Evaluation and Management of Fetal Heart Rate Patterns in Premature Gestation
The potential for the beneficial effects of fetal heart rate (FHR) monitoring in the patient delivering prematurely is perhaps greater than in any other risk group. Continued dramatic improvements in the neonatal survival rates at progressively earlier gestational ages increase the necessity for evaluating fetal well-being in early pregnancies and for intervention for fetal indications. Delivering prematurely is, of course, an abnormal event, and as opposed to normal labor and delivery in the term pregnancy, the various pathologic causes of premature delivery are often scenarios in which the likelihood of fetal hypoxia is increased. The premature fetus is more likely not only to be exposed to hypoxia but also to develop, and die from, the most common and serious complications of prematurity if born depressed and/or acidotic. FHR patterns in the premature fetus, both normal tracings and those indicative of hypoxia, differ from those at term. It therefore seems appropriate to emphasize the evaluation and management of fetal hypoxia separately in the premature fetus.
EFFECTS OF HYPOXIA IN THE PREMATURE FETUS
It is clear that neonatal care is the major contributor to the ongoing improvements in survival and decreasing permanent morbidities in premature babies. An impressive body of evidence indicates that the condition in which the premature newborn is delivered has an important impact on both its likelihood to survive and its odds of developing serious complications of prematurity.
Respiratory Distress Syndrome
In the early 1970s, when electronic FHR monitoring was initiated, Hobel et al. (1) and Martin et al. (2) showed that fetal hypoxia had an impact on the outcome of the premature newborn. Both investigations demonstrated that premature babies with low Apgar scores, abnormal FHR patterns in labor, or both had higher chances of developing respiratory distress syndrome (RDS), the most common serious complication of premature neonates, and had higher chances of dying of this complication. In the series of Martin et al., abnormal FHR patterns were more predictive of RDS development than were low Apgar scores. Subsequent research has confirmed these findings. Physiologically, this makes sense as those enzyme systems responsible for the production of surfactant, which keeps the term baby’s lungs open at birth, are very sensitive to acidosis in the preterm baby. Donald et al. (3) have shown that even those babies with amniotic fluid lecithin-to-sphingomyelin ratios that are indicative of fetal lung maturity may develop RDS if fetal hypoxia and/or acidosis precede delivery.
Intraventricular Hemorrhage
With improved outcomes in even smaller babies, and as the treatment of RDS has become more successful, intraventricular hemorrhage (IVH) has assumed greater importance in the morbidity of the very premature newborn. Initially, intracranial compression forces were thought to be causative, but as data have accumulated, it has become apparent that route of delivery, per se, has little to do with IVH (4,5 and 6). The most important risk factor for IVH is the degree of prematurity, with newborns in the range of 500 to 1,000 g being at highest risk. Ventilator therapy probably ranks next in importance due to the combination of RDS and patent ductus arteriosus in this very-low-birth-weight group (7,8). FHR patterns in labor indicative of hypoxia rank next. Babies with no RDS and normal Apgar scores at birth are less likely to develop the more severe degrees of IVH (grades 3 and 4), regardless of birth weight (8). Because fetal hypoxia and RDS are integrally related, it becomes apparent that the labor process is of critical importance in determining whether the very-low-birth-weight fetus will develop and possibly die of these two serious complications (IVH and RDS).
Necrotizing Enterocolitis
Necrotizing enterocolitis (NEC) is another important and potentially lethal complication in the premature infant. Although the cause is unknown, risk factors include infection, early feeding, umbilical arterial lines, exchange transfusion, and polycythemia (9). NEC is most likely to occur in premature infants with a history of perinatal asphyxia. The proposed mechanism is diversion of gastrointestinal blood flow to more critical organs with asphyxic conditions, resulting in ischemic injury to the bowel (9,10). In a review of FHR tracings of babies who developed NEC, Braly et al. (11) found that only 1 of 16 babies had a normal tracing, and 11 had severe FHR changes.
Death and Long-Term Injury
As one would expect, premature babies with hypoxia in labor and the above complications are more likely to die in the neonatal period (1,2,3,4,5,6,7,8,9,10,11,12,13,14 and 15). Furthermore, the abnormal FHR patterns in labor that are indicative of potential compromise have also been found to correlate with immediate and longterm neurologic sequelae. Westgren et al. (12,13) found that in premature fetuses abnormal FHR patterns to be more highly predictive of fetal acidosis and that in acidotic babies with abnormal FHR patterns, neurologic problems in the neonatal period were more frequent than those in premature controls. They also found a relationship between abnormal FHR, acidosis, and death from asphyxia in the first 2 years of life.
In general, the earlier in pregnancy that delivery occurs, the more profound the correlation between abnormal FHR patterns, neonatal depression and acidosis, and immediate and long-term complications. Most studies find these relationships to be most persistent and most profound in babies of <33 weeks’ gestation with birth weights of < 1,500 g (12,13,15). For complications such as severe IVH, earlier gestations, such as those of <28 weeks and with birth weights of < 1,000 g, are more important.
RELATIONSHIP BETWEEN CAUSE OF PREMATURE BIRTH AND FETAL COMPROMISE
Many of the causes of prematurity are also situations that increase the probability that the fetus will be subjected to antepartum and/or intrapartum hypoxia; thus, the premature baby not only is more likely to suffer complications if it becomes asphyxiated but also is more likely to be subjected to asphyxia. The implications for management relate to the reasons for this increased exposure as it pertains to the various causes.
Abruptio Placentae
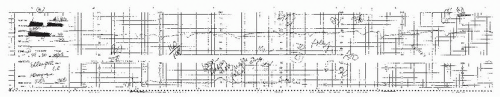
Abruption is an uncommon complication, occurring in only about 0.5% of term infants but in 5% to 10% of premature deliveries (16,17 and 18). Abruptio placentae increases hypoxic insults through two mechanisms. The separation of the placenta from the maternal decidual surface and thus the maternal blood supply, depending on degree, decreases placental surface area and thus oxygen exchange. In addition, there is often a marked increase in the frequency and, occasionally, duration of contractions, which prolongs the interval during which oxygen delivery to the intervillous space is interrupted. Because placental insufficiency is the mechanism of the fetal hypoxia, late decelerations will be the characteristic FHR pattern, and prolonged decelerations may occur in severe cases. One particular benefit of fetal monitoring is that patients sometimes present with preterm labor with minimal or no bleeding, and the contraction pattern and/or late decelerations are the earliest and only indication that abruptio placentae is the etiology of the premature labor (Fig. 10.1).
Preeclampsia
Preeclampsia is not an unusual cause of premature delivery resulting from associated premature labor, abruption, or induction of labor at an early gestational age because of the clinician’s concern over the severity of the disease. Often, the onset of preeclampsia at very early gestational ages is associated with intrauterine growth restriction (IUGR) and chronic placental insufficiency. In such cases, FHR patterns may exhibit late decelerations if there is insufficient placental perfusion (Fig. 10.2) and/or variable decelerations if there are growth restriction and oligohydramnios leading to umbilical cord compression (Fig. 10.3). Clinical decisions regarding delivery of a very premature infant in a setting of abnormal FHR patterns are complex and involve the integration of both maternal and fetal issues and prognoses.
Preterm Premature Rupture of Membranes
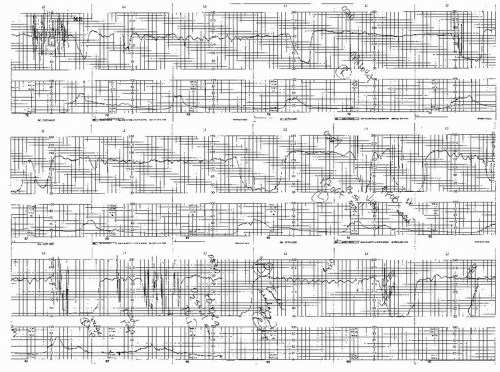
Preterm premature rupture of membranes (PPROM) is the most common single circumstance leading to premature delivery and accounts for approximately 35% of preterm deliveries. Patients with PPROM in preterm labor have a sevenfold greater risk of fetal compromise requiring cesarean section than patients with preterm labor with intact membranes (19). The vast majority of such patients have variable or recurrent prolonged decelerative patterns consistent with umbilical cord compression secondary to oligohydramnios (Figs. 10.4 and 10.5). Prophylactic use of amnioinfusion has been demonstrated to decrease the frequency and severity of such decelerations and increase the likelihood of allowing vaginal delivery in such patients (20).
Intrauterine Growth Restriction
IUGR may result in preterm delivery either because the problem that caused the growth restriction also leads to preterm labor, as in preeclampsia or thyrotoxicosis, or because the physician detecting the IUGR decides to intervene prematurely. In such cases, fetal hypoxia in labor is more likely due to the associated inadequate delivery or exchange of oxygen resulting in late decelerations or to the associated oligohydramnios leading to umbilical cord compression patterns (Fig. 10.6). Fetuses with IUGR are even more susceptible to damage from asphyxia than their premature counterparts of similar gestational ages.
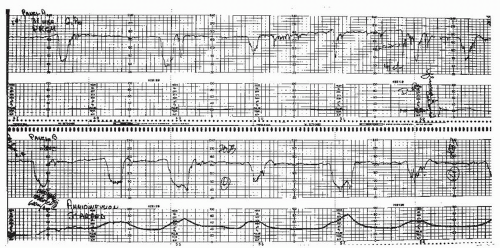 Figure 10.4. Typical variable decelerations seen in early labor (4-cm dilation) in a patient with premature rupture of membranes and oligohydramnios at 31 weeks. An attempt at amnioinfusion (seen on the lower panel) failed to relieve the cord compression, and the patient required cesarean section for a worsening pattern.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|