There is no large-scale population-based study to clarify the association between major adverse cardiovascular events (MACEs) and pre-eclampsia/eclampsia. A population-based Taiwanese cohort study was performed in 1,132,064 parturients from 1999 to 2003 using a dataset linking birth certificates and National Health Insurance hospital discharge data. Sociodemographic factors and obstetric complications were used in multivariate logistic regression models to determine adjusted hazard ratios of pre-eclampsia/eclampsia on risks of MACEs and mortality during pregnancy to at least the third year postpartum. Incidence rates of MACEs and all maternal mortality in women with pre-eclampsia/eclampsia were 16.21 and 40.38 per 100,000 patients per year, respectively. Women with pre-eclampsia/eclampsia had a 13.0-fold higher incidence of myocardial infarction, a 8.3-fold higher incidence of heart failure, a 14.5-fold higher incidence of stroke, a 12.6-fold higher incidence of MACEs, a 7.3-fold higher incidence of MACEs without stroke, a 2.3-fold higher incidence of MACE-related deaths, and a 6.4-fold higher incidence of overall death than women without pre-eclampsia/eclampsia. Kaplan-Meier survival curve discriminated in MACEs, nonstroke MACEs, MACE related death and overall death. In conclusion, women with pre-eclampsia/eclampsia have a significantly higher risk of MACEs, especially myocardial infarction and stroke, during pregnancy and their risk remains significant to ≥36 months postpartum. Our results suggest that women with pre-eclampsia/eclampsia should be closely monitored during pregnancy and for up to ≥3 years postpartum.
Our previous study showed that Taiwanese peripartum women with pre-eclampsia/eclampsia have a significantly higher risk of stroke during pregnancy and in the first postpartum year. Many studies have shown that pre-eclampsia/eclampsia increases life-long risk of major adverse cardiovascular events (MACEs) after pregnancy mainly in Western populations. However, whether pre-eclampsia/eclampsia also poses a higher risk for other MACEs such as myocardial infarction (MI), heart failure, percutaneous cardiac intervention, coronary artery bypass grafting, malignant dysrhythmia, cardiac shock, thrombolysis, or implantable cardiac defibrillator in Asian women such as women in Taiwan remains unanswered. To our best knowledge, there is no large-scale study evaluating overall major cardiovascular risks during pregnancy in Asian populations. Moreover, few studies have examined the period beyond postpartum. This study is a large-scale, population-based study in an Asian population with an observation period that included pregnancy extending to the third postpartum year. The present study provides the incidence of MACE in Taiwanese women for 1999 to 2003 based on birth certificate data linked with National Health Insurance (NHI) claims data to determine risk of MACEs in women from pregnancy to the third postpartum year.
Methods
Data for this study were obtained from 3 main sources. The first source was birth registries from 1999 to 2003 provided by the ministry of the interior. This dataset contains comprehensive information about birth and parents’ data, including age, education, marital status, infant birth weight, gestational weeks, infant sex, and multiple births. The second source was the NHI hospital discharge data covering 1996 to 2004, a nationwide population-based data including >21 million enrollees, representing about 97% of the Taiwanese population. It provided inpatient registries from all medical facilities contracted with the NHI and contained information on all admissions including new-onset MACEs in peripartum women and all deliveries with 1 principal and 4 secondary International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes. The third source was death files from 1996 to 2004 that provide the incidence of death and cause of death.
A mother’s date of birth and her unique personal identification number were used to link birth certificate data, NHI claims dataset, and death files. All personal identifiers were encrypted by the NHI bureau before release to the researchers. Confidentiality assurances were addressed by following data regulations of the NHI bureau and institutional review board approval was waived.
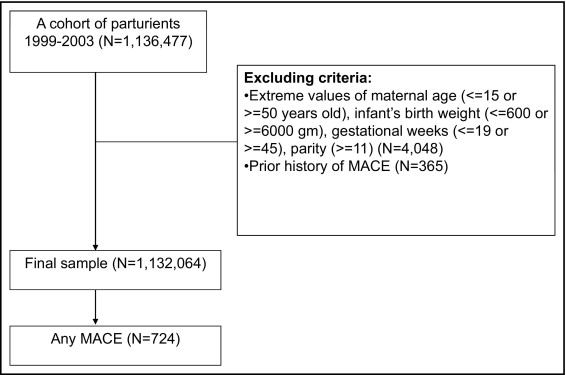
The study cohort consisted of 1,136,477 birth records for 1999 to 2003 for which the birth certificate dataset and delivery entries in the NHI hospital discharge data were successfully linked. In total 4,048 data entries, representing 0.36% of the total sample, had extreme values of maternal age (≤15 or ≥50 years old), infant’s birth weight (≤600 or ≥6,000 g), gestational weeks (≤19 or ≥45), and parity (≥11) and were therefore excluded. To examine risk factors of MACEs occurring during the prenatal period, an index date was created by subtracting 90 days from the date of delivery. Also, cases of MACEs before the index date were excluded from analyses (n = 365) to avoid the potential confounding factor of a history of major cardiovascular events. The final sample available for analyses was 1,132,064 ( Figure 1 ).
To identify any MACE, each case was tracked from the index date until the end of 2004 or the date of death, whichever came first. Women who were alive without MACEs were censored on December 31, 2004. Cases of MACE were further classified as MI (ICD-9-CM code 410-410.9), heart failure (ICD-9-CM codes 428.0 to 428.10), percutaneous cardiac intervention (ICD-9-CM codes 36.0 to 36.03, 36.05 to 36.09), coronary artery bypass grafting (ICD-9-CM codes 36.1 to 36.99, V45.81), cerebrovascular accident (stroke; ICD-9-CM codes 430 to 432, 433 to 437), malignant dysrhythmia (ICD-9-CM codes 246.0, 426.12 to 426.13, 426.51 to 426.52, 426.54, 427.1, 427.4, 427.41 to 427.42, 427.5), cardiac shock (ICD-9-CM code 785.51), thrombolysis (ICD-9-CM codes 36.0 to 36.99), or implantable cardiac defibrillator (ICD-9-CM code V4502). Occlusion or stenosis of precerebral (extracranial) arteries without infarction (codes 430.00, 431.00, 433.20, 433.30, 433.80, 43.390, 434.90, 434.00, 434.10, and 434.90) was not considered a MACE. Basilar, vertebral, and subclavian artery syndrome (codes 435.0 to 435.3), hypertensive encephalopathy (437.2), nonruptured cerebral aneurysm (437.3), cerebral arteritis (437.4), and Moyamoya disease (437.5) were excluded unless accompanied by a code concerning cerebral infarction or cerebral hemorrhage.
Nonstroke MACEs were examined in particular to determine whether pre-eclampsia/eclampsia increases the risk of other types of MACE except stroke. MACE-related death and death were identified from ICD-9-CM codes of causes of death in death files.
The subject of interest was pre-eclampsia/eclampsia, which was defined by ICD-9-CM codes 642.4 to 642.7 as the secondary diagnosis in the index discharge of delivery. Regression models also adjusted for maternal characteristics that increase cardiovascular risk such as age, education, marital status, and parity. In addition, models adjusted for infant characteristics such as sex, birth weight, and gestational week. Details on selected pregnancy and obstetric complications including multiple gestations (ICD-9-CM diagnosis code 651), diabetes mellitus (648.0/250), long-term hypertension (401 to 405), pregnancy-related hypertension (642.0 to 642.3/642.9/760.0), anemia (648.2/285.0), antepartum hemorrhage (641/640.9), postpartum hemorrhage (666/667/669.1), and cesarean delivery (procedure codes 74.0 to 74.4) were also extracted from NHI claims data at time of discharge after delivery. Multiple pregnancies, diabetes, long-term hypertension, pregnancy-related hypertension, cesarean delivery, and systemic lupus erythematous were entered because they were risk factors of MACEs reported by previous studies. Other factors such as age, education level, marital status, sex of infant, parity, gestational weeks, birth weight, postpartum hemorrhage, and antepartum hemorrhage were entered to examine their possible association with risk of MACEs.
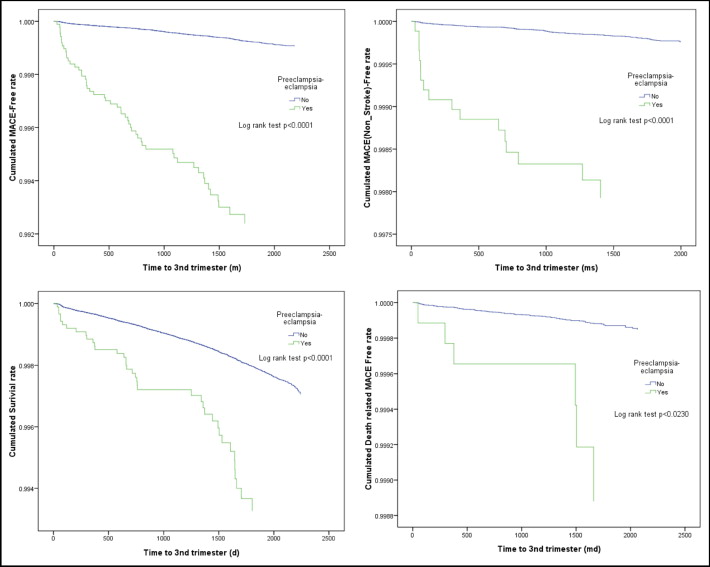
Incidence rates of MACEs or MACE-related death were calculated among patient clinical and sociodemographic groups. MACE-free survival rates were estimated using the Kaplan-Meier method, and log-rank test was used to examine the effect of pre-eclampsia/eclampsia on MACE-free, nonstroke MACE-free, MACE-related death-free, and survival rates ( Figure 2 ). Cox proportional regression was then used to examine the independent effect of pre-eclampsia/eclampsia on the incidence of each type of MACE, nonstroke MACE, any MACE, MACE-related death, or death. Hazard ratios and 95% confidence intervals were determined and a p value <0.05 was considered statistically significant. All analyses were performed using SAS/Stat 9.01 for Windows (SAS Institute, Cary, North Carolina).
Results
There were 1,132,064 pregnancies identified during the study period; of these 68% of mothers were ∼25 to 34 years old, 97% of pregnancies were single gestation and 46% were nulliparous, and 724 cases of MACEs occurred from the third trimester of pregnancy to the end of 2004. Table 1 presents the distribution of MACE cases among sociodemographic and clinical groups.
| MACEs | MACE-Related Death | Any Death | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MI | Heart Failure | PCI | CABG | Stroke | Malignant Dysrhythmia | Cardiac Shock | Thrombolysis | Any MACEs | Any MACEs (without stroke) | |||
| Total | 33 (0.74%) | 99 (2.22%) | 8 (0.18%) | 7 (0.16%) | 518 (11.59%) | 70 (1.57%) | 1 (0.02%) | 13 (0.29%) | 724 (16.21%) | 207 (4.63%) | 118 (2.64%) | 1,803 (40.38%) |
| Age (years) | ||||||||||||
| ≤24 | 2 (0.21%) | 25 (2.6%) | 85 (8.83%) | 12 (1.25%) | 124 (12.88%) | 39 (4.05%) | 29 (3.01%) | 401 (41.69%) | ||||
| 25–34 | 19 (0.63%) | 53 (1.75%) | 7 (0.23%) | 4 (0.13%) | 331 (10.9%) | 46 (1.51%) | 1 (0.03%) | 9 (0.3%) | 452 (14.89%) | 122 (4.02%) | 65 (2.14%) | 1,069 (35.23%) |
| ≥35 | 12 (2.56%) | 21 (4.47%) | 1 (0.21%) | 3 (0.64%) | 102 (21.74%) | 12 (2.56%) | 4 (0.85%) | 148 (31.56%) | 46 (9.8%) | 24 (5.11%) | 333 (71.05%) | |
| Education level (years) | ||||||||||||
| ≤9 | 6 (0.55%) | 41 (3.79%) | 1 (0.09%) | 3 (0.28%) | 181 (16.74%) | 14 (1.29%) | 4 (0.37%) | 243 (22.47%) | 63 (5.82%) | 43 (3.98%) | 715 (66.19%) | |
| >9 | 27 (0.8%) | 58 (1.71%) | 7 (0.21%) | 4 (0.12%) | 337 (9.95%) | 56 (1.65%) | 1 (0.03%) | 9 (0.27%) | 481 (14.2%) | 144 (4.25%) | 75 (2.21%) | 1,088 (32.14%) |
| Married | ||||||||||||
| Yes | 32 (0.74%) | 89 (2.05%) | 8 (0.18%) | 7 (0.16%) | 494 (11.4%) | 67 (1.55%) | 1 (0.02%) | 13 (0.3%) | 686 (15.83%) | 193 (4.45%) | 111 (2.56%) | 1,644 (37.96%) |
| No | 1 (0.74%) | 10 (7.41%) | 24 (17.78%) | 3 (2.22%) | 38 (28.16%) | 14 (10.37%) | 7 (5.19%) | 159 (118.06%) | ||||
| Number of gestations | ||||||||||||
| Single | 32 (0.74%) | 96 (2.22%) | 8 (0.18%) | 7 (0.16%) | 502 (11.59%) | 66 (1.52%) | 1 (0.02%) | 13 (0.3%) | 700 (16.16%) | 199 (4.59%) | 116 (2.68%) | 1,739 (40.16%) |
| Multiple | 1 (0.74%) | 3 (2.22%) | 16 (11.87%) | 4 (2.97%) | 24 (17.81%) | 8 (5.93%) | 2 (1.48%) | 64 (47.51%) | ||||
| Infant sex | ||||||||||||
| Male | 13 (0.56%) | 48 (2.05%) | 4 (0.17%) | 3 (0.13%) | 259 (11.09%) | 38 (1.63%) | 1 (0.04%) | 5 (0.21%) | 357 (15.28%) | 99 (4.24%) | 56 (2.4%) | 955 (40.9%) |
| Female | 20 (0.94%) | 51 (2.39%) | 4 (0.19%) | 4 (0.19%) | 259 (12.15%) | 32 (1.5%) | 8 (0.38%) | 367 (17.22%) | 108 (5.07%) | 62 (2.91%) | 848 (39.8%) | |
| Birth weight (g) | ||||||||||||
| <4,000 | 33 (0.76%) | 96 (2.21%) | 8 (0.18%) | 7 (0.16%) | 494 (11.39%) | 69 (1.59%) | 1 (0.02%) | 13 (0.3%) | 696 (16.05%) | 203 (4.68%) | 115 (2.65%) | 1,737 (40.06%) |
| ≥4,000 | 3 (2.31 | 24 (18.48 | 1 (0.77 | 28 (21.56 | 4 (3.08 | 3 (2.31 | 66 (50.85 | |||||
| Nulliparous | ||||||||||||
| Nulliparous | 11 (0.54%) | 45 (2.21%) | 2 (0.1%) | 4 (0.2%) | 192 (9.41%) | 29 (1.42%) | 4 (0.2%) | 278 (13.63%) | 86 (4.21%) | 44 (2.16%) | 709 (34.77%) | |
| Multiparous | 22 (0.91%) | 54 (2.22%) | 6 (0.25%) | 3 (0.12%) | 326 (13.43%) | 41 (1.69%) | 1 (0.04%) | 9 (0.37%) | 446 (18.37%) | 121 (4.98%) | 74 (3.05%) | 1,094 (45.09%) |
| Risk factor | ||||||||||||
| Cesarean delivery | 18 (1.18%) | 58 (3.79%) | 3 (0.2%) | 2 (0.13%) | 254 (16.59%) | 36 (2.35%) | 5 (0.33%) | 367 (23.98%) | 113 (7.38%) | 51 (3.33%) | 690 (45.1%) | |
| Systemic lupus erythematosus | 3 (54.13%) | 2 (36.1%) | 2 (36.07%) | 7 (126.62%) | 2 (36.07%) | 12 (217.83%) | 5 (90.39%) | 1 (18.02%) | 27 (491.12%) | |||
| Long-term hypertension | 2 (212.86%) | 1 (105.98%) | 3 (320.05%) | 2 (212.86%) | 1 (105.75%) | |||||||
| Pregnancy-related hypertension | 1 (6.29%) | 9 (56.62%) | 10 (62.93%) | 1 (6.29%) | 22 (138.69%) | |||||||
| Anemia | 3 (4.38%) | 10 (14.6%) | 1 (1.46%) | 14 (20.44%) | 4 (5.84%) | 7 (10.22%) | 43 (62.84%) | |||||
| Diabetes mellitus | 1 (17.06%) | 2 (34.15%) | 1 (17.06%) | 1 (17.06%) | 6 (102.52%) | 2 (34.14%) | 2 (34.13%) | 11 (188.36%) | 5 (85.47%) | 1 (17.06%) | 8 (136.86%) | |
| Antepartum hemorrhage | 1 (1.12%) | 5 (5.58%) | 22 (24.54%) | 1 (1.12%) | 29 (32.36%) | 7 (7.81%) | 6 (6.69%) | 50 (55.82%) | ||||
| Postpartum hemorrhage | 2 (7.4%) | 3 (11.11%) | 1 (3.7%) | 6 (22.23%) | 3 (11.11%) | 4 (14.81%) | 40 (148.78%) | |||||
| Pre-eclampsia/eclampsia | 5 (14.25%) | 11 (31.38%) | 1 | 1 (2.85%) | 39 (111.4%) | 1 (2.85%) | 2 (5.7%) | 56 (160.17%) | 17 (48.51%) | 6 (17.1%) | 39 (111.38%) | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


