Liver function test (LFT) abnormalities are often observed in patients with heart failure (HF). However, the relation of LFTs with outcomes has not been well described. Patients of the VA Palo Alto Health Care System (3 inpatient facilities and 7 community clinics) with a complete set of LFTs in the 60 days before a first HF diagnosis were included in the analysis from January 2005 to April 2013. A total of 2,096 patients met inclusion criteria. Patients were a mean of 71 ± 12 years old, 97% were men, 57% had a previous diagnosis of ischemic heart disease, and the mean left ventricular ejection fraction was 51 ± 12%. The median (twenty fifth and seventy fifth) values were albumin 3.6 g/dl (3.3, 3.9), alanine transaminase 21 IU/L (16, 30), aspartate transaminase 24 IU/L (20,31), AP 70 IU/L (57, 87), and total bilirubin 0.8 mg/dl (0.6, 1.0). There were 851 deaths (41%) over a mean duration of 41 ± 27 months. Mortality significantly increased with lower values of albumin and alanine transaminase and higher levels of aspartate transaminase and AP. The association with total bilirubin was not significant. In conclusion, many LFT values in the “normal” range are independently associated with decreased survival beyond traditional risk factors for mortality in HF.
Liver function test (LFT) abnormalities are prevalent in both ambulatory and hospitalized patients with heart failure (HF) and may be independently associated with adverse outcomes. Thus, the Veterans Affairs (VA) Health Care System provides a unique opportunity to investigate the epidemiology and prognostic value of LFTs in a heterogeneous patient population including ischemic and nonischemic causes of HF, systolic and diastolic dysfunction, and across the inpatient and outpatient settings. Specifically, the objectives of this retrospective analysis were (1) to determine the prevalence and pattern of LFT abnormalities and (2) to evaluate the association between LFTs and morbidity and mortality in patients with de novo or newly diagnosed HF.
Methods
Patients of the VA Palo Alto Health Care System, which includes 3 inpatient facilities and 7 community clinics, with a complete set of LFTs in the 60 days before a first HF diagnosis were included in the analysis from January 2005 to April 2013. A cutoff of 60 days was chosen a priori to standardize the time frame from LFT measurement to first HF diagnosis. LFTs (threshold for abnormal value) included albumin (Alb ≤3.2 g/dl), alanine transaminase (ALT ≥45 IU/L), aspartate transaminase (AST ≥41 IU/L), alkaline phosphatase (AP ≥113 IU/L), and total bilirubin (T Bili ≥1.3 mg/dl). A diagnosis of HF was made based on the International Classification of Disease, Ninth Revision ( ICD-9 ) (i.e., 428.xx, 429.3, 402.01, 402.11, 402.91, 425.xx, or diagnosis-related group of 127). Only the first complete set of LFTs was used for the present analysis.
Co-morbid conditions were defined using the ICD-9 diagnostic coding for the Charlson co-morbidity criteria. Additional co-morbidities were defined as follows: hypertension ( ICD-9 401 to 405) and ischemic heart disease ( ICD-9 410 to 414). Medication data were obtained using VA pharmacy records for filled prescriptions and included all prescriptions filled 6 months before LFT measurement. Survival was determined based on the VA Beneficiary Identification Records Locator Subsystem death file and the Social Security Death Index. The primary outcome was all-cause mortality. Secondary outcomes included all-cause hospitalization and HF-specific hospitalization.
All data were reported as a number (%), mean ± SD, or a median (twenty fifth and seventy fifth). The association between LFTs and outcomes were assessed using univariate and proportional hazards analysis. The multivariable model included all LFTs and was adjusted for age, gender, race, left ventricular EF, ischemic origin, medical co-morbidities (i.e., hypertension, previous myocardial infarction, diabetes mellitus, and chronic kidney disease), blood urea nitrogen and creatinine, serum sodium, hemoglobin, and any admission for HF or other hospitalization in the previous year. All statistical analyses were 2 tailed with a threshold for significance set at p value <0.05. Final analyses were conducted using SAS software, version 9.2 (SAS Inc., Cary, North Carolina).
Results
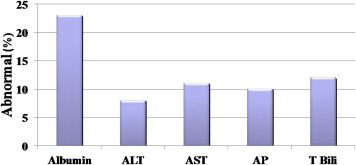
A total of 2,096 patients from January 2005 to April 2013 met inclusion criteria. Twenty-six percent of patients had LFTs measured during hospitalization, whereas the remainder had LFTs measured in the outpatient setting. Patients were a mean age of 71 ± 12 years old, 97% were men, and the mean left ventricular EF was 51 ± 12%. Approximately 60% of patients had a previous diagnosis of ischemic heart disease, and the prevalence of medical co-morbidities was high ( Table 1 ). Utilization of guideline-directed medical therapies was low, but the study population was defined based on a recent diagnosis of HF and the proportion of patients with a preserved EF was high. At baseline, with the notable exception of Alb, most patients had LFT measurements within the normal range, and the prevalence of LFT abnormalities was low ( Table 2 , Figure 1 ).
| Variable | Study Population (N = 2096) |
|---|---|
| Age, mean±standard deviation (years) | 71±12 |
| Men | 2033 (97%) |
| White | 1667 (80%) |
| Black | 150 (7%) |
| Unknown | 279 (13%) |
| Ejection Fraction (%), mean±standard deviation | 51±12 |
| Ischemic etiology | 1203 (57%) |
| Hypertension | 1714 (82%) |
| Diabetes Mellitus | 966 (46%) |
| Chronic Kidney Disease | 464 (22%) |
| β-blockers | 723 (34%) |
| Serum Na | 139±3 |
| Hemoglobin | 13.0±2.0 |
| Creatinine | 1.4±1.0 |
| Blood urea nitrogen | 24±14 |
| B-type natriuretic peptide | 245 (93, 536) |
| Angiotensin-Converting Enzyme Inhibitors/Angiotensin Receptor Blockers | 734 (35%) |
| Mineralocorticoid Receptor Antagonists | 86 (4%) |
| Digoxin | 96 (5%) |
| Loop Diuretics | 547 (26%) |
| Variable | Median | 25 th | 75 th |
|---|---|---|---|
| Albumin (g/dL) | 3.6 | 3.3 | 3.9 |
| Alanine transaminase (IU/L) | 21 | 16 | 30 |
| Aspartate transaminase (IU/L) | 24 | 20 | 31 |
| Alakine phosphatase (IU/L) | 70 | 57 | 87 |
| Total Bilirubin (mg/dL) | 0.8 | 0.6 | 1.0 |
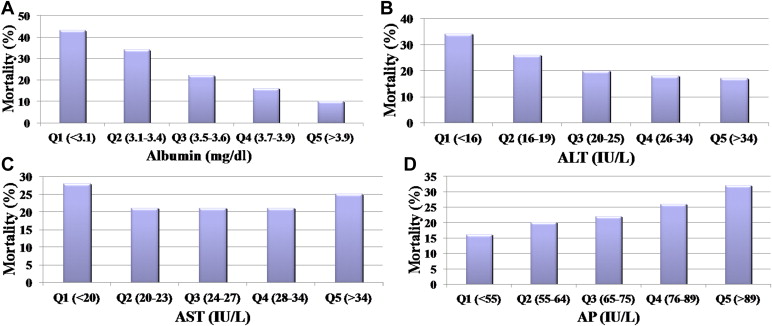
There were a total of 851 deaths (41%) over a mean duration of 41 ± 27 months. In general, mortality increased with lower values of Alb and ALT and higher levels of AST and AP ( Figure 2 ). These associations remained significant after adjustment for potential confounders ( Figure 3 ). The T Bili association with survival was not significant after adjustment. The results were similar for subgroup analyses dichotomizing patients based on clinical setting (i.e., inpatient vs outpatient) and history of ischemic heart disease. Lower Alb was associated with all-cause hospitalization (Q5 vs Q1: hazard ratio 0.41, 95% confidence interval 0.30 to 0.58). However, the associations between the remaining LFTs and all-cause and HF-specific hospitalization were not significant.