Endovascular Repair of Acute Aortic Transection
STEPHANIE M. CARVALHO and MARK F. CONRAD
Presentation
A 54-year-old man with no past medical history presents to the emergency department after he struck the handlebars of his dirt bike while attempting to jump 75 feet. He was wearing a helmet and had no loss of consciousness. He was ambulating at the scene but complained of difficulty breathing. First responders noted subcutaneous emphysema and decreased breath sounds. They attempted bilateral needle decompression of his lungs in the field with no relief of symptoms. He continued to decompensate in the field and was intubated and transported to the emergency department. His vitals upon presentation are blood pressure (BP) 90/50, heart rate (HR) 110 beats per minute, oxygen saturation (O2 Sat) 90%, and Glasgow Coma Scale 4T (patient is intubated and withdraws to pain). He has bruising on his sternum and substantial subcutaneous emphysema that extends from the shoulders to the diaphragm. The normal trauma protocol is followed, during which he receives two large-bore IVs, undergoes a negative FAST exam, and has bilateral 36-F chest tubes placed with return of 500 mL of blood from the left chest and no blood from the right. He responds to the fluid and chest decompression, and his vitals improve to BP 120/60 and HR 80, and pulse oximetry is 100%. The following x-ray is obtained (Fig. 1).
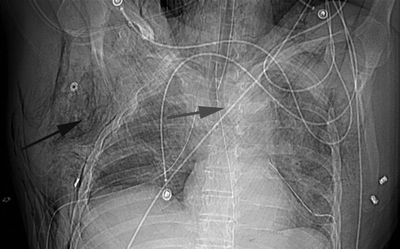
FIGURE 1 The patient’s initial supine chest x-ray. It shows that the patient has an endotracheal tube and bilateral chest tubes in place. The red arrow points to the widened mediastinum. The black arrow points to the extensive subcutaneous emphysema seen throughout the x-ray.
Differential Diagnosis
The main pathologic causes of a widened mediastinum on chest x-ray are chest masses and enlargement of the great vessels. Common masses include lymphoma, thyroid enlargement, teratoma, and thymus tumors. An aneurysm of the aortic arch or descending thoracic aorta will also lead to a widened mediastinum. However, in a patient with a significant mechanism of blunt injury to the chest, the most likely cause is a traumatic aortic tear, and this must be diagnosed expediently.
Workup
A high-velocity head-on motor vehicle crash or blunt force to the chest leads to rapid deceleration of the body and can cause the aorta to tear along its attachment at the ligamentum arteriosum. A history of this mechanism of injury should increase the index of suspicion for a traumatic aortic tear. Other major injuries to the chest such as multiple rib fractures, flail chest, or pulmonary contusion should also make one think of an acute aortic tear, as should a widened mediastinum on chest x-ray. In the setting of blunt chest trauma, if there is a suspicion of traumatic aortic tear, the next test to obtain is a CT angiogram of the chest. These patients usually present with multiple injuries, and most trauma protocols involve scanning the chest, abdomen, and pelvis at the same time to identify occult solid organ injuries. It is important to stabilize the patient using the ABCs of trauma resuscitation prior to traveling from the trauma bay to radiology for further imaging studies.
Chest CTA
In the region of the aortic isthmus distal to the origin of the left subclavian artery, there is intimal injury with elevation of an intimal flap and pseudoaneurysm of the descending aorta at the level of the ligamentum arteriosum (Fig. 2). There is also accompanying intraluminal thrombus. The pseudoaneurysm is located approximately 2.2 cm distal to the origin of the left subclavian artery. There is an intermediate density hematoma surrounding the descending aorta to the level of the renal arteries with no evidence of active extravasation.
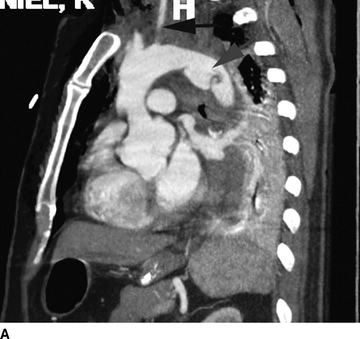
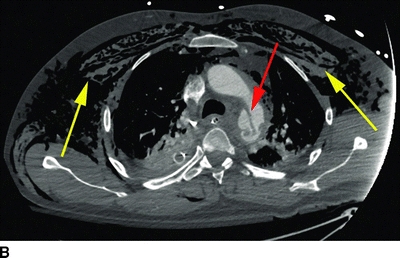
FIGURE 2 A: This is an oblique view of the aorta showing the aortic tear (red arrow) with intima floating free within the aorta and surrounding hematoma of the pseudoaneurysm. The left subclavian artery (black arrow) is proximal to the tear. B: Axial view of the chest showing the extensive subcutaneous emphysema (yellow arrows). The aortic tear has led to a complex infolding of the intima with surrounding hematoma (red arrow).
Diagnosis
Grade 3 traumatic aortic tear.
Discussion
Although rare, injury to the thoracic aorta is the second leading cause of death (head injury is most common) after blunt force trauma. This is usually a lethal condition with a greater than 80% mortality rate at the scene of the accident, and contemporary autopsy studies of patients after blunt trauma have reported the incidence of aortic rupture to be approximately 30%. The most common mechanism for this injury remains motor vehicle crashes, especially head on collisions because of the transfer of energy between the two vehicles and the rapid deceleration that is experienced by their occupants.
Traumatic aortic injuries occur across a spectrum of lesions, and a grading system has been developed to help guide management. A grade 1 injury amounts to an intimal tear with no violation of the media or adventitia of the aorta. These are usually treated conservatively with medical management. Grade 2 injuries involve the intima and media of the aorta and present as in intramural hematoma. These represent a gray zone of management as many can be treated medically with serial CTA follow-up, but some will progress to rupture and need treatment. Although the general recommendation is to treat grade 2 injuries, it is important to consider the patient’s overall condition when addressing these lesions. A grade 3 injury involves all three layers of the aorta with pseudoaneurysm formation, and a grade 4 injury is a frank rupture. Both of these injuries require early intervention.
Medical management consists of strict BP control with beta blockade and afterload reduction in order to decrease aortic wall stress. It is common for these patients to have other injuries and repair of a grade 2 to 3 tear may have to be deferred for more pressing injuries such as an actively bleeding pelvic fracture or solid organ injury. The current Society for Vascular Surgery (SVS) guidelines recommend that all patients with grade 2 to 4 injuries undergo repair. In the absence of other injuries, repair should be performed within 24 hours of the initial presentation if possible.
Preoperative Planning
The CTA should be used to develop an operative plan. It is important to have 2 cm of normal aorta proximal to the tear in order to obtain an adequate seal. Due to the location of the aortic tear, it is common to have to cover the left subclavian artery but the graft rarely needs to extend beyond the origin of the left common carotid artery. In the emergent setting, we have not routinely revascularized the left subclavian artery with a carotid to subclavian bypass as this will delay therapy and is unnecessary in most patients. The diameter of the aorta is measured in the proximal seal zone and then 10 cm distally. It is best to obtain these measurements in the centerline fashion using three-dimensional image planning software. If this is not available or an accurate diameter cannot be obtained, intravascular ultrasound (IVUS) can be used to obtain an accurate centerline measurement during the procedure. Finally, the access vessels need to be assessed for adequate size to deliver a 20- to 24-F sheath (needs to be at least 7 mm in diameter without calcium). This can be an issue in young females, and a conduit may be needed to safely deliver the device.
There are currently two commercially available stent grafts in the United States with an indication for traumatic tear. They are the Conformable GORE TAG Thoracic Endoprosthesis (W.L. Gore and Associates Inc., Flagstaff, AZ) and the Valiant Captivia Stent Graft (Medtronic, Santa Rosa, CA). Grafts are chosen based upon the sizing recommendations of the manufacturer. Ultimately, the oversizing may be determined by what is stocked on the OR shelves such that centers with a high volume of blunt thoracic injuries should have a good selection of grafts available.
Case Continued
The patient was placed in the supine position with a roll under the left chest to improve visualization of the aortic arch. The abdomen and groins were prepped and draped in a sterile fashion. The left common femoral artery was exposed through a small transverse incision. The patient was given 5000 U of heparin. A Kumpe catheter was used to drive a glidewire beyond the lesion and into the arch. A stiff wire was then placed. The IVUS catheter was advanced over the wire through a 9-F sheath and was used to identify the pseudoaneurysm and the proximal and distal seal zones (Fig. 3). The proximal seal zone was measured to be 28 mm by IVUS, and the distal was 24 mm. A tapered stent graft (32 to 28 mm) with a 120-mm length was chosen. A pigtail catheter was advanced into the aorta from a 5-F sheath placed in the opposite groin. An angiogram was performed prior to graft deployment (Fig. 4), and the graft was deployed so that it partially covered the left subclavian artery (Fig. 5). There were no endoleaks so the graft was not ballooned. The hardware was removed and the artery was repaired with a 5-0 Prolene stitch.
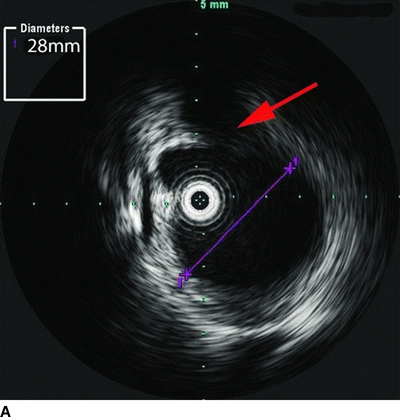
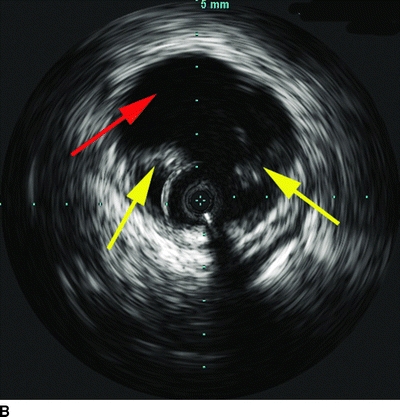
FIGURE 3 A: Static IVUS image of the aorta proximal to the traumatic tear. The purple line gives a true centerline measurement of 28 mm at the level of the origin of the left subclavian artery (red arrow). B: Static IVUS image of the aortic tear. The intimal flaps are free flowing in the aorta (yellow arrows), and there is a contained pseudoaneurysm outside the aortic wall (red arrow).



