. Nearly one third of respondents were unaware of their condition. Although two thirds were told to adopt lifestyle changes or take medications, only 31% achieved BP control of ≤140/90 mm Hg (8). Temporal trends show limited improvement in control over the past two decades.
Traditional definitions used systolic BP (SBP) >139 mm Hg and/or diastolic BP (DBP) >89 mm Hg to define hypertension. More recently, the recommendation shifted to defining normal BP as mean daytime SBP <120 mm Hg and DBP <80 mm Hg with pre- or established hypertension above these levels (9).
Clinical Profile
Natural History
Whether viewed as a distinct disease or as a cardiovascular risk factor, hypertension commonly produces structural changes in arteries and target organs in several patterns. During the prehypertension phase, repetitive perturbations of cardiovascular homeostasis occur, reflecting an array of hereditary and environmental factors. In time, these small changes accumulate and yield larger pathophysiologic changes that are recognizable as early hypertension. If the BP elevations are caught in time and reversed, normalization may occur. Reducing sodium intake, alcohol intake, and obesity lowered the incidence of hypertension from 19% to 9% in a 5-year trial of 201 individuals with high-normal BP (10). Patients with sustained elevations of
BP most often progress to established hypertension. A detailed discussion of the pathophysiology of hypertension appears in Chapter 100.
BP most often progress to established hypertension. A detailed discussion of the pathophysiology of hypertension appears in Chapter 100.
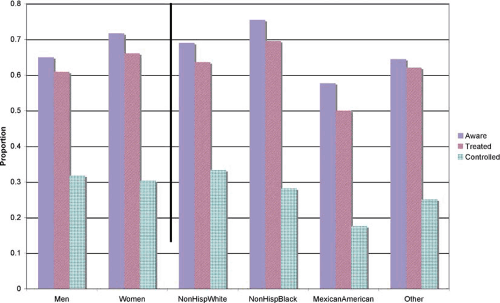 FIGURE 7.1. Awareness and management of hypertension by sociodemographic subgroups, NHAMES 1999–2000. |
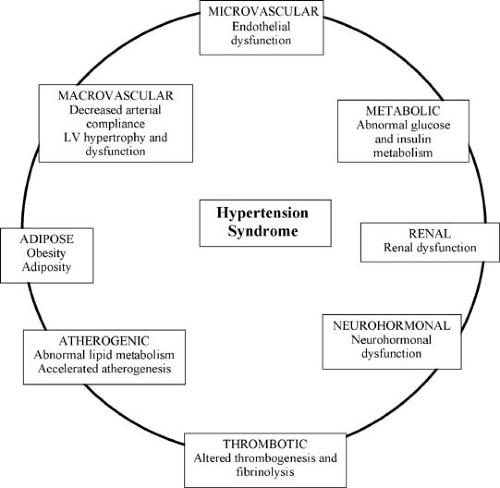
BP is only one factor among many that affects prognosis. Fewer than 5% of people with hypertension enter a fulminant course with rapid deterioration in cardiac, renal, and neurologic function. About half of hypertensives develop related end-organ damage if BP is left untreated over 7 to 10 years (11). The remaining patients exhibit a more indolent course with hypertensive complications occurring slowly, if at all (Fig. 7.2). The most common organ systems involved with destructive and remodeling processes include (a) the heart itself (diastolic
dysfunction, left ventricular hypertrophy, endocardial scarring, CHF, and coronary insufficiency), (b) the large- and medium-sized arteries (accelerated atherosclerosis, aneurysm formation with or without dissection), (c) the brain and intracranial circulation (ischemia, both hemorrhagic and thrombotic infarction), and (d) renal circulation (nephrosclerosis, with and without renal failure). These target organ complications reflect a cluster of contributing factors termed the hypertension syndrome (12). Figure 7.3 displays the pathophysiologic derangements of the hypertension syndrome.
dysfunction, left ventricular hypertrophy, endocardial scarring, CHF, and coronary insufficiency), (b) the large- and medium-sized arteries (accelerated atherosclerosis, aneurysm formation with or without dissection), (c) the brain and intracranial circulation (ischemia, both hemorrhagic and thrombotic infarction), and (d) renal circulation (nephrosclerosis, with and without renal failure). These target organ complications reflect a cluster of contributing factors termed the hypertension syndrome (12). Figure 7.3 displays the pathophysiologic derangements of the hypertension syndrome.
Effective treatment changes the natural history of hypertension-related end points, more for cerebrovascular than for coronary events. Hypertension carries a high risk for subsequent CHF, accounting for 39% of cases in men and 59% in women. Effective therapy lowers the overall relative risk (RR) of CHF in 12 randomized controlled trials to 0.48 (95% confidence interval [CI], 0.38 to 0.59) among treated versus control subjects (13). Among those younger than age 65, pulse pressure and SBP predict outcomes better than DBP (14). Over age 65, only elevated SBP and pulse pressure predict risk of adverse cardiovascular events and total mortality (15).
Preventing end-organ damage is more effective than trying to reverse the changes once established. Nevertheless, controlling BP after end-organ damage carries proven benefit. Among patients with prior stroke or transient ischemic attack, BP lowering reduces risk of dementia and cognitive decline (16). In patients with chronic renal failure, tight BP control slows decline in renal function (17).
Common Presentations
The vast majority of hypertensive patients (93% to 95%) display no demonstrable, curable abnormality of anatomy or physiology (18). Termed primary hypertension, the condition carries no consistent hallmark symptoms or signs, except for the elevated BP itself. Most cases are detected incidentally as part of routine examinations and generally in the absence of target organ damage at initial presentation. For the majority of hypertensives, specific symptoms and symptom levels do not correlate well with BP level, whether or not under medication treatment (19).
Establishing the Diagnosis
The Seventh Report of the Joint National Committee on the Detection, Evaluation, and Treatment of High Blood Pressure (JNC VII) defines prehypertension as indirect, sphygmomanometric levels of 120 to 139 mm Hg SBP or 80 to 89 mm Hg DBP, or both. Stage 1 hypertension is defined by 140 to 159 mm Hg SBP or 90 to 99 mm Hg DBP on the average of two or more seated BP readings on each of two or more office visits (9). Other groups have urged more stringent thresholds for high-risk populations in special danger of target organ damage, such as diabetics, infants, children, and pregnant women. The standard criteria are summarized in Table 7.1.
Appropriate diagnosis and management of hypertension require accurate and representative BP measurement. There is commonly a physiologic 15% to 20% variation in hour-to-hour BP readings. Studies using ambulatory BP monitoring (ABPM) reveal BP is generally highest during the day, lowest during sleep, and increases during the period from 4:00 AM to 12:00 PM, correlating with diurnal cortisol levels (20). Self-measurement correlates better with ABPM than office BP measurement (21).
Target organ damage and long-term prognosis correlate better with home self-measurement than with office BP measurements. In an 11-year cohort study of 1702 subjects with hypertension, the JNC VII classification had a stronger predictive
power of first transient ischemic attack or stroke using home BP measurements compared to clinic BP readings (22).
power of first transient ischemic attack or stroke using home BP measurements compared to clinic BP readings (22).
TABLE 7.1 BP Classification—Adults 18 Years or Oldera | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
No consensus currently exists about the optimal analysis for ABPM data, although the concept of BP load has gained special prominence. Load refers to the percentage of readings during which the SBP or DBP exceeds predefined limits (e.g., 140/90 mm Hg while awake and 120/80 mm Hg during sleep). Among patients with treated hypertension, a higher mean ABPM independently predicts cardiovascular events, even after adjustment for office measurements of BP and classic risk factors (23). Measuring BP outside the office helps to identify and address cases of apparent drug resistance, autonomic dysfunction, or when hypotensive symptoms are present (9,24).
Risk Assessment and Profile
When assessing a hypertensive patient, the clinician seeks to (a) confirm the existence and magnitude of hypertension, (b) assess the extent of end-organ damage, (c) evaluate for contributing comorbidities and risk factors, (d) screen for secondary causes of hypertension, (e) understand any special circumstances that may impact treatment over time, and (f) help to develop professional trust and the patient’s ongoing commitment for reducing cardiovascular risk. The most important components of initial and follow-up visits in the ambulatory setting are enumerated in Table 7.2.
The physical examination should search for target organ damage and evidence of atherosclerotic disease, concentrating on evidence for cardiomegaly or heart failure, vascular insufficiency, bruits, and possible stigmata of secondary hypertension such as thyromegaly. Other priorities include identifying comorbidities that can complicate therapy, such as diabetes or renal dysfunction, and calculating body mass index for cardiac risk stratification. Thorough neurologic assessment provides a baseline for hypertensive complications including dementia (25). Routine fundoscopy usually shows only arteriolar narrowing with elevated BP, but hemorrhages or exudates as well as swelling of the optic discs indicate the need for urgent treatment (26).
TABLE 7.2 Components of Ambulatory Antihypertensive Management | ||||
|---|---|---|---|---|
|
Useful initial tests for patients with hypertension include (a) urinalysis (screen for proteinuria), (b) serum potassium, sodium, creatinine (calculate glomerular filtration rate and screen for secondary causes), (c) thyroid-stimulating hormone (screen for hyperthyroidism), and (d) total cholesterol, high-density lipoprotein, fasting glucose, and/or glycosylated hemoglobin (risk stratification) (27). A resting electrocardiogram (28) may show left ventricular hypertrophy, presence of coronary artery disease, and conduction blocks, important when using antihypertensive medications that have nodal blocking activity. Extensive laboratory and imaging evaluation for secondary causes of hypertension is not routinely indicated unless suggestive history or refractory BP control appears (9).
Hypertension often keeps close company with other cardiovascular risk factors, including diabetes mellitus, hyperinsulinemia, dyslipidemia, and exogenous obesity (29). In combination, these risk factors are synergistic rather than merely additive. Obesity brings a two- to six-fold increase in the probability of developing hypertension (30) and accounts for 65% to 78% of its attributable risk (31). Among patients with concomitant hypertension and dyslipidemia, coronary artery disease prevalence more than doubles compared with those with either condition alone (32). Aggressive multifactorial risk factor intervention reduces mortality by nearly 30% among hypertensive patients with hypercholesterolemia, diabetes, or a history of smoking (33).
Smoking and alcohol use also contribute to cardiovascular morbidity. Cigarette smoking leads to endothelial damage and atherosclerosis. Consuming three or more alcoholic drinks a day increases BP, even when controlling for body mass index, cigarette smoking, and age (34).
Principles of Management
Goal of Antihypertensive Therapy
Antihypertensive therapy seeks to prevent cardiovascular morbidity and mortality. Nonpharmacologic diet and lifestyle changes remain essential for all patients, especially those with only modestly elevated BP. Drug therapy offers value for those with hypertension and those with prehypertension who have compelling indications, such as chronic kidney disease or diabetes (9). The benefit of therapy rises for those with higher pretreatment BPs (35) or multiple risk factors (36). Benefit of treatment accrues to both genders (37) and continues throughout older age (15).
Nonpharmacologic Treatment
Diet and lifestyle approaches, including weight loss, exercise, and dietary adjustment, may prevent and control of hypertension (38). Combining nonpharmacologic and pharmacologic therapy controls BP better than nonpharmacologic treatment alone (39). Table 7.3 summarizes recommendations for nonpharmacologic therapy.
TABLE 7.3 Recommendations for Nonpharmacologic Therapy | |||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||
Weight Reduction
Losing excess weight reduces SBP and DBP. The Trials of Hypertension Prevention, phase II (40) studied 2382 prehypertensive patients and achieved an average of 4.4 kg weight loss at 6 months and reduction of SBP and DBP by 3.7 and 2.7 mm Hg, respectively. In a study of patients with established hypertension, weight management associated with an average 7.8 kg weight loss yielded 7 mm Hg SBP and 5 mm Hg DBP reductions in clinic BP (41).
Most trials confirm that BP reduction is directly related to the weight loss achieved. If weight gain recurs, hypertension may return, but the long-term benefits of BP reduction persist. After 7 years of following 181 participants, body weight was similar in the weight loss and control groups, but the odds of developing hypertension in the weight loss group were reduced by 77% (P = .02) (42). Caloric restriction and regular physical activity remain the two basic ingredients for successful weight loss.
Exercise
Adding physical activity to a weight-loss program accelerates the weight loss and augments BP reduction (43). An addition of even a 20-minute daily walk can reduce the risk of incident hypertension by 29% (44). The precise mechanism likely involves decreases in cardiac output and peripheral resistance as well as modifications in serum norepinephrine levels, insulin sensitivity, electrolyte balance, neural and baroreflex mechanisms, and vascular structure (41,45).
Cardiovascular exercise training is the most effective type of exercise for the prevention and treatment of hypertension. In a review of 39 studies using predominately walking or jogging exercise, lower intensity exercise resulted in greater BP reduction than did high-intensity exercise. Combined random and nonrandom trials showed average reductions in SBP of -13 mm Hg and in DBP of -18 mm Hg in hypertensive patients. Training more than three times per week or for more than 50 minutes per session did not confer added antihypertensive benefit (46). Current recommendations specify that exercise should occur for 20 to 60 minutes, 3 to 5 days per week, at low to moderate intensity (47).
Dietary Adjustment
Some of the most dramatic evidence supporting nonpharmacologic therapy has emerged from the Dietary Approaches to Stop Hypertension (DASH) trial (48). The study evaluated 459 adults with prehypertension or stage 1 hypertension (<160/80 to 95 mm Hg) randomized to usual diet or to a diet with
increased fruits and vegetables with or without reduced total and saturated fat intake. During the trial, investigators kept patients’ sodium intake and body weight at constant levels. After 8 weeks, the combined dietary intervention reduced BP by 11.4/5.5 mm Hg versus 7.2/2.8 mm Hg achieved by increasing fruits and vegetables alone (P < .01). Remarkably, 70% of subjects on combination diet—versus 23% on usual diet—were normotensive at the end of 8 weeks (49). Recent data establishes the combination diet as sustainable (50) and particularly effective in groups at highest risk of hypertension-related end-organ damage (African Americans, those with hypertension, and patients over age 50) (51).
increased fruits and vegetables with or without reduced total and saturated fat intake. During the trial, investigators kept patients’ sodium intake and body weight at constant levels. After 8 weeks, the combined dietary intervention reduced BP by 11.4/5.5 mm Hg versus 7.2/2.8 mm Hg achieved by increasing fruits and vegetables alone (P < .01). Remarkably, 70% of subjects on combination diet—versus 23% on usual diet—were normotensive at the end of 8 weeks (49). Recent data establishes the combination diet as sustainable (50) and particularly effective in groups at highest risk of hypertension-related end-organ damage (African Americans, those with hypertension, and patients over age 50) (51).
The impact of reducing sodium on BP remains controversial, perhaps because salt sensitivity is heterogeneously distributed to a minority. In an unselected, normotensive population, there is insufficient evidence to recommend universal restriction of salt intake (52). In contrast, salt restriction may yield modest antihypertensive benefit among elderly hypertensives (53). Adding extra salt confers no medical value and possible harm. High sodium intake predicted mortality and risk of coronary disease among 2436 adults, independent of other cardiovascular risk factors including BP in a prospective trial (54) and cumulative mortality up to 27 years later (55).
There is consensus about the benefit of salt restriction among hypertensives (9). In the DASH-Sodium trial (56,57), subjects received the DASH diet or a typical U.S. diet and three levels of sodium (50, 100, and 150 mmol per 2100 kcal) for 30 days. Both the DASH diet group and the low-sodium groups had significant reductions in BP, but the greatest effect was seen in the combined groups (58). The benefit of BP reduction was greatest in the oldest subjects and in those with the lowest sodium intake. Moderate salt restriction with a target range of 90 to 130 mmol per day carries no associated adverse effects (52).
Importantly, sodium restriction often allows reduced need for antihypertensive medications, regardless of combination with weight loss (59). In one trial of sodium reduction with or without weight reduction among elderly hypertensives, over one third of patients were able to remain off their hypertensive medication, compared to only 16% who continued on their usual diet (60).
Adjustments in dietary and nondietary calcium supplementation may lower BP. In a meta-analysis of 42 randomized trials, calcium supplementation resulted in a small (about 1 mm Hg) but significant (P < .001) decrease in SBP and DBP (61). Recent data in elderly women demonstrate that adding vitamin D3 supplementation to calcium may confer additional benefit in lowering BP versus supplementation with calcium alone. During an 8-week trial of 140 women with 25-hydroxycholecalciferol levels below 50 nmol/L, 81% of subjects in the combined vitamin D3 and calcium group compared with 47% of subjects in the calcium alone group showed a decrease of at least 5 mm Hg SBP (P = .04) (62).
Most other dietary interventions appear to have trivial effects on BP. A randomized controlled intervention studying a low carbohydrate, high-protein, and high-fat diet (e.g., Atkins diet) did not significantly change SBP over 12 months (63). Reflecting a 1966–1996 Medline search, supplementing above the general dietary allowance of potassium and/or magnesium carries no demonstrable benefit in treating hypertension (64). More recently, isolated reports of mild benefit have appeared for potassium supplementation (65).
Alcohol Restriction and Smoking Cessation
Alcohol acts as a vasodilator at low doses (1 to 2 drinks per day) and as a pressor at high doses (66). Despite popular attention surrounding potential health benefits of red wine, there is insufficient rigorous evidence to recommend a “therapeutic” daily glass of wine (67). In contrast, among habitual drinkers there is ample evidence to recommend restriction of alcohol intake to two or fewer drinks. For individuals consuming four to six standard drinks a day, the pressor effect lasts throughout a 24-hour period (68). Alcohol may have a BP-lowering effect at 4 hours yet lead to BP elevations 10 hours later (69). Restricting habitual alcohol consumption can reduce BP in normotensive and hypertensive individuals (70). In a trial of hypertensive, alcohol-dependent patients, ethanol abstinence over a 24-hour period was associated with a decrease in mean BP of up to 12.5 mm Hg (71).
Among smokers, smoking cessation is commonly associated with a 3- to 4-kg weight gain and increased incidence of hypertension (72). Nevertheless, smoking cessation dramatically reduces overall cardiovascular risk.
Stress Reduction/Relaxation Training
For over 45 years, scientists have explored the relationship between mental stress and cardiovascular disease (73). Currently, insufficient evidence exists to support stress reduction as a principal or sufficient treatment for hypertension. Conflicting data exist as to whether high job stress alone is a predictor of subsequent hypertension or whether the methods used to cope with stress are more determinant (74). In a 5-year study of 292 healthy adult subjects, there was no increased risk among subjects with the highest perceived job stress, although 32% did progress to hypertension during the study period (75).
Although stress reduction programs have unclear impact on BP, device-assisted slow breathing shows promise. In a randomized study of 149 hypertensives, accumulated time spent in slow breathing resulted in significant decreases in BP. The greatest decreases in SBP (-15.0 mm Hg) were seen in subjects who spent more than 180 minutes over 8 weeks in device-assisted slow breathing. Postulated mechanisms involve effects on baroreceptor sensitivity, heart rate variability, and venous return (76). Additional studies of greater size and duration are needed before such BP-lowering techniques gain broad acceptance.
Pharmacologic Therapy
If 3 to 6 months of nonpharmacologic therapy fail to reduce BP to acceptable levels, the clinician should consider adding pharmacologic therapy or start it immediately along with nonpharmacologic therapy in patients with evidence of cardiovascular disease, target organ damage, or stage 2 hypertension (28).
The key goal is to lower BP to reduce adverse cardiovascular outcomes. In one study of 4736 hypertensive patients 60 years or older over a 5-year period, drug treatment lowered the RR of stroke by 36%, myocardial infarction by 27%, and total cardiovascular disease by 32% (77). BP lowering itself is of greater importance than the specific medication used (78). Thoughtful selection of appropriate single and combination drug therapy remains essential to maximize benefit and minimize adverse events.
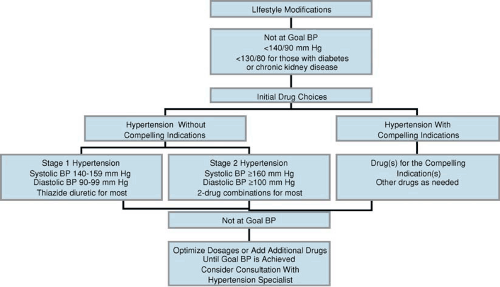
Figure 7.4 displays the JNC VII recommended pathway for treating hypertensive patients. No single approach or drug is appropriate for every patient. An individualized approach helps to tailor therapy for maximal effectiveness. Initiation of monotherapy and combination therapy should take into account compelling indications for and adverse effects from each antihypertensive drug. A summary of antihypertensive drug therapy appears in Table 7.4.
Individualized Approach
The most comprehensive strategy for selecting antihypertensive therapy is the individualized approach. It takes into account
several key components of each patient: profile of hemodynamics and pathophysiology, cardiovascular risk analysis, concurrent medical conditions and therapies, quality of life analysis, and cost. In essence, the customized approach corresponds to a type of “mosaic” model of treatment, incorporating a large number of variables that differ for each individual (79).
several key components of each patient: profile of hemodynamics and pathophysiology, cardiovascular risk analysis, concurrent medical conditions and therapies, quality of life analysis, and cost. In essence, the customized approach corresponds to a type of “mosaic” model of treatment, incorporating a large number of variables that differ for each individual (79).
Responding to the projected pathophysiology and hemodynamics, the clinician chooses medications to reverse the underlying circulatory dysregulation, lowering the vascular resistance, if elevated, while preserving cardiac output and maintaining perfusion to critical target organs: at rest, with exercise, and over the entire 24 hours.
Reflecting cardiovascular risk profile analysis, the clinician should avoid medications that likely worsen the known risk profile, such as using high-dose thiazides in a patient with elevated low-density lipoprotein cholesterol (80,81). The clinician should prospectively monitor those regimen-affected factors that impact risk and adjust the regimen to minimize overall risk, whether related to atherosclerosis, arrhythmias, congestive failure, or sudden death (82).
Aware of concurrent medical conditions and therapies, the clinician prescribes the fewest antihypertensive drugs to treat the greatest number of concomitant conditions, such as using β-blockers when the need for coronary prophylaxis and hypertension are present in the absence of limiting bradycardia or bronchospasm. Such therapeutic parsimony facilitates medication adherence by simplifying the overall regimen and minimizes adverse drug reactions and drug–drug interactions.
For regimen adherence, the clinician seeks to optimize the patient’s quality of life by considering physical and mental factors (83). For example, diuretic-based therapy may be more problematic in an older patient with incontinence (84). Similarly, β-blocker therapy has been associated with a small but significant increase in fatigue and sexual dysfunction (85). Such adjustments necessitate ongoing clinician–patient dialogue regarding disease- and treatment-mediated symptoms.
Rising health care expenditures, especially for medications, prompt both clinician and patient to consider cost. Key components include drug acquisition, concomitant treatment (e.g., potassium supplementation) and tests (e.g., monitoring serum potassium and renal function) (86), clinician visits, switching to a new agent after therapeutic failure or adverse event (87), and cost of not treating to goal BPs with attributable morbidity and mortality (88).
Best Options for Initial Monotherapy
The JNC VII recommends thiazide diuretics as the drug of choice for initial monotherapy in the absence of specific contraindications or compelling indications (9). In support, the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) comprises the largest randomized trial comparing outcomes with antihypertensive monotherapy. The ALLHAT trial compared a calcium channel blocker, angiotensin-converting enzyme (ACE) inhibitor, and thiazide diuretic among 33,357 hypertensive adults over a mean of 5 years (89). All-cause mortality did not differ among the groups, but the rate of heart failure was lowest in the diuretic group. Similar results have been seen in both black and non-black patients (90,91). In a meta-analysis of 42 trials designed to compare several antihypertensive drugs, low-dose diuretics were the most effective initial treatment for prevention of cardiovascular morbidity and mortality (92). Whereas BP reductions were similar between comparison groups for every outcome studied (coronary heart disease, CHF, stroke, cardiovascular disease events, cardiovascular mortality, and total mortality), no drug was significantly better than low-dose diuretics. When analyzed from a financial perspective, thiazide therapy is the least expensive hypertensive agent available with the atypical exception of vasodilator therapy (86).
Despite concern about links between thiazide use and elevated blood glucose, recent data show that thiazides did not
increase risk of developing diabetes among 12,550 hypertensive adults. In contrast, use of β-blockers was associated with a 28% higher risk of subsequent diabetes (93). Similarly, over a mean 14-year follow-up in the Systolic Hypertension in the Elderly Program (94), diuretic treatment versus placebo or atenolol in diabetics was associated with the most improved long-term outcomes.
increase risk of developing diabetes among 12,550 hypertensive adults. In contrast, use of β-blockers was associated with a 28% higher risk of subsequent diabetes (93). Similarly, over a mean 14-year follow-up in the Systolic Hypertension in the Elderly Program (94), diuretic treatment versus placebo or atenolol in diabetics was associated with the most improved long-term outcomes.
TABLE 7.4 Overview of Antihypertensive Medications | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||