Exercise and Physical Activity
Eric H. Awtry
Gary J. Balady
Physical Activity And Public Health
Nearly 70 million (approximately 1 of every 4) persons in the United States have cardiovascular disease (CVD). Of these, 65 million suffer from hypertension, 13 million have coronary artery disease (CAD), 4.9 million have congestive heart failure, and 5.4 million have suffered a stroke (1). Despite the declining mortality rate from cardiovascular illness observed since 1950, 38% of all deaths in the United States are currently attributed to CVD. The morbidity and subsequent disability incurred from cardiovascular illness have far-reaching medical and socioeconomic implications, and accounted for an estimated total cost of $327 billion in 2000 (1).
Physical inactivity is a risk factor for the development of CVD (2) and is associated with a higher all-cause mortality rate (3,4). Conversely, regular exercise is associated with a lower incidence of cardiovascular symptoms and a reduction in cardiovascular mortality rates among asymptomatic persons (5,6) and patients with established CVD (7,8,9). Furthermore, a regular exercise program is a cost-effective intervention, with an estimated cost of less than $12,000 per year of life saved (10). Despite the clear benefits of physical activity, the proportion of Americans who are physically active is relatively small. The most recent report from the Centers for Disease Control and Prevention (CDC) indicates that only 25% of adult Americans engage in recommended levels of physical activity (11); 58% never participate in vigorous leisure-time activity (12), and 25% report no regular leisure time physical activity at all (13).
Many factors contribute to physical inactivity in adults; the most-cited reasons are a real or perceived risk of self-injury and lack of time. Other important barriers include physical limitations resulting from comorbid conditions, lack of companionship or encouragement, and the absence of an appropriate environment for exercise (e.g., no available paths for walking or biking, lack of exercise equipment, inclement weather, or unsafe neighborhoods). Although most Americans are aware of the health benefits of exercise, this awareness does not strongly correlate with engagement in physical activity. Rather, regular physical activity is more strongly associated with enjoyment of exercise, confidence in athletic ability, and participation in low to moderate levels of activity (14).
Physical Activity, Exercise, and Fitness
Physical activity, fitness, and exercise are related entities but have different definitions. The definitions described below are as defined in the Surgeon General’s report on physical activity and health (15).
Physical activity refers to skeletal muscle contraction resulting in bodily movement that requires energy use, and can be further classified based on the specific mechanical and metabolic aspects of contraction. Mechanically, physical activities can be divided into those that produce muscle tension without limb movement (isometric exercise) and those that produce limb movement without a change in muscle tension (isotonic exercise). Metabolically physical activity can be classified as aerobic (energy derived in the presence of oxygen) or anaerobic (energy derived in the absence of oxygen). Most activity involves a combination of these forms of muscle contraction (15). The intensity of physical activity can be described as the energy required per unit of time for the performance of the activity and can be expressed in units of oxygen use, kilocalories (measure of heat), or kilojoules (measure of energy). This energy requirement can be most readily quantified by measuring the oxygen uptake required during the activity. Alternatively, activity intensity can be expressed as a measure of the force of muscle contraction required (in pounds or kilograms). The intensity of a physical activity can be related in relative terms by expressing it as a proportion of the individual’s maximal capacity (e.g., the percentage of O2max or the percentage of
maximum heart rate) or as a multiple of resting metabolic requirements (i.e., the number of metabolic equivalents [METs] required to perform the activity) (15) (Tables 6.1 and 6.2).
maximum heart rate) or as a multiple of resting metabolic requirements (i.e., the number of metabolic equivalents [METs] required to perform the activity) (15) (Tables 6.1 and 6.2).
TABLE 6.1 Effort Intensity for Various Commonly Performed Exercise Activities | |||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||
Physical exercise is a form of physical activity that is planned and performed with the goal of achieving or preserving physical fitness. Exercise training may be a more accurate term, because similar activity may be viewed as exercise by one person and not by others (15). Physical fitness is a set of attributes that enables an individual to perform physical activity (14). Physical fitness is best assessed by measures of O2max, and is often estimated by measurement of the peak workrate or MET level achieved during graded exercise tests. Numerous exercise-training studies have evaluated the frequency, intensity, and duration of the training sessions required to achieve physical fitness. Based on these data, it appears that the most consistent benefit on O2max is observed when exercise training is performed at an intensity of approximately 60% of the maximum heart rate or 50% of O2max, for 20 to 60 minutes per session, for at least 3 to 5 sessions per week, for 12 or more weeks (16). Improvements in O2max of 15% to 30% are usually achieved using the above guidelines. It also appears that intermittent activity at comparable exercise intensity and total duration can confer fitness benefits similar to those of continuous activity (17).
TABLE 6.2 Classification of Physical Activity Intensitya | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
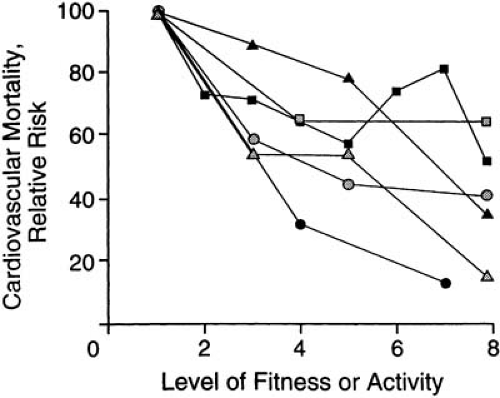 FIGURE 6.1. The relationship between physical activity or fitness and the relative risk for cardiovascular mortality. As fitness improves, the risk for cardiovascular death diminishes. ▪, Paffenbarger et al. (26); ▲, Morris et al. (1990); •, Blair et al. (2); □, Leon et al. (1987); [gray up-pointing triangle], Ekelund et al. (1988); [gray circle] Sandvik et al. (1993). (Source: From Pate RR, Pratt M, Blair SN, et al. Physical activity and public health: a recommendation from the CDC and the American College of Sports Medicine. JAMA 1995;273:402–407 , with permission.) |
Physical Activity and Health: Epidemiologic Observations and Biologic Mechanisms
Effects on All-Cause Mortality
Data accumulated over the past 50 years confirm the health benefits of exercise; epidemiologic studies show that active individuals have a lower risk of developing many chronic illnesses, including CVD (14), and that as many as 12% of deaths in the United States are associated with inactivity (18) (Fig. 6.1). In addition, physical activity is associated with lower all-cause mortality rates in healthy individuals (2,19,20), individuals with chronic diseases (4), diabetic persons (21), and the elderly (22,23). A large-scale epidemiologic study involving 13,375 women and 17,265 men between the ages of 20 and 93 years reported a significant inverse association between leisure time physical activity and all-cause mortality, with active individuals enjoying a 30% to 50% reduction in mortality compared with their sedentary counterparts (24). Importantly, an evaluation of 5,209 men and women demonstrated that the performance of recent activity confers a reduction in all-cause mortality, whereas activity performed decades earlier without subsequent maintenance appears to have no long-term benefit (25). Nonetheless, the risk for all-cause mortality decreases among inactive men and women who subsequently become more physically active (26,27).
Effects on Cardiovascular Events
Multiple studies have demonstrated the efficacy of regular exercise and physical activity in the primary and secondary prevention of cardiovascular events (2,6,20,23). In the Harvard University alumni study, men without a history of CVD were assessed for their activity level and followed for 16 years (20). There was a 39% reduction in cardiovascular morbidity and a 24% reduction in cardiovascular mortality in subjects with exercise energy expenditures of more than 2,000 kcal/week. Additionally, the risk of death became progressively lower as weekly energy expenditures from physical activity increased from 500 to 3,500 kcal. Furthermore, alumni who were initially inactive and later increased their activity levels demonstrated significantly reduced cardiovascular risk compared with those who remained inactive (26). A similar graded effect of exercise was noted in the Honolulu Heart Program, which studied the effects of walking on 2,678 physically capable men aged 71 to 93 years who did not have known CVD (6). Participants who walked less than 0.25 mile daily had a twofold increased risk of developing coronary heart disease (CHD) compared with those who walked more than 1.5 mile/day (5.1% versus 2.5%, P <0.1), whereas subjects who walked 0.5 to 1.5 mile daily had an intermediate risk (4.5%, P <0.5). In the Nurses’ Health Study of 73,029 women (aged 40 to 65 years), physical activity was inversely related to the risk of stroke and CAD (28,29). The largest benefit was seen between the lowest and second-lowest quintile groups for exercise, suggesting that the incremental value of exercise is greatest in the least-active subjects.
Exercise programs for patients with established CHD have been well studied (8,9,30,31,32). A meta-analysis of 48 randomizing trials encompassing 8,940 patients with CHD revealed that patients enrolled in cardiac rehabilitation programs had a 20% reduction in all-cause mortality and a 26% reduction in cardiac mortality, compared with subjects receiving usual care (9). Although individual trials have demonstrated a reduction in myocardial infarction (MI) in patients undergoing cardiac rehabilitation, there was no significant reduction in either MI or coronary revascularization noted in this meta-analysis. Among patients referred for or enrolled in cardiac rehabilitation programs, exercise capacity is a strong prognostic factor; incremental reductions in mortality risk are associated with progressively higher levels of fitness (31). Additionally, low exercise capacity predicts the need for future hospitalization (32). A recent meta-analysis regarding the use of exercise training in patients with heart failure has shown that exercise training in this population is safe, and is associated with a 35% reduction in mortality (8).
The specific mechanisms by which physical activity reduces CVD and CVD mortality have not been completely elucidated, but are likely multifactorial. In a cross-sectional analysis of a large cohort of men and women, higher levels of fitness were associated with lower levels of atherosclerotic risk factors in persons with and without CAD (33). However, modification of risk factors does not fully explain the benefits that have been observed. Other possible mechanisms—including effects on thrombosis, endothelial function, inflammation, and autonomic tone—may play an important role (Table 6.3).
TABLE 6.3 Physical Activity and Reduced Cardiovascular Risk: Biologic Mechanisms | |
|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


