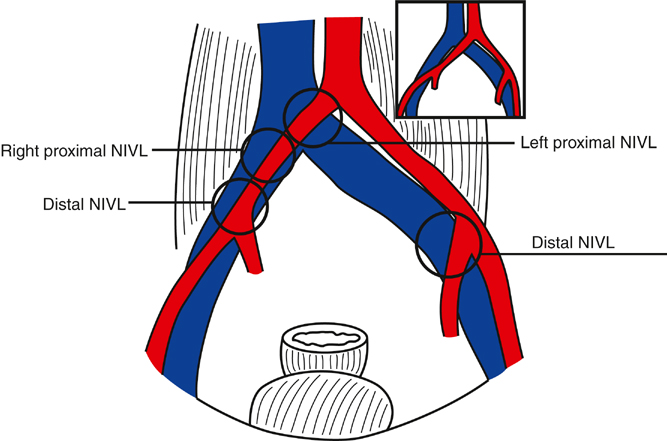
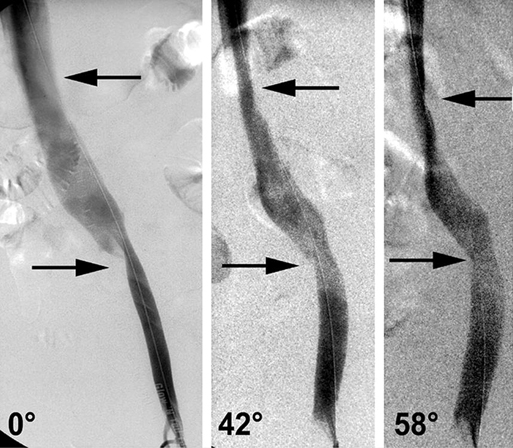
IVUS has greatly expanded current knowledge regarding NIVL. It occurs on both sides and in both sexes, involves all age groups, and is not confined to the left lower limb of young women as previously thought. NIVLs occur not only at the classic proximal site near the iliac–caval junction but also distally (Figures 1 and 2).
Endovascular Treatment of Chronic Venous Occlusion
Pathophysiology
Postthrombotic Disease
Nonthrombotic (Primary) Disease
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Key
Fastest Thoracic Insight Engine
