Introduction
In the second half of the 20th century, cardiovascular diseases (CVD) became the dominant cause of global mortality and a major contributor to disease-related disability. At the beginning of the 21st century, this pattern has become even more pervasive as the CVD epidemic accelerates in many developing regions of the world, even as it retains its primacy as the leading public health problem in the developed regions.1–9
An estimated 17.5 million people died from cardiovascular diseases in 2005, representing 30% of all global deaths. Of these deaths, an estimated 7.6 million were due to coronary heart disease and 5.7 million were due to stroke. Over 80% of cardiovascular deaths took place in low-and middle-income countries and occurred equally in men and women.1 The low-and middle-income countries contributed 83.8% of all CVD deaths and 88.5% of disability-adjusted life-years (DALY) loss attributed to CVD that year.
Around 9 million stroke cases were reported to occur in 2004. Large geographic differences exist in the burden of stroke as well as its case fatality rates globally. There is an increasing trend in the incidence of stroke in developing countries as opposed to the decreasing or stabilizing trend in developed countries. While coronary heart disease (CHD) was the dominant form of CVD in the developed countries, Latin America and India, stroke was the leading cause of cardiovascular deaths in sub-Saharan Africa and China. Epidemiologic studies in developing countries provide evidence that stroke mortality rates tend to be higher than coronary heart disease rates, and may be considerably higher than in developed countries.1,2 In 2004, low-and middle-income countries contributed to 86.7% of global deaths due to cerebrovascular diseases. Hypertension and diabetes are more widely prevalent in stroke patients in developing countries as compared to developed countries.3
The rise and recent decline of the CVD epidemic in the developed countries have been well documented.9–12 The identification of major risk factors through population-based studies and effective control strategies combining community education and targeted management of high-risk individuals have together contributed to the fall in CVD mortality rates (inclusive of coronary and stroke deaths) that has been observed in almost all industrialized countries. It has been estimated that, during the period 1965 – 90, CVD-related mortality fell by 50% or so in Australia, Canada, France and the United States and by 60% in Japan.8 Other parts of Western Europe reported more modest declines (20 – 25%).9 The decline in stroke mortality has been more marked compared to the decline in coronary mortality. In the United States, the decline in stroke mortality commenced nearly two decades earlier than the decline in coronary mortality and maintained a sharper rate of decline.11 During the period 1979 – 89, the age-adjusted mortality from stroke declined, in that country, by about one-third while the corresponding decline in coronary mortality was 22%.11 In Canada, Japan, Switzerland and the United States, stroke mortality has declined by more than 50% in men and women aged 65 – 74 years since the 1970s.12 In Japan, where stroke mortality outweighs coronary mortality, the impressive overall decline in CVD mortality is principally contributed by the former.
However, recent trends in some of the developed countries have provoked some concern. A flattening of age-adjusted mortality rates for major cardiovascular diseases in the USA has been reported since 1990, with an especially well-documented absence of a decline in stroke mortality since that year. This has been accompanied by an increase in mortality from congestive heart failure. Lack of decline in incidence of CHD and stroke, fall in the rate of decrease in cardiovascular risk factor levels and rising levels of obesity since 1990 have all been incriminated as factors responsible for such a plateau effect on CVD mortality rates in USA over the past decade.13
Within Europe, there is a considerable variation in cardiovascular and all-cause mortality on both a national and a regional level. Mortality from both CHD and CVD has continuously been decreasing in most Western European countries over the last three decades. In most Central and Eastern European countries, on the other hand, cardiovascular mortality increased during the 1970s and 1980s and started to decline or stabilize in the early to mid-1990s. Despite the recent decrease, rates are considerably higher in most Central and Eastern European countries. With regard to cerebrovascular mortality rates, a different pattern is observed. Cerebrovascular mortality is reduced in the center of Western Europe, with the lowest national mortality rates in Switzerland, France, Norway, Spain, The Netherlands and Italy. Countries and regions with higher mortality rates surround this circle of reduced mortality such as the Central and East European Countries as well as some Mediterranean countries including Greece, Portugal and certain regions of Southern Spain and Italy.14
CHD, previously considered rare in sub-Saharan Africa, now ranks eighth among the leading causes of death in men and women. A wide variety of studies from Ethiopia, Ghana, Kenya, Nigeria, Tanzania and Zaire suggest that the incidence and prevalence of CVD is increasing, especially in urban and semi-urban areas.15 This is the result of adverse behavioral and lifestyle changes associated with urbanization and epidemiologic transition.
Developing countries like China and India have experienced an epidemiologic transition in a much shorter time than many countries. Mortality analysis of China shows that deaths due to chronic diseases have increased as a proportion of all deaths, from 41.7% in 1973 to 74.1% in 2005, with CVD being a major contributor. China already has 177 million adults with hypertension.16 An increasingly larger number are at risk of cardiovascular diseases because of smoking, dietary changes and reduced physical activity. In India, too, cardiovascular disease is now the leading cause of death, accounting for 29% of all deaths in 2005. The risk factors are also on the rise, as evidenced by a number of community surveys in different regions of the country. India is presently home to 40 million persons with diabetes and 118 million hypertensive individuals. These are projected to increase even further by 2025.17
Rheumatic heart disease (RHD) continues to be a burden in developing countries, although there is an overall decline in the incidence and deaths resulting from RHD. Of 12 million people currently affected by rheumatic fever and RHD, two-thirds are children between 5 and 15 years of age. There are around 300 000 deaths each year with 2 million people requiring repeated hospitalization and 1 million likely to require surgery in the next 5 – 20 years.18
Early age of CVD deaths in developing countries
Although the present high burden of CVD deaths is itself a reason for attention, a greater cause of concern is the early age of CVD deaths in developing countries compared to developed countries. Globally, more than 38% of CVD deaths occurred below the age of 70 years in 2002. Deaths from cardiovascular diseases in people younger than 70 years accounted for 21% of all deaths.19 Age-specific CVD mortality rates for those between 35 and 64 years have increased many-fold between 1984 and 2002 in less developed countries. This kind of concentration of CVD deaths among people of working age (35 – 64 years) is not seen in industrialized nations. In India, China, Russia and Brazil, 30 – 40% of the CVD deaths occur in people of working age. The Philippines has over 50% of its CVD deaths in this age group, 8 – 10 times higher than the Western experience.20
South Asians have a greater prevalence of coronary risk factors than the rest of the world, and coronary artery disease often manifests at an early age.21 Asians tend to have slimmer body build than Westerners, with less muscle mass and connective tissue than stockier subjects.22 Further, Asian populations have a different fat distribution pattern from the Western population and are more prone to central obesity, even at low BMI levels.23 Such considerations raise the possibility that the risks associated with adiposity at lower levels of BMI are greater in Asian population.
Epidemiologic transition and the evolution of the CVD epidemic
What is the “transition”?
The health status and dominant disease profile of human societies have been historically linked to the level of their economic development and social organization at any given stage. The shift from nutritional deficiencies and infectious diseases, as the major causes of death and disability, to degenerative disorders (chronic diseases like CVD, cancer, diabetes) has marked the economic ascent of nations as they industrialized. This shift has been called the epidemiologic transition.
The economic and social changes that propel this transition are related to a rise in per capita income, greater investments in public sanitation, housing and healthcare, assured availability of adequate nutrition and technologic advances in medical care. Life expectancy rises as causes of childhood and early adult mortality decline. This, in turn, leads to a decline in fertility. The age profile of the population changes from a pyramidal distribution dominated by the young to a columnar structure where adults and the elderly progressively expand their numbers. This has been described as the demographic transition. Since the disease profile is also linked to the age profile of the population, the health transition encompasses the effects of the epidemiologic and demographic transitions.
CVD profile at different stages of the epidemiologic transition
The model of epidemiologic transition originally described by Omran,24 with three phases (the age of pestilence and famine, the age of receding pandemics;,the age of degenerative and man-made diseases), was later modified to include a fourth phase (the age of delayed degenerative diseases).25 Life expectancy progressively increases from around 30 years in the first phase to over 70 years in the fourth phase. The shift to a dominant chronic disease profile occurs in the third phase. As the average life expectancy exceeds 50 – 55 years, the proportionate mortality due to CVD begins to exceed that of infectious diseases.26
The transition not only occurs between the broad disease categories but also within them. The disease profile within CVD alters at each phase of the epidemiologic transition. In the first phase (the age of pestilence and famine), CVD accounts for 5 – 10% of deaths.26 The major causes of CVD are, however, related to infectious and nutritional deficiencies. Thus, RHD and cardiomyopathies (e.g. Chagas’ disease) are the main CVD in this phase. Even as countries emerge from this phase, the residual burden of chronic valvular heart disease and congestive heart failure often remains for some period. These effects are still evident in sub-Saharan Africa and parts of South America and South Asia.26
In the second phase (the age of receding pandemics), the decline in infectious disease which accompanies socio-economic development ushers in changes in diet. As the subsistence nutrition changes to more complete diets, the salt content of the food increases. Hypertension and its sequelae (hypertensive heart disease and hemorrhagic stroke) now affect the population whose average age also has risen with increased life expectancy. Some residual burden of RHD and cardiomyopathies is also evident. These non-atherosclerotic diseases contribute to 10 – 35% of deaths. This pattern currently prevails in parts of Africa, North Asia, and South America.26
In the third phase (the age of degenerative and man-made disease), accelerated economic development and increased per capita incomes promote lifestyle changes in diet, physical activity, stress, and addictions. A diet rich in calories, saturated fat and salt is accompanied by reduced physical activity through increased use of mechanized transport and sedentary leisure time pursuits. The metabolic mismatch leads to obesity, increased blood lipids, diabetes, and elevated blood pressure. Tobacco consumption, especially cigarette smoking, starts as a pleasurable pastime and turns into a severe addiction. These factors result in the onset of clinically manifest atherosclerotic vascular disease (CHD, atherosclerotic stroke, and peripheral vascular disease) at around 55 years of age. Such patterns first occur in the upper socio-economic classes who have disposable income to expend on rich diets, tobacco and transport vehicles. Several countries in South America and Asia currently manifest this pattern. As the epidemic advances further and involves all social strata, with homog-enization of risk behaviors and risk factors across the population, the death toll of CVD rises to range between 35% and 65% of all deaths. This scenario is currently observed in Eastern Europe.
In the fourth phase (the phase of delayed degenerative disease), a number of changes occur in the society to modify risk behaviors and reduce risk factor levels in the population. Health research augments the knowledge of CVD risk factors. The desire to reduce the adverse impact of CVD on individuals as well as on society steers the community as well as the policymakers to apply this knowledge for disease prevention and health promotion. Community awareness through education, as well as its ability to exercise healthy choices through supportive regulatory measures, empowers its members to adopt healthier lifestyles. Saturated fat and salt consumption declines and leisure-time physical activity and exercise programs are avidly pursued. With concerns over the effects of active and passive smoking, tobacco consumption falls. Simultaneously, medical research makes available new technologies which are very effective in saving lives, modifying the course of disease, and reducing the levels of risk factors. All of these changes, in unison, delay the onset of disease, lower the age-standardized mortality rates and reduce the disability. The contribution of CVD to total mortality falls to 50% or below. These patterns are now established in most of North America, Western Europe, and New Zealand.26
Recent developments in some countries of Eastern Europe, with sharp declines in life expectancy and other health indices, led to a fifth phase of health transition being postulated.7 In this stage of “social upheaval and health regression”, the CVD spectrum too may witness a reversal with CHD and stroke occurring at younger ages, resulting in a fall in life expectancy, as in Russia. Further transition may also occur in the future, due to health impacts of global climate change and environmental degradation which can profoundly influence both infectious diseases and chronic diseases.
Variations in the tfransition
There are, however, variations on this theme. Even within Europe, for example, there is still a clear north-east to south-west gradient in mortality from CHD. With regard to the east – west gradient, dietary fat intake appears to play a major role. In Eastern Europe, higher consumption of saturated fat was reported during the 1980s and early 1990s. In Poland, changes in the dietary fat intake during the 1990s, leading to a more favorable ratio of polyunsaturated to saturated fat, were associated with a drop in mortality from CHD by approximately one-quarter. The attribution of single risk factors to regional variation may also vary depending on geographic location of the area of interest. For example, regional differences between Israel, Germany and Greece were found to be associated particularly with differences in blood pressure levels.14
The results of the Sino-MONICA study (1987–93) in China have shown large differences in the occurrence of coronary and stroke events, with higher rates in northern provinces and lower rates in southern provinces. This geographic difference in CVD mortality and incidence reflects underlying differentials in risk factor profiles (like hypertension and cholesterol levels).27,28 Prevalence of CHD in the Japanese population remains lower than that in the US and other Western populations. However, lifestyle changes in recent decades have been accompanied by the increasing prevalence of hypercholesterolemia and diabetes, and recent data indicate an increase in prevalence of CHD.29 The prevalence of lipid risk factors in younger Japanese people is now similar to that in the US.
The question of “arrested epidemiologic transition” is also raised with respect to some of the developing countries. If poverty continues to be a major problem for them, will they experience the CVD epidemic in its full fury or will the pre-transitional diseases of nutrition and infection continue to occupy the center stage? Even now, there is evidence that the social gradient has begun to reverse for risk factor levels and even for morbidity measures in some populations in the developing world.5 Unless economic development is greatly stunted in some countries, it is likely that the model of epidemiologic transition will be applicable to most of the developing world.
The transition to the atherothrombotic phase of the epidemic may be preceded by a sharp fall in the burden of hemorrhagic strokes. The recent decline in CVD mortality reported from South Korea reflects such a fall in the contribution from hemorrhagic strokes, while thromobotic stroke and coronary heart disease burdens have just begun to rise.30 The model of “health transition”, while very useful, is not immutable and is likely to vary according to both levels of development and the nature of public health responses to social transition.
The model of health transition should also not lead to complacency regarding the high absolute burdens and early deaths in the developing countries. For example, even in a country in “early transition” like Tanzania, the stroke mortality rates in the age group of 15–59 years in rural and urban areas are 2 – 4 times higher than those in UK, in a similar age group.31
Early and late adopters
The pace of epidemiologic transition will vary both among countries and within countries. Usually lifestyle changes towards risk-prone behaviors occur first in the higher socio-economic groups and urban communities for whom the innovations of modernity are more easily accessible and affordable. As these innovations diffuse and become routinely available at prices amenable to mass consumption, the poorer sections and rural communities also join the CVD bandwagon. Soon the awareness of CVD risks as well as the economic independence to make healthy lifestyle choices in relation to diet and leisure time exercise (along with the greater ability to access healthcare) moves the “early adopters” in the affluent and urban strata into a reduced risk zone. The burden of CVD then is largely concentrated in the lower socio-economic groups and rural populations who continue to practice high-risk behaviors and display elevated risk factor levels.24 These “late adopter” groups also will slowly alter their behaviors, lower their levels of risk and reduce their burden of CVD, as healthcare responses to the CVD epidemic become universally effective. The progressive reversal of CVD risk factors with increasing levels of urbanization is now evident in India.32
This is the evolutionary profile of the CVD epidemic, as evident from the analysis of mature epidemics in industrial nations and the advancing epidemics in the developing countries. Differences within countries and between countries, suggested by cross-sectional views at any point in this evolution, should not obscure the longitudinal perspective of an evolving epidemic in which most countries will traverse similar paths, albeit at different times determined by their pace of development. Global shifts in CVD risk factors and their reflection in global CVD trends indicate that all countries and communities have far more in common in terms of disease causation than the differences which demarcate them. The challenge of epidemiologic transition is not whether it will happen in the developing countries, but whether we can apply the available knowledge to telescope the transition and abbreviate phase three of the model in these countries.
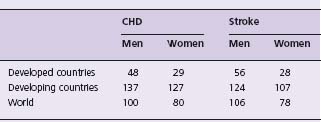
The Global Burden of Diseases study estimates that annual mortality from non-communicable diseases will rise from an estimated 28.1 million deaths in 1990 to 49.7 million in 2020.7 CVD, which accounts for a large proportion of these, will rise as a result of the accelerating epidemic in the developing countries. CHD will continue to be the leading cause of death in the world and, in terms of DALY lost, will rise from its fifth position in 1990 to top the DALY table in 2020.7 Men as well as women in the developing countries will experience the largest rise in CHD and stroke mortality rates across the world (Table 8.1).
The profile of DALY loss attributable to CVD in 1990 in various regions of the world and the projected estimates for 2020 (Table 8.2) also indicate a large rise.4 Among the developed countries, the sharp decline in the industrial nations is partly offset by the rise in the former socialist countries.
Table 8.2 Contribution of cardiovascular disease to DALY loss (percentage of total)
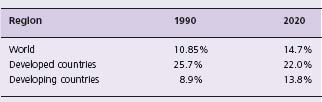
Adapted from Murray and Lopez.4
Deaths attributable to tobacco, a risk factor for CVD and other chronic diseases, are projected to rise from 3.0 million in 1990 to 8.4 million in 2020. The largest increases will be in India, China and other developing countries in Asia, where tobacco-attributable deaths will rise from 1.1 million to 4.2 million in 2020.33
These projections have been updated on the basis of substantial improvements in data availability and methods for dealing with incomplete and biased data (Table 8.3). According to the revised model, age-specific death rates for most chronic diseases are projected to decrease slightly at rates of around 0.5 – 1.0% per year in low-and middle-income countries. This is with the exceptions of lung cancer and chronic obstructive pulmonary disease (which are increasing because of the tobacco epidemic) and diabetes mellitus (which is increasing because of projected increases in the prevalence of overweight and obesity). Adverse trends for some risk factors like overweight and physical inactivity were probably more than offset in the selected countries by improved control of other risk factors like high blood pressure, high blood cholesterol and tobacco smoking and improved access to effective treatment interventions. Total deaths from cardiovascular diseases and diabetes are projected to rise to 14.3 million in 2015 and 17.3 million in 2030 in 23 selected low-and middle-income countries.19 Just under half of these deaths will occur in people younger than 70 years compared to 27% in high-income countries.
Table 8.3 Millions of projected deaths and DALY s for all chronic diseases as a proportion of deaths and DALY s for all causes in 23 selected low-and middle-income countries for 2005, 2010 and 2030
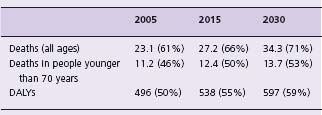
Adapted from Abegunde et al.19
Mechanisms which propel a cardiovascular disease epidemic in developing countries
Demographic changes due to the epidemiologic transition
A major public health challenge, identified by recent analyses of global health trends, is the projected rise in both proportional and absolute CVD mortality rates in the developing countries over the next quarter century. The reasons for this anticipated acceleration of the epidemic are many.5 In the second half of the 20th century, most developing countries experienced a major surge in life expectancy. This was principally as a result of a decline in deaths occurring in infancy, childhood and adolescence and was related to more effective public health responses to perinatal, infectious and nutritional deficiency disorders and to improved economic indicators like per capita income and social indicators like female literacy in some areas. These demographic shifts have augmented the ranks of middle-aged and older adults. The increasing longevity provides longer periods of exposure to the risk factors of CVD, resulting in greater probability of clinically manifest CVD events. The concomitant decline of infectious and nutritional disorders (competing causes of death) further enhances the proportional burden due to CVD and other chronic lifestyle-related diseases.
The ratio of deaths due to pre-transitional diseases (related to infections and malnutrition) to those caused by post-transitional diseases (like CVD and cancer) varies among regions and between countries, depending on factors like the level of economic development and literacy as well as availability and access to healthcare. The direction of change towards a rising relative contribution of post-transitional diseases is, however, common to and consistent among the developing countries.34 The experience of urban China, where the proportion of CVD deaths rose from 12.1% in 1957 to 35.8% in 1990, illustrates this phenomenon.35
Population expansion and aging
The aging of all populations heightens the importance of CVD both in people of working age and in those who are beyond working age. The world population is expected to rise from 5.71 billion in 1995 to 8.29 billion in 2025. By 2020, the median age of the population in much of the developing world will begin to approach that of the West. By 2040, the total number of people more than 65 years old in more developed countries will be only one-third of the number in less developed countries.20
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree