Moderate functional mitral regurgitation (MR) in patients with aortic valve stenosis (AS) is often left unaddressed at the time of aortic valve replacement (AVR) because it is expected to decrease after AVR. However, some patients have persistent moderate MR after AVR. We sought to determine the preoperative echocardiographic predictor for persistent functional MR after AVR in patients with AS. Pre- and postoperative echocardiograms were reviewed in 110 patients with severe AS and functional MR who underwent AVR without mitral valve (MV) surgery. Fifty-eight patients received concomitant coronary artery bypass graft surgery. In patients with MV tenting, defined as apical displacement of mitral leaflets in the apical 4-chamber view, MV tenting area and tenting height were measured at midsystole. Eighty patients had MV tenting (mean MV tenting area 1.4 ± 0.5 cm 2 , mean MV tenting height 0.8 ± 0.2 cm) and 30 did not have it before AVR. MR severity decreased in 51 of 80 patients (64%) with MV tenting after AVR and in 25 of 30 patients (83%) without MV tenting (p <0.05). In patients with MV tenting, multivariate analysis revealed that presence of long-term atrial fibrillation and MV tenting area were independent predictors of postoperative MR severity (all p values <0.05). The sensitivity and specificity in predicting persistent moderate MR after AVR were 72% and 82% for MV tenting area >1.4 cm 2 . In conclusion, preoperative MV tenting predicts persistent functional MR after AVR in patients with severe AS.
Moderate mitral regurgitation (MR) in patients with aortic valve stenosis (AS) is often not corrected at the time of aortic valve replacement (AVR) because concomitant MR is expected to decrease after AVR, and simultaneous replacement of aortic and mitral valves significantly increases morbidity and mortality. However, we sometimes encounter patients who have persistent moderate MR even after AVR. Recent studies have demonstrated that more than moderate MR at the time of AVR could influence the long-term outcome in patients with AS. Therefore, if concomitant MR would not decrease after AVR, we may consider mitral valve (MV) surgery at the time of AVR. The cause of concomitant MR at the time of AVR was a significant predictive factor for improvement of MR after surgery. In most patients with organic MR such as those with myxomatous or rheumatic mitral valves, concomitant MR would likely not decrease after AVR, whereas patients with functional MR with no morphologic abnormalities of mitral apparatus show more frequent decrease of MR after surgery. However, even functional MR could persist after AVR in some patients. The ability to predict persistent functional MR after AVR would be of great clinical value. However, previous studies on this matter did not examine large numbers of patients with functional MR or show enough echocardiographic parameter data for functional MR. Therefore, this study examined whether persistence of functional MR after AVR could be predicted by preoperative echocardiographic parameters.
Methods
The study population consisted of 3,124 consecutive patients who underwent AVR from January 2002 to June 2006 at the Cleveland Clinic (Cleveland, Ohio). We selected patients who met the following inclusion criteria: (1) severe AS (aortic valve area ≤1.0 cm 2 ), (2) equal to or greater than moderate functional MR (grade ≥2+), (3) patients who underwent a first AVR with/without coronary artery bypass grafting, and (4) patients for whom pre- and postoperative echocardiographic images were available for review. Functional MR was defined as MR without morphologic abnormalities of mitral apparatus such as valve prolapse, significant calcification of leaflet or annulus, or ruptured chorda. We excluded patients who underwent concomitant MV repair or replacement at the time of AVR. All patients with severe functional MR (grade 4+) underwent concomitant MV surgery. Thus, they were excluded from this study. We initially examined data from 145 patients extracted from surgical and echocardiographic databases approved by the institutional review board for clinical research in our institution. Subsequently, patients with significant aortic insufficiency (grade ≥2+, n = 18), pacing rhythm (n = 5), or inadequate echocardiographic image quality (n = 12) were excluded. A total of 110 patients met the eligibility criteria. Patient clinical characteristics and preoperative echocardiographic data are listed in Table 1 . Patients with coronary artery disease were defined as those with known previous myocardial infarction and/or concomitant coronary artery bypass graft at the time of AVR. All patients had 2-dimensional echocardiographic examinations before and after (5 ± 3 days) AVR.
| All Patients (n = 110) | Tenting Group (n = 80) | No-Tenting Group (n = 30) | p Value (tenting vs no-tenting group) | |
|---|---|---|---|---|
| Variable | ||||
| Age (years) | 73 ± 10 | 73 ± 11 | 73 ± 7 | 0.5 |
| Men | 65 (59%) | 53 (66%) | 12 (40%) | 0.01 |
| Coronary artery disease | 60 (55%) | 50 (63%) | 10 (33%) | 0.006 |
| Long-term atrial fibrillation | 13 (12%) | 10 (13%) | 3 (10%) | 0.7 |
| Preoperative echocardiographic parameters | ||||
| Left ventricular end-diastolic volume (ml) | 136 ± 51 | 149 ± 50 | 102 ± 33 | <0.001 |
| Left ventricular end-systolic volume (ml) | 85 ± 49 | 99 ± 49 | 47 ± 26 | <0.001 |
| Left ventricular ejection fraction (%) | 41 ± 15 | 36 ± 14 | 55 ± 10 | <0.001 |
| Left ventricular mass (g) | 285 ± 97 | 312 ± 94 | 222 ± 73 | <0.001 |
| Left atrial area (cm 2 ) | 25 ± 6 | 27 ± 5 | 24 ± 6 | 0.006 |
| Mean transaortic valve gradients (mm Hg) | 43 ± 18 | 42 ± 18 | 47 ± 18 | 0.2 |
| Aortic valve area (cm 2 ) | 0.67 ± 0.17 | 0.67 ± 0.18 | 0.65 ± 0.15 | 0.5 |
| Mitral regurgitation jet area (cm 2 ) | 8.1 ± 2.7 | 8.6 ± 2.7 | 6.7 + 2.2 | 0.001 |
| E velocity (cm/s) | 96 ± 24 | 99 ± 24 | 88 ± 22 | 0.03 |
| A velocity (cm/s) | 86 ± 29 | 84 ± 30 | 88 ± 29 | 0.6 |
| E/A rate | 1.3 ± 0.7 | 1.4 ± 0.7 | 1.1 ± 0.6 | 0.08 |
| Deceleration time (ms) | 200 ± 91 | 187 ± 84 | 231 ± 105 | 0.03 |
| Postoperative functional mitral regurgitation | ||||
| Mitral regurgitation after aortic valve replacement <2+ | 76 (69%) | 51 (64%) | 25 (83%) | 0.03 |
| Mitral regurgitation jet area (cm 2 ) | 4.8 ± 2.9 | 4.8 ± 3.1 | 4.6 ± 2.5 | 0.2 |
Of 110 patients, 52 patients had isolated AVR and 58 had AVR with concomitant coronary artery bypass graft. AVR was performed with a bioprosthetic valve in 107 patients (Carpentier-Edwards, Edwards Life sciences, Irvine, California, in 105; 3F, ATS Medical, Inc., Minneapolis, Minnesota, in 1; and Mosaic, Medtronic, Inc., St. Paul, Minnesota, in 1), a mechanical valve in 2 patients (St. Jude Medical, St. Jude Medical, Inc., St. Paul, Minnesota, in 1; and Carbomedics, Inc., Austin, Texas, in 1), and a homograft in 1 patient. Average prosthetic valve size was 23 ± 2 mm (range 19 to 29). The concomitant aortic root enlargement procedure was performed in 14 patients (13%). In 58 patients with concomitant coronary artery bypass graft, 14 patients had 1 graft bypass surgery, 14 had 2 grafts, 16 had 3 grafts, and 14 had >4 grafts.
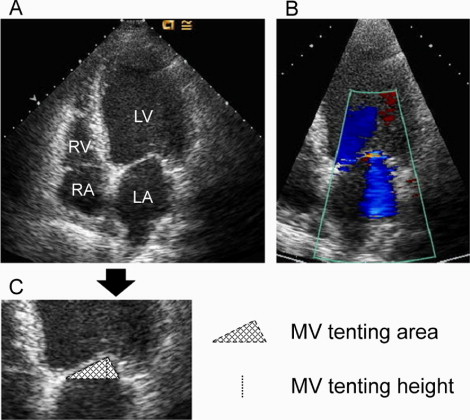
Two-dimensional comprehensive transthoracic echocardiography was performed using several commercially available echocardiographic systems. Left ventricular end-diastolic and end-systolic volumes and ejection fraction were calculated by the modified Simpson disk method. Left ventricular mass index was calculated by the area–length method. Left atrial area was measured from the apical 4-chamber view at end-systole. Mean transaortic valve gradient was calculated with the simplified Bernoulli equation. Aortic valve area was calculated by the continuity equation. For quantitative evaluation of MR severity, MR jet area on color flow mapping was measured by planimetry. Equal to or greater than moderate MR was defined as an MR jet area ≥4 cm 2 (grade ≥2+). We measured mitral annular area, which was estimated by the product of annular diameters in the apical 4-chamber and 2-chamber views. In patients with MV tenting, defined as apical displacement of mitral leaflets in the apical 4-chamber view, we measured the tenting height and tenting area of the MV. Tenting height of the MV was defined as the minimal distance between the leaflet coaptation and the mitral annular plane, and tenting area of the MV was defined as the area enclosed by the annular plane and 2 leaflets in the 4-chamber view at the time of maximal MV closure in midsystole as previously reported ( Figure 1 ). From transmitral inflow velocities, the following variables were measured: peak velocity of early diastolic filling (E velocity), late filling with atrial contraction (A velocity), E/A ratio, and deceleration time of the E wave. In patients with atrial fibrillation, only E velocity and deceleration time were evaluated. E velocity and deceleration time were measured 3 times and the average of these measurements was calculated in each patient with atrial fibrillation.
Data are expressed as mean ± SD, frequency distribution, or simple percentage. An unpaired t test or chi-square analysis was used to compare continuous variables or proportions between 2 different groups. Paired t test was used to compare pre- and postoperative measurements. We used linear regression for correlation of variables of interest. Multivariate stepwise regression analysis was performed to identify factors associated with postoperative MR jet area. Significant variables for univariate analysis were entered into the models. Differences were considered statistically significant at a p value <0.05 (2-sided). We also examined the sensitivity and specificity of various cut-off points for predicting persistent MR grade ≥2+ after AVR using receiver operating characteristic curves. Calculations were done using commercially available statistical software (SPSS 13.0, SPSS, Inc., Chicago, Illinois).
The authors had full access to the data and take full responsibility for their integrity. All authors have read and agree to the report as written.
Results
Eighty patients had MV tenting (73%, tenting group; mean MV tenting area 1.4 ± 0.5 cm 2 , mean MV tenting height 0.8 ± 0.2 cm) and 30 did not (27%, no-tenting group). Clinical and preoperative echocardiographic data of the 2 groups are listed in Table 1 . There were more men and patients with coronary artery disease in the tenting group than in the no-tenting group. Patients in the tenting group had significantly larger left ventricular volumes, left ventricular mass, and left atrial size, lower ejection fraction, and more severe MR than those in the no-tenting group. In transmitral inflow velocities, E velocity in the tenting group was significantly higher than that in the no-tenting group and deceleration time in the tenting group was significantly shorter than that in the no-tenting group. Functional MR in 51 of 80 patients (64%) improved to ≤1+ after AVR in tenting group and in 25 of 30 patients (83%) in the no-tenting group ( Table 1 ).
In 80 patients with MV tenting, postoperative MR jet area was significantly associated with long-term atrial fibrillation, preoperative left ventricular end-diastolic and end-systolic volumes, left ventricular ejection fraction, MR jet area, MV tenting area, tenting height, and mitral annular area in univariate analysis ( Figure 2 , Table 2 ). Multivariate stepwise regression analysis revealed that long-term atrial fibrillation and preoperative MV tenting area independently predicted postoperative MR jet area ( Table 2 ). In the MV tenting group, 51 patients (64%) showed decrease in MR after AVR (grade ≤1+). Twenty-nine patients (36%) showed persistent MR after AVR (grade ≥2+). Comparisons of clinical and echocardiographic data between patients in the tenting group with and without persistent MR after AVR are presented in Table 3 . Using receiver operating characteristic curves, we found that the sensitivity and specificity in predicting persistent MR after AVR were 72% and 82% for an MV tenting area >1.4 cm 2 (area under the curve 0.81; Figure 3 ).
| r | Univariate p Value | Multivariate p Value | |
|---|---|---|---|
| Variable | |||
| Age | −0.14 | 0.2 | |
| Male gender | −0.03 | 0.8 | |
| Coronary artery disease | −0.17 | 0.1 | |
| Long-term atrial fibrillation | 0.30 | 0.007 | 0.03 |
| Preoperative echocardiographic parameters | |||
| Left ventricular end-diastolic volume (ml) | 0.25 | 0.03 | 0.2 |
| Left ventricular end-systolic volume (ml) | 0.29 | 0.009 | 0.3 |
| Left ventricular ejection fraction (%) | −0.27 | 0.02 | 0.7 |
| Left ventricular mass (g) | 0.12 | 0.4 | |
| Left atrial area (cm 2 ) | 0.18 | 0.1 | |
| Mean transaortic valve gradients (mm Hg) | −0.20 | 0.08 | |
| Aortic valve area (cm 2 ) | 0.05 | 0.7 | |
| Mitral regurgitation jet area (cm 2 ) | 0.32 | 0.003 | 0.4 |
| E velocity (cm/s) | −0.05 | 0.7 | |
| A velocity (cm/s) | 0.16 | 0.2 | |
| E/A rate | −0.23 | 0.08 | |
| Deceleration time (ms) | −0.04 | 0.7 | |
| Mitral valve tenting area (cm 2 ) | 0.62 | <0.001 | <0.001 |
| Mitral valve tenting height (cm) | 0.53 | <0.001 | 0.6 |
| Mitral annular area (cm 2 ) | 0.35 | 0.002 | 0.3 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


