The continuous measurement of sustained atrial tachyarrhythmia (AT) is now possible with some permanently implanted devices. Data on this subject remain controversial. The aim of this study was to evaluate the incidence of sustained AT in patients treated with cardiac resynchronization therapy using pacemakers without backup defibrillators (CRT-P), within the first year after implantation, using strict definition criteria for sustained AT and a systematic review of all high-quality electrographically recorded episodes. The Mona Lisa study was a prospective, multicenter, cohort study carried out from February 2004 to February 2006, with a 12-month follow-up period. Sustained AT was defined as an episode lasting ≥5 minutes; episodes were confirmed by a systematic review of electrograms in the whole study population. Of the 198 patients who underwent CRT-P device implantation and were enrolled in the study, 173 were in stable sinus rhythm at baseline and were included in the analysis (mean age 70 ± 9 years, 66% men, 91% in New York Heart Association class III, mean QRS duration 164 ± 26 ms, mean left ventricular ejection fraction 25 ± 7%). During a mean follow-up period of 9.9 ± 3.6 months, 34 patients experienced ≥1 episode of sustained AT, for an incidence rate of 27.5% (95% confidence interval 18.2 to 36.7). Only a history of AT was independently associated with the occurrence of sustained AT within the 12 months after CRT-P device implantation (hazard ratio 2.3, 95% confidence interval 1.2 to 4.4, p = 0.02). In conclusion, this first prospective electrogram-based evaluation of AT incidence demonstrated that 27% of patients developed ≥1 episode of sustained AT lasting ≥5 minutes in the 12 months after CRT-P device implantation.
Atrial tachyarrhythmia (AT) (mostly fibrillation or flutter) is a common finding in patients with heart failure and is known to be associated with increased risk for morbidity and mortality. Until recently, the incidence of AT was evaluated using ambulatory electrographic recordings. The continuous measurement of such events is now possible with some permanently implanted devices using different methodologies, such as event markers or endocavitary electrographic Holter memories. When based on high-quality electrographic recordings, these devices enable the accurate quantification of AT burden. This feature is of particular interest in heart failure patients implanted with cardiac resynchronization devices. However, data on this subject are controversial for 2 main reasons. First, there is poor consensus on the definition of “sustained” AT, mainly in terms of duration. Second, it was difficult to accurately assess AT with previous generations of implanted devices that did not offer the possibility of high-quality electrographic recordings. Consequently, reliable AT burden within 1 year after resynchronization is still unclear. In the present prospective study, we investigated the “true” or “reliable” incidence of sustained AT in patients treated with cardiac resynchronization therapy (CRT) using pacemakers without backup defibrillators (CRT-P), within the first year after implantation, using strict definition criteria for sustained AT and a systematic review of all high-quality electrographically recorded episodes.
Methods
The study population and methods of the Mona Lisa cohort study have been described in detail previously, as well as in a subanalysis aiming to evaluate heart rate variability in this population. Briefly, the Mona Lisa study was a prospective, multicenter, cohort study ( ClinicalTrials.gov identifier NCT00180531 ) carried out from February 2004 to February 2006, designed to determine the incidence of arrhythmias and their prognostic impact in CRT-P device recipients within 1 year after implantation (until February 2007). Patients who underwent transvenous CRT-P (Contak Renewal TR2; Guidant Corporation, St. Paul, Minnesota) were enrolled at 24 centers and followed for 12 months. All enrolled patients provided informed consent for a specific follow-up plan.
All patients were aged >18 years, with the following criteria for CRT-P device implantation according to current guidelines when the study was designed : New York Heart Association functional class III or IV, QRS duration ≥120 ms, left ventricular ejection fraction ≤40%, and receiving optimal medical therapy. In addition, intra- and/or interventricular dyssynchrony was confirmed by echocardiography or tissue Doppler imaging in all patients. Exclusion criteria included conventional recommendations for treatment with a CRT-D device upon inclusion, patients in whom transplantation was anticipated as preferable, unexplained syncope, myocardial infarction <60 days before inclusion, suboptimal pharmacologic treatment, any coronary disease that might be treated by revascularization, and estimated life expectancy <6 months in patients with concomitant pathology. In addition, in this analysis, only sinus rhythm patients at inclusion were considered.
Patients underwent the implantation of CRT-P devices using commercially available leads for right atrial and ventricular pacing. A left ventricular lead was placed through a guiding sheath into a distal branch of the coronary sinus vein. Atrioventricular delay was programmed to obtain complete capture of both ventricles. CRT-P device optimization by echocardiography (atrioventricular and ventriculoventricular delays) was left to the physicians’ discretion.
The baseline clinical characteristics, including the results of noninvasive and invasive cardiac evaluations, as well as implantation data, were stored prospectively in the Mona Lisa database. Patients were then followed up at 3, 6, and 12 months after implantation. The devices were interrogated at each session, and the complete set of data was recorded on a floppy disk, printed out, and used to retrieve sustained AT episodes.
The Contak Renewal TR2 is a CRT-P device offering high-quality atrial electrographic recording capabilities; it allows the diagnosis of sustained AT ( Figure 1 ). The prevalence of sustained AT was based only on stored intracardiac electrograms, not on markers or counters that could be mismatched by artifacts. A systematic review of all stored electrograms was performed by an independent events committee that was unaware of the patients’ histories.
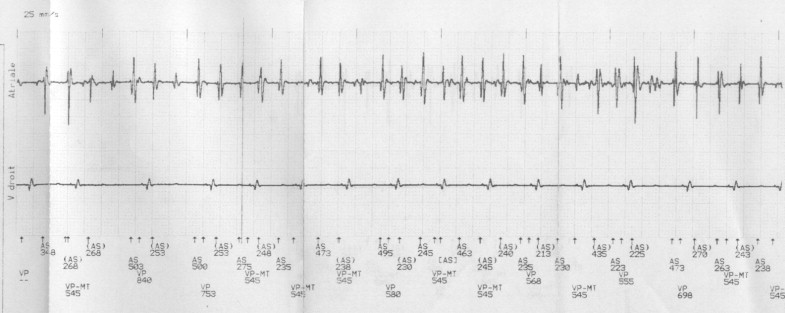
Capture of electrograms was triggered by a minimal programmed number of atrial cycles at a minimal programmed cycle length. Devices were programmed identically in all patients to facilitate the detection of sustained AT as follows: (1) bipolar and optimized atrial sensing; (2) spontaneous atrial rate >160 beats/min (cycle length <375 ms); and (3) number of cycles >512, corresponding to a sustained AT episode duration of approximately 5 minutes. This point was also crucial so as not to saturate the device’s Holter memory and to register only clinically relevant episodes of AT that could lead to specific treatments.
Categorical variables are presented as percentages and continuous variables as mean ± SD as appropriate. A p value <0.05 was considered statistically significant, and 95% confidence intervals (CIs) were calculated. Incidence rates were estimated for sustained AT. Predictive analysis for the risk for a sustained AT event was based on Cox proportional-hazard models and was quantified by hazard ratios (HRs). The following covariates were considered: age (≥72 vs <72 years); gender (male vs female); functional status (New York Heart Association class IV vs III); underlying heart disease (coronary artery disease or dilated cardiomyopathy); history of AT before CRT-P device implantation; left ventricular ejection fraction (≥30% vs <30%); variation in QRS duration after CRT-P (≥40 vs <40 ms); and β-blocker, angiotensin-converting enzyme and/or angiotensin II-receptor blocker, and amiodarone use. HRs of sustained AT events associated with these covariates were first estimated in univariate models. Covariates with p values <0.20 in the univariate analysis were included in a multivariate model with backward stepwise selection. All data were analyzed using SAS version 8.2 (SAS Institute Inc., Cary, North Carolina).
Results
From February 2004 to February 2006, 198 patients underwent CRT-P device implantation and were enrolled in the Mona Lisa study. Of these patients, 173 were in stable sinus rhythm and were included in the present analysis. Among them, 56 (32.4%) had histories of AT. The mean follow-up period was 9.9 ± 3.6 months (median 11.5 months, interquartile range 10.1 to 12.0). The baseline characteristics of the overall population are listed in Table 1 .
| Characteristics | Value |
|---|---|
| Age (years) | 71 ± 9 |
| Weight (kg) | 75 ± 15 |
| Men | 113 (65%) |
| NYHA functional class | |
| III | 157 (91%) |
| IV | 16 (9%) |
| Mean NYHA functional class | 3.1 ± 0.3 |
| Cause of heart failure | |
| Coronary artery disease | 72 (42%) |
| Dilated cardiomyopathy | 84 (49%) |
| Other | 17 (9%) |
| QRS duration (ms) | 164 ± 26 |
| Left ventricle ejection fraction (%) | 25 ± 7 |
| Left ventricle end-diastolic diameter (mm) | 66 ± 11 |
| Left auricular diameter (mm) | 47 ± 8 |
| Asynchrony on echocardiography | |
| Interventricular delay (ms) | 70 ± 49 |
| Intra-left ventricle delay (ms) | 110 ± 61 |
| History of atrial tachyarrhythmia | 56 (32%) |
| Medical treatment | |
| β blockers | 119 (69%) |
| ACE inhibitors/ARBs | 158 (91%) |
| Furosemide | 164 (95%) |
| Aldactone | 100 (58%) |
| Digoxin | 46 (27%) |
| Amiodarone | 128 (74%) |
During the follow-up period, a total of 75 events were detected in 34 patients who experienced ≥1 episode of sustained AT lasting ≥5 minutes (range 1 to 6), for an incidence rate for a first event of about 27.5% (95% CI 18.2% to 36.7%) (the distribution of AT occurrence over time is shown in Figure 2 ). In 31 patients, the mean duration of sustained AT episodes was 3.8 ± 3.7 hours (range 0.1 to 10) per patient during this period, whereas in 3 others, long-standing AT was reduced by electrical external cardioversion. Most of these 75 events (84.0%) were asymptomatic or had few symptoms, whereas 16.0% of patients presented with significant symptoms (dyspnea, palpitations, dizziness), leading to 5 hospitalizations, including 3 for cardioversion.
Cox analysis showed that angiotensin-converting enzyme and/or angiotensin II receptor blocker use appeared to be associated with fewer episodes of sustained AT (HR 0.45, 95% CI 0.2 to 1.2, p = 0.10), even if this association did not reach statistical significance. History of sustained AT was the only significant predictor of occurrence of sustained AT (HR 2.3, 95% CI 1.2 to 4.5, p = 0.01) and remained significant (p = 0.02) in multivariate analysis ( Table 2 ).
| Variable | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| HR | 95% CI | p Value | p Value | |
| Age ≥72 vs <72 years | 1.19 | 0.60–2.36 | 0.62 | |
| Men vs women | 1.66 | 0.75–3.69 | 0.21 | |
| NYHA class IV vs class III | 1.58 | 0.55–4.48 | 0.39 | |
| Coronary artery disease vs non–coronary artery disease | 0.68 | 0.34–1.38 | 0.28 | |
| Dilated cardiomyopathy vs non–dilated cardiomyopathy | 1.34 | 0.69–2.63 | 0.40 | |
| Ejection fraction ≥30% vs <30% | 0.67 | 0.29–1.55 | 0.84 | |
| History of AT vs others | 2.27 | 1.16–4.45 | 0.01 ⁎ | 0.02 |
| ΔQRS duration † | 1.07 | 0.53–2.13 | 0.86 | |
| β-blockers | 0.75 | 0.37–1.52 | 0.43 | |
| ACE inhibitors/ARBs | 0.45 | 0.17–1.16 | 0.10 ⁎ | NS |
| Amiodarone | 1.38 | 0.68–2.78 | 0.37 | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


