Although the number of centenarians has been rapidly increasing in industrialized countries, no clinical studies evaluated their characteristics and outcomes from out-of-hospital cardiac arrests (OHCAs). This nationwide, population-based, observation of the whole population of Japan enrolled consecutive OHCA centenarians with resuscitation attempts before emergency medical service arrival from 2005 to 2013. The primary outcome measure was 1-month survival from OHCAs. The multivariate logistic regression model was used to assess factors associated with 1-month survival in this population. Among a total of 4,937 OHCA centenarians before emergency medical service arrival, the numbers of those with OHCAs increased from 70 in 2005 to 136 in 2013 in men and from 227 in 2005 to 587 in 2013 in women. Women accounted for 80.3%. Ventricular fibrillation (VF) as first documented rhythm was 2.5%. The proportions of victims receiving bystander cardiopulmonary resuscitation were 64.2%. The proportion of 1-month survival from OHCAs in centenarians was only 1.1%. In a multivariate analysis, age was not associated with 1-month survival from OHCAs (adjusted odds ratio [OR] for one increment of age 1.01; 95% confidence interval [CI] 0.87 to 1.18). Witness by a bystander (adjusted OR 3.45; 95% CI 1.88 to 6.31) and VF as first documented rhythm (adjusted OR 5.49; 95% CI 2.24 to 13.43) were significant positive predictors for 1-month survival. Cardiac origin was significantly poor in 1-month survival compared with noncardiac origin (adjusted OR 0.37; 95% CI 0.21 to 0.64). In conclusion, survival from OHCAs in centenarians was very poor, but witness by a bystander and VF as first documented rhythm were associated with improved survival.
Japan is one of the super-aging countries in the industrialized world, and the life expectancy for men and women there reached 80.5 years and 86.8 years in 2014, respectively. In accordance with the aging of the population, the proportion of out-of-hospital cardiac arrests (OHCAs) among the elderly population aged ≥65 years has also been increasing in recent years, and its continuous increase is an important public health problem. In preceding studies, researchers focused on OHCAs among elderly patients, but no studies assessed the epidemiology of OHCAs in centenarians. The population of centenarians has been rapidly increasing in industrialized countries; there were 44,449 centenarians in Japan and 53,364 in the United States in 2010, and their numbers in 2060 are expected to reach 637,000 in Japan and 604,000 in the United States. Therefore, the evaluation and understanding of characteristics and outcomes from OHCAs in centenarians are needed in the super-aging era. During the 9 years from 2005 to 2013, this registry collected approximately 5,000 OHCAs before emergency medical service (EMS) arrival in centenarians. Using this database, the present study aimed to evaluate the epidemiology of OHCAs in centenarians. Furthermore, we evaluated factors associated with 1-month survival from OHCAs in centenarians by multivariate analysis.
Methods
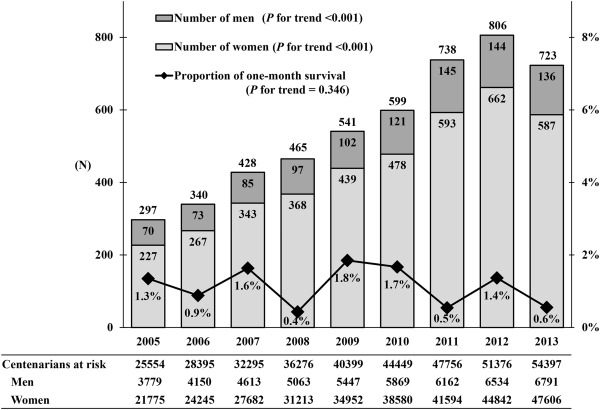
Based on the international standardized Utstein style, the Fire and Disaster Management Agency of Japan launched the All-Japan Utstein Registry, which is a nationwide, prospective, population-based OHCA registry, in January 2005. For our observation, we enrolled centenarians aged ≥100 years suffering from OHCAs before EMS arrival who were resuscitated by a bystander or EMS personnel and were then transported to medical hospitals from January 2005 to December 2013. In 2014, the elderly population aged ≥65 years was approximately 33,840,000, a proportion that accounted for 26.7% of the total population. During the study period, the population of centenarians increased from 25,554 (3,779 men and 21,775 women) in 2005 to 54,397 (6,791 men and 47,606 women) in 2013. The study protocol was approved by the medical institutional review board of Kyoto University and Osaka University. The requirement of attaining individual informed consent was waived in this registry.
Cardiac arrest was defined as the cessation of cardiac mechanical activity as confirmed by the absence of circulation signs. The arrest was presumed to be of cardiac origin unless it was caused by cerebrovascular diseases, respiratory diseases, malignant tumors, and external causes, such as drug overuse, drowning, suffocation, exsanguinations, trauma, or any other noncardiac origins. These diagnoses were made clinically by physicians in charge in collaboration with the EMS personnel. We previously described details of the Japanese EMS system. In Japan, there were 752 fire stations with emergency dispatch centers in 2014 that provided emergency services 24 h every day, and anyone is still free to use the free telephone emergency number 119 to call for an ambulance anywhere in Japan. Highly trained emergency care providers called emergency life-saving technicians (ELSTs), and each ambulance basically has a crew of 3 emergency providers including at least an ELST. The ELSTs are permitted to insert an intravenous line and an adjunct airway and to apply a semi-automated external defibrillator for patients with OHCAs. Specially trained ELSTs have been allowed to intubate since July 2004 and to administer intravenous epinephrine since April 2006. Automated external defibrillator (AED) use by citizens was legally approved in July 2004. All the EMS providers conduct cardiopulmonary resuscitation (CPR) according to the Japanese CPR guidelines. Importantly, do-not-resuscitate orders or living wills are not generally accepted in Japan. Furthermore, EMS providers are not allowed to terminate resuscitation in prehospital settings. All patients with OHCA treated by EMS personnel are, therefore, transported to a medical institution and basically registered in our registry, excluding victims with rigor mortis, decapitation, dependent cyanosis, incineration, or decomposition.
All data were prospectively gathered using a specific form that included core items recommended in the Utstein-style guidelines for OHCAs. These items included age, origin of OHCA, gender, witness status, first documented rhythm, type of bystander-initiated CPR, time course of resuscitation, public-access AED shocks, intravenous fluid, epinephrine, and endotracheal intubation and return of spontaneous circulation at prehospital settings, 1-month survival, and neurologic status 1 month after the OHCA occurrence. The EMS personnel first diagnosed documented rhythm recorded at the scene using semi-automated defibrillators. We regarded the first recorded rhythm as ventricular fibrillation (VF) when laypersons provided shocks using public-access AEDs.
The data were electrically recorded by the EMS personnel in co-operation with the physician in charge of an OHCA patient, transferred to and integrated into the OHCA registry system on the database server of the FDMA, and then checked logically by the system. Neurologic outcome 1 month after the occurrence was assessed by the physician responsible for the care of an OHCA patient, using the cerebral performance category (CPC) scale as follows: category 1, good cerebral performance; category 2, moderate cerebral disability; category 3, severe cerebral disability; category 4, coma or vegetative state; and category 5, death. The primary outcome measure was 1-month survival. Secondary outcome measures were prehospital return of spontaneous circulation and 1-month survival with neurologically favorable outcome, defined with CPC scale as 1 or 2.
Patient and EMS characteristics were expressed by the median (interquartile) for numerical variables and percentages for categorical variables. Poisson regression model was used for the trend in the number of OHCAs in centenarians, and univariable regression model was used for the trend in 1-month survival after OHCA were used. Multiple logistic regression models were used to assess prehospital factors associated with 1-month survival, and we calculated odds ratios (ORs) and their 95% confidence intervals (CIs). Selected potential confounding factors in a multivariable model were as follows: age (for one increment of age), origin (cardiac, noncardiac), gender (men, women), witness status (bystander, none), first documented rhythm (VF, non-VF), bystander CPR (yes, no), EMS response time (the time from call to contact with a patient, for one increment of minute), and year of arrest (for one increment of year). All tests were 2 tailed and p values <0.05 were considered statistically significant. All statistical analyses were made using SPSS statistical package, ver20.0 J (IBM Corp. Armonk, New York).
Results
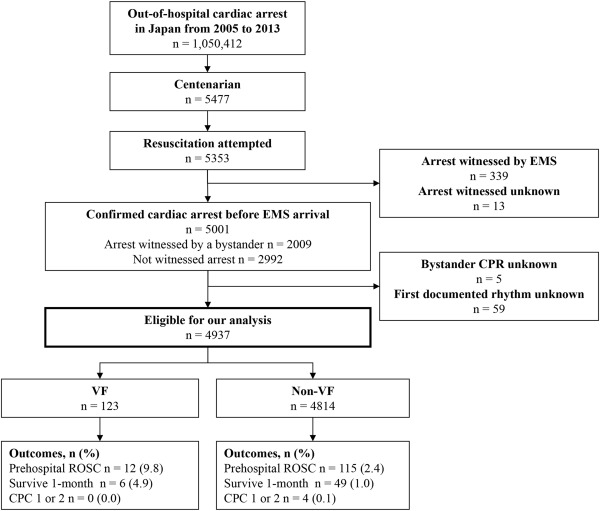
A patient flow of those with OHCA based on the Utstein-style template is noted in Figure 1 . Of the 1,050,412 OHCAs in Japan, a total of 5,477 centenarians with OHCAs were identified over 9 years. Resuscitation was attempted in 5,353 (97.7%), and 5,001 centenarians with OHCAs before EMS arrival (2,009 witnessed by a bystander and 2,992 not witnessed) were confirmed. Excluding victims without information on bystander CPR and first documented rhythm, 4,937 were eligible for our analyses. Of them, 123 (2.5%) had VF and 4,814 (97.5%) had non-VF. The proportion of 1-month survival from OHCAs in centenarians was 1.1% (55 of 4,937), and the proportion of those with VF and those with non-VF were 4.9% and 1.0%, respectively. Only 4 patients with non-VF had better neurologic outcome.
Patient and EMS characteristics of 4,937 centenarians with OHCAs before EMS arrival are listed in Table 1 . Median age was 101, and the proportions of OHCA centenarians aged 100, 101, 102, 103, 104, and ≥105 years were 38.3%, 24.7%, 15.7%, 9.4%, 5.3%, and 6.6%, respectively. The proportion of OHCAs with cardiac origin was 64.0%. Women accounted for 80.3%. VF as first documented rhythm was 2.5%. The proportion of those shocked by public-access AEDs and received bystander CPR were 0.8% and 64.2%, respectively (17.7% compression-only CPR and 46.5% conventional CPR). Median EMS response and hospital arrival times were 8 and 29 min, respectively.
| Variable | Total (n=4937) |
|---|---|
| Age (years, median [IQR]) | 101 (100 – 102) |
| Age, years | |
| 100 | 1893 (38.3%) |
| 101 | 1218 (24.7%) |
| 102 | 773 (15.7%) |
| 103 | 463 (9.4%) |
| 104 | 262 (5.3%) |
| 105 | 148 (3.0%) |
| 106 | 88 (1.8%) |
| 107 | 39 (0.8%) |
| 108 | 22 (0.4%) |
| 109 | 18 (0.4%) |
| 110 | 10 (0.2%) |
| 111 | 3 (0.1%) |
| Origin | |
| Cardiac | 3162 (64.0%) |
| Non-cardiac | 1775 (36.0%) |
| External cause | 460 (9.3%) |
| Respiratory disease | 455 (9.2%) |
| Cerebrovascular disease | 83 (1.7%) |
| Malignant tumor | 40 (0.8%) |
| Other | 737 (14.9%) |
| Gender | |
| Men | 973 (19.7%) |
| Women | 3964 (80.3%) |
| Type of bystander-witness status | |
| None | 2960 (60.0%) |
| Family | 895 (18.1%) |
| Non-family member | 1082 (21.9%) |
| First documented rhythm | |
| Ventricular fibrillation | 123 (2.5%) |
| Pulseless electrical activity | 973 (19.7%) |
| Asystole | 3841 (77.8%) |
| Shock by public-access automated external defibrillators | 39 (0.8%) |
| Type of bystander-initiated cardiopulmonary resuscitation | |
| None | 1766 (35.8%) |
| Chest compression-only cardiopulmonary resuscitation | 873 (17.7%) |
| Conventional cardiopulmonary resuscitation with rescue breathing | 2298 (46.5%) |
| Intravenous fluid | 823 (16.7%) |
| Epinephrine | 284 (5.8%) |
| Endotracheal intubation | 272 (5.5%) |
| EMS response time (call to contact with a patient) (min, median [IQR]) | 8 (6 – 10) |
| Hospital arrival time (call to hospital arrival) (min, median [IQR]) | 29 (23 – 36) |
Figure 2 shows trends in the number of centenarians with OHCAs before EMS arrival by gender and the proportion of 1-month survival from OHCAs in whole centenarians. The number of those with OHCAs increased from 70 in 2005 to 136 in 2013 in men (p for trend <0.001) and from 227 in 2005 to 587 in 2013 in women (p for trend <0.001). The proportion of 1-month survival did not improve during the study period (p for trend = 0.346).
In a multivariate analysis ( Table 2 ), age was not associated with 1-month survival from OHCAs in centenarians (adjusted OR for one increment of age 1.01; 95% CI 0.87 to 1.18). OHCAs of cardiac origin had significantly poor 1-month survival compared with those of noncardiac origin (adjusted OR 0.37; 95% CI 0.21 to 0.64). Witness by a bystander (adjusted OR 3.45; 95% CI 1.88 to 6.31) and VF as first documented rhythm (adjusted OR 5.49; 95% CI 2.24 to 13.43) were significant positive predictors of 1-month survival. In contrast, bystander CPR (adjusted OR 1.07; 95% CI 0.62 to 1.86) and earlier EMS response time (adjusted OR 0.82; 95% CI 0.58 to 1.17) tended to improve 1-month survival, although it was statistically insignificant.
| Variable | One-month survival | OR | |
|---|---|---|---|
| % (n/N) | Crude (95% CI) | Adjusted (95% CI) | |
| Age (for one increment of age) | 1.02 (0.88-1.18) | 1.01 (0.87-1.18) | |
| Origin | |||
| Cardiac | 0.6 (20/3162) | 0.32 (0.18-0.55) | 0.37 (0.21-0.64) |
| Non-cardiac | 2.0 (35/1775) | Reference | Reference |
| Gender | |||
| Men | 0.9 (9/973) | 0.80 (0.39-1.63) | 0.78 (0.38-1.61) |
| Women | 1.2 (46/3964) | Reference | Reference |
| Witness status | |||
| Bystander | 2.0 (40/1977) | 4.05 (2.23-7.36) | 3.45 (1.88-6.31) |
| None | 0.5 (15/2960) | Reference | Reference |
| First documented rhythm | |||
| Ventricular fibrillation | 4.9 (6/123) | 4.99 (2.09-11.87) | 5.49 (2.24-13.43) |
| Non-ventricular fibrillation | 1.0 (49/4814) | Reference | Reference |
| Bystander cardiopulmonary resuscitation | |||
| Yes | 1.2 (32/2639) | 1.21 (0.71-2.08) | 1.07 (0.62-1.86) |
| No | 1.0 (23/2298) | Reference | Reference |
| Emergency medical service response time (for one-increment of minute) | 0.94 (0.86-1.03) | 0.82 (0.58-1.17) | |
| Year (for one-increment of year) | 0.95 (0.85-1.06) | 0.94 (0.85-1.05) | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


