Estrogen, Female Gender, and Heart Disease
Pathmaja Paramsothy
Robert H. Knopp
Overview
Death from cardiovascular disease (CVD), meaning heart disease and stroke, is slightly more common in women than in men. CVD in women is a formidable problem because of difficulties in diagnosis and increased morbidity and mortality associated with CVD events at all ages. In the middle years, CVD is associated with multiple risk factors, generally more in women than in men of the same age. Among these, diabetes is a more severe risk factor in women than in men, raising CVD rates in women to those of men. Insulin resistance, obesity, and the metabolic syndrome also function in the same way. An example of this relationship is the greater risk of high triglyceride and low high-density lipoprotein (HDL) for CVD in women compared to men. In contrast, low-density lipoprotein (LDL) seems to be the more predominant CVD predictor in men. Smoking is also a very serious CVD risk factor in women. In the context of oral contraceptive use, smoking can multiply CVD risk many times. Postmenopausally, hormone replacement therapy (HRT) does not prevent CVD in women at mean ages of 64 and 67 years in two prospective trials. An increase in stroke incidence was observed in one of these trials. In contrast, estrogen may have CVD benefit if given before the development of advanced atherosclerosis, for instance at the time of menopause. On the other hand, women with advanced CVD at the time of menopause or combinations of risk factors may have increased risk from estrogen. Thus, complete risk factor assessment, including noninvasive vascular testing and careful clinical judgment are advisable in starting HRT at the time of menopause. The estrogen patch is an attractive modality of estrogen delivery, because it avoids the first-pass hepatic effect of oral estrogens on clotting factors. Potential distinctions among the vascular effects of the available progestins have not been ruled out.
Glossary
Combined hyperlipidemia
The combined elevations of triglycerides above 200 mg/dL and LDL-C levels above National Cholesterol Education Program (NCEP) targets: 70, 100, 130, or 160 mg/dL.
Cholesterol ester transport protein (CETP)
A protein that recycles cholesterol from HDL to LDL, thereby conserving the body’s cholesterol.
Lipoprotein(a) [Lp(a)]
A protein on LDL that inhibits fibrinolysis in arterial clots, enhances LDL trapping in the arterial wall, and is risk factor for premature CVD, particularly in women.
Polycystic ovary syndrome (PCOS)
A common manifestation of insulin resistance in young women, characterized by infertility, anovulation, hyperandrogenemia, irregular menses, and often obesity.
Remnant lipoprotein
An atherogenic particle, intermediate between very-low-density lipoprotein (VLDL) and LDL in size and metabolism having atherogenic potential.
Metabolic syndrome
A syndrome of insulin resistance in which at least three of the following five abnormalities are seen: abdominal obesity, hypertriglyceridemia, low HDL, hypertension, and increased fasting glucose.
The main points of this chapter are illustrated in the following true case. A 25-year-old woman who used oral contraceptives (OCs) and smoked one pack of cigarettes per day had vague chest pains for a year, initially diagnosed as anxiety and acid reflux. On July 4, 2000, she was seen at an emergency room (ER) for chest pain and sent away. Twelve hours later at the same ER, the possibility of a myocardial infarction (MI) was entertained as she went into shock. An emergency two-vessel angioplasty procedure was performed, saving the patient’s life. Several other angioplasties and three-vessel bypass surgery have been done since, complicated by bilateral iliac vessel stenosis. She is now somewhat intellectually impaired. In clinic, her cholesterol was 182 mg/dL, triglyceride was 175 mg/dL, and HDL cholesterol (HDL-C) was 24 mg/dL on 40 mg atorvastatin. Her lipoprotein (a) [Lp(a)] level was 30 mg/dL, the seventy-fifth percentile.
Important questions are raised by this case. Why did this patient have an MI? Why was the MI not recognized during the ER room visit? Is this case really rare? Is the presentation and risk profile unique to this case or to women in general? What is the approach to managing this patient’s lipid disorder? This chapter attempts to address these issues.
Incidence of Coronary Artery Disease in Women Versus Men
The perception persists that coronary artery disease (CAD) among women is uncommon, especially in the young, and that arteriosclerotic disease is less important overall. These perceptions are incorrect. CVD is an equal opportunity killer in men and women over their lifetimes. In Washington State, the incidence of CVD death was 42% in women and 39% in men in 1991 and 33% in women and 32% in men in 2003 (1,2). Nationwide, these numbers approach 50%. The slightly higher percentage of female cardiovascular deaths can be attributed to the greater longevity of women, age being an extremely powerful risk factor in its own right. Greater longevity allows female CVD mortality to “catch up” in old age, particularly with stroke, 9.4% in women versus 6.2% in men (2).
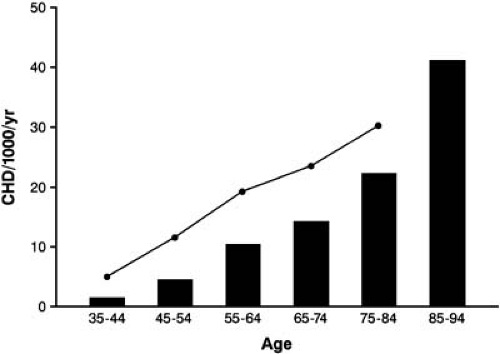
In youth, CVD rates are certainly lower in women than in men. However, the rate is not negligible and has defined relationships to cardiovascular risk factors. As shown in Figure 9.1, the increase in CVD with age in women in the Framingham study (3) is parallel to men but is delayed by 10 to 15 years. A similar delay in women is seen even in high-risk conditions such as heterozygous familial hypercholesterolemia. The delay in onset is attributed to the premenopausal exposure to endogenous ovarian estrogen, but is not immune to advancing age (Fig. 9.1). A slight increase in the female risk curve around the time of menopause may reflect the lack of estrogen (Fig. 9.1). Some women develop menopause early (especially smokers), and plasma estrogen levels decline in the 40s (a number of years before menopause), possibly contributing to an acceleration of atherogenesis prior to menopause.
The importance of CVD in young women can be appreciated by comparing CVD death rates in women to other causes of mortality. Since 1982, heart disease mortality has occurred at a rate of approximately 11 per 100,000 in women ages 25 to 45 years with little decline, reflecting the level rates for CVD in women overall in the last decade (4). The decline in Washington state since 1991 may be atypical (2). Among young women, approximately one third of heart disease deaths are coronary in etiology. In men ages 25 to 44 years, the CVD rate is approximately 30 per 100,000—almost 10 times more common than in women. As for other causes of mortality in women, cancer accounts for 29 per 100,000 and injuries for 14 per 100,000 (5). In a study of ER admissions among young persons (ages 18 to 45 years) for sudden death, 1 of 20 cases of coronary disease was in a young woman (6). In another study, one fourth of all MI survivors younger than 40 years at a major hospital were women (7). The main point is that CVD incidence in younger women is not negligible, ranging from one fourth to one twentieth the rate in men.
The early lesions of arteriosclerosis—fatty streaks and fibrous plaques—are seen in both young women and men. Half of the men and one fourth of the women in Bogalusa were so affected. Among blacks, men and women were affected equally. In both genders, the fatty streak lesions were proportional to the plasma LDL-C. However, the plasma very-low-density lipoprotein cholesterol (VLDL-C) level (8), was also associated with lesions, but only in women. When coronary lesions are examined, those in women are more lipid filled, rich in macrophages, and less densely fibrous (9). Thus, lesions in women could be more unstable under certain circumstances, as well as more readily reversed (10). Likewise, coronary calcification is
half that of men on ultrafast computed tomography until age 60 years, when the difference between the genders narrows (11).
half that of men on ultrafast computed tomography until age 60 years, when the difference between the genders narrows (11).
An excess of acute MI among young black women was observed in Bogalusa (8) and is confirmed nationally, where black women have a 50% to 75% greater risk of death from heart since 1950 (12) and into the 1990s (4). Age adjusted rates, per 100,000, were 190 for blacks and 110 for whites in 1988 (12). The reasons for this greater risk may reflect a greater CVD risk burden among African American women.
Differences in Cardiovascular Disease Presentation, Management, and Outcome In Women Versus Men
The tendency to overlook CVD in women is compounded by a less classical presentation, which is more frequently angina in women compared to MI in men. Among women participating in the Framingham study, the annual incidence of angina pectoris exceeded that of MI by more than 2:1 in the age range of 45 to 64 years. In contrast, frank MI exceeded angina in men of all age groups, ranging from 1.5:1 between ages 45 and 64 years to 6.5:1 between ages 75 and 84 years (13,14). In a recent study, women presenting for stenting had fewer MIs than men (15).
Recognition of cardiac chest pain is difficult in women because it is unexpected, often atypical, and more often noncardiac than in men. Misdiagnosis as chronic fatigue or a psychiatric disorder is not uncommon. The greater incidence of silent MI in women (14) may also be related to the atypicality of presentation. For example, one of our patients complained of early fatigability with exercise but had no ST changes on treadmill testing. Eventually, she developed overt angina and had bypass surgery whereupon the fatigue resolved. Anatomic studies might have been done earlier if her severe combined hyperlipidemia, elevated Lp(a), and impaired fasting glucose (see the section Lipid Screening Guidelines for Hyperlipidemic Women) had been appreciated.
This case also illustrates the point that exercise tolerance testing in women is more susceptible to false-positive and false-negative results than in men. If doubt persists after a negative exercise test, radionuclide or echocardiographic imaging may be ordered after exercise (16,17). Furthermore, a normal or negative angiogram does not necessarily mean that early atherosclerosis or endothelial dysfunction is not present, especially in women with risk factors.
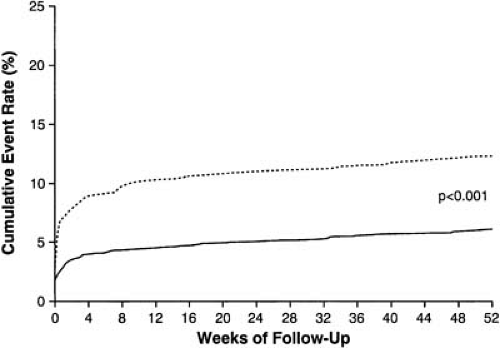
Frank MI in women has higher morbidity and mortality than in men. Sudden death is more frequent, and early post-MI mortality is greater in women than in men (18,19,20). Nearly all of the excess mortality in women is concentrated in the first 4 weeks post MI (Fig. 9.2). These data influence all subsequent statistics. After 1 year, a mortality rate of 32% in women versus 16% in men has been observed in the Framingham study (21,22). Thus, post-event, nonadjusted mortality is approximately 50% greater in women than in men for various intervals. These trends were confirmed recently and extended (23) with a higher risk for death relative to younger men (24).
Revascularization procedures including percutaneous intervention and bypass surgery also show greater short- and long-term morbidity and mortality in women than in men, although the probability of benefit remains high in both genders (25,26,27). Percutaneous interventions in women with coronary ischemia are associated with increased complications and decreased benefits (28,29). An analysis of stent experience from Germany found rates of death and MI greater in women at 30 days (3.1% versus 1.8% in men) but equal after 1 year (6.0 versus 5.8%) (15). Male–female differences in clinical presentation and prognosis are summarized in Table 9.1.
As to whether a frank bias exists in physician management of coronary disease and cardiac catheterization between the genders, two investigations indicate that less aggressive decision making is appropriate in women at low risk for cardiac death and little probability of benefit (30,31), or with angina pectoris (32). A recent study found more orders for do not resuscitate, less aspirin prescription, and less thrombolytic therapy in women compared to men with acute MI (33). The gender difference persists in the latest reports, especially in African American women. Specifically, reperfusion therapy was done post MI in 86.5% of white men, 83.3% of white women, 80.4% of black men, and 77.8% of black women (34). Ultimately, a woman’s care depends greatly on the interaction between patient and physician (35).
TABLE 9.1 Differences in CVD Presentation and Outcome in Women Versus Men | ||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||
The most important message from the greater morbidity and mortality associated with coronary disease in women is that high priority should be given to early recognition and treatment of risk factors and early ischemic symptoms in women. The other point is that obscure symptoms of fatigue or atypical chest pain should be worked up aggressively for potential coronary ischemia with exercise or vasodilator stress (when exercise is contraindicated) and myocardial perfusion imaging, particularly when risk factors for CAD are present and especially when present in combination.
Cardiovascular Disease Risk Factors in Women Compared to Men
Hypertension and smoking are risk factors for coronary disease in women as they are in men (13). Smoking was the worst of any single risk factor among male subjects (36), but seemed to have less impact among females. Nonetheless, in a study of 119,404 female nurses, the cardiovascular risk of smoking was clear (37) and appeared to be increasing in severity in recent birth cohorts (38). The interaction of smoking with OC use is also very strong (see the section Oral Contraceptive Use and Cardiovascular Disease Risk). Lp(a), fibrinogen, and homocysteine all function as risk factors in women, as well as in men (39,40,41). C-reactive protein (CRP), a marker of inflammation, is a strong and independent risk factor for CHD in women (41). Abdominal obesity, weight gain since age 18, and increments in body weight—even at body mass indexes less than 27—are associated with increased CVD incidence in women (42). Some of this association may be mediated by the strong CRP association with abdominal obesity (43). Two other risk factors in women are marital stress (44) and the initial days of the menstrual cycle (45).
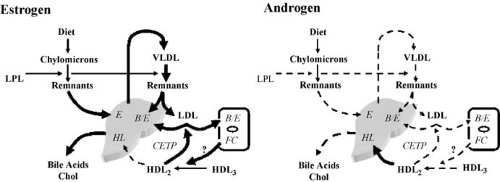
Diabetes, elevated triglyceride, and low HDL levels are stronger risk factors for CVD in women than men. Diabetes confers a greater increment of susceptibility to atherosclerosis in women than men, resulting in diabetic women having an absolute coronary disease rate equaling or approaching that of men (46,47,48). Diabetes may confer a greater mortality risk than having a prior MI (without diabetes) in women (48). The exaggerated diabetic effect on CVD in women is most marked in middle-aged women and attenuates with age, as does the cholesterol effect owing to the increased incidence of coronary disease from other causes, especially age (49). The greater impact of diabetes on CVD in women compared to men is due to more greatly disturbed lipoprotein levels in women compared to men (50,51,52), as well as the other classical CVD risk factors (51). Whether female gender exaggerates additional atherogenic mechanisms in diabetes such as lipoprotein oxidation and glycoxidation requires further study.
Total plasma cholesterol relates to heart disease risk differently in women than in men. The increment in CVD in men from a low- to a high-cholesterol level is nearly 10-fold in men aged 35 years but attenuates with increasing age to only 1.2-fold by age 65 years. In women aged 65 years, the increase in CVD risk associated with high cholesterol is twofold, but at an absolute increment similar to men: 2.4% versus 1.9%. This trend persists to old age, where LDL has stronger relative risk in women than men (53). Again, the decline in relative risk of cholesterol is because of the dilution of this effect by the increased rate of CVD with age.
The cluster of risk factors associated with CVD in middle age also differs between men and women. Because women tend to be protected compared to men and have a 10- to 15-year delay in the curve describing the rise in CVD (see Fig. 9.1), it follows that for a woman to have coronary disease in middle age, she must have more risk factors or a greater risk burden than a man to experience CAD, as seen in many studies (15,54).
The leading condition embodying multiple risk factors is the metabolic syndrome, arising from obesity and insulin resistance (55). The metabolic syndrome is defined as having three of five criteria, namely, abdominal obesity; elevated blood pressure, glucose; and triglycerides; and decreased HDL-C (56). The two lipid criteria define combined hyperlipidemia (57,58). Clotting factor abnormalities are also associated, including elevated factor VII and plasminogen activator inhibitor-1 levels as are markers of inflammation such as CRP and serum amyloid A (SAA), which is associated with a dysfunctional, “inflammatory HDL” (59). Thus, a single entity, the metabolic syndrome, may embody three to eight risk factors or more and cause premature CAD in middle aged women.
Coronary disease in middle-aged women is highly associated with the metabolic syndrome. Diabetes and hypertension are overrepresented three- and five-fold, respectively, in women with coronary disease compared to women without. In addition, diabetes, hypertension, and hyperlipidemia are present in more women than men with acute MI in virtually every study (15,18,19,20,25,30,35,60,61,62,63). In the recent WISE study, the metabolic syndrome predicted coronary disease, whereas obesity alone did not (64).
Plasma triglyceride and HDL abnormalities are stronger risk predictors for CAD in women compared to men. Triglyceride elevations are associated with a 1.8-fold increase in CVD risk in women compared to a 1.2-fold increase in risk in men (65). Similarly, a reduction in HDL-C is more strongly associated with CVD risk in women than in men. A 1 mg/dL drop in HDL-C is associated with a 3% to 4% increase in CAD in women compared to a 2% increment in coronary disease in men (66).
The importance of triglyceride and HDL to CVD in women is confirmed when coronary arteriosclerosis is graded according to angiographic severity. Elevated total cholesterol, LDL-C, and apoprotein B are most strongly associated with severity in men. In contrast, elevated VLDL-C, intermediate-density lipoprotein cholesterol, LDL triglyceride, and low apoprotein A-I levels are most strongly associated with severity in women (67). Again, lipid abnormalities of the metabolic syndrome predominate over LDL as CVD risk factors in women.
In women, an early manifestation of the metabolic syndrome is polycystic ovary syndrome (PCOS), with the features of hyperandrogenemia, irregular periods, and male pattern baldness. Such individuals typically have the lipid profile of combined hyperlipidemia. Conversely, women with CAD more frequently have a history of PCOS (68). Treatments include metformin 500 mg BID for the first week and 1 g BID thereafter, if tolerated (diarrhea) and thiazolidinediones (e.g., pioglitazone), 15 or 30 mg QD if tolerated (fluid and subcutaneous weight gain). Both reduce hyperandrogenemia and dysmenorrhea (69,70). Weight loss by modifying diet and regular aerobic exercise is also very important.
A further argument that combined hyperlipidemia in the metabolic syndrome is a major cause of premature coronary disease in middle-aged women is made from the distribution of arteriosclerosis in the vascular tree in women versus men (1,71). The increase in arterial surface area affected by arteriosclerosis occurs later in women than in men by approximately 10 years, as does the clinical onset of coronary disease (3), but the distribution of arteriosclerosis in women is greater in the aorta and less in the coronary circulation than in men. The more peripheral distribution of arteriosclerotic vascular disease is typical of patients with diabetes, high triglycerides, and low HDL—all features of the metabolic syndrome.
In summary, the metabolic syndrome and its associated combined hyperlipidemia are more prevalent in women with arteriosclerosis in middle age than in men. Management should
be directed toward the entire metabolic disorder (e.g., insulin resistance, obesity, hypertension, hyperglycemia, dyslipidemia) (72) and not toward a single factor such as elevated LDL, as important as it is. Important risk factors in women are listed in Table 9.2.
be directed toward the entire metabolic disorder (e.g., insulin resistance, obesity, hypertension, hyperglycemia, dyslipidemia) (72) and not toward a single factor such as elevated LDL, as important as it is. Important risk factors in women are listed in Table 9.2.
TABLE 9.2 Risk Factors for CVD in Women | ||
|---|---|---|
|
Dietary Response and Cardiovascular Disease
Controlled feeding studies indicate that LDL in women is approximately 30% less responsive to diet and cholesterol feeding than men, though this is not seen in free-living dietary interventions (73,74). More consistent are greater HDL-C decreases in women on low fat-diet—5% to 6% as compared to 1% to 3% in men after 6 and 12 months of diet—with the greatest reduction in HDL2-C, the estrogen-exercise–sensitive portion of HDL (74,75). Conversely, HDL is more sensitive to cholesterol and fat feeding in women.
There is no difference in dietary recommendation for men versus women in the current national guidelines (56). However, low-fat diets tend to raise triglycerides and lower HDL. Because these abnormalities are more important in women than in men, and higher fat intake lowers triglyceride levels (75,76




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree