Implantable cardioverter–defibrillator (ICD) therapy for primary prevention of sudden cardiac death is not routinely recommended within 90 days of coronary artery bypass grafting (CABG) because of the possibility of an improvement in left ventricular ejection fraction (EF) to>35% after revascularization. We sought to determine the incidence and predictors of EF improvement to >35% after isolated CABG in patients who had a preoperative EF ≤35%. We studied 375 patients who underwent CABG at a tertiary institution and had an echocardiogram preoperatively and postoperatively. Of these, 74 patients (20%) with a preoperative EF ≤35% were included in this analysis. Improvement in EF was defined as postoperative EF >35%. In the overall study population (n = 74), mean EF improved from 28 ± 6% preoperatively to 36 ± 12% postoperatively (p <0.0001). A total of 38 patients (51%) had postoperative improvement in EF to >35% (mean EF in these patients increased from 30 ± 5% to 46 ± 8%; p <0.0001). Patients with EF improvement had a higher preoperative EF than those with no improvement (30 ± 5% vs 26 ± 7%, p <0.005). Improvement in EF was 5 times more likely in patients with preoperative EF 26% to 35% (odds ratio 4.95, 95% CI 1.73 to 14.1; p = 0.003) than those with preoperative EF ≤25%. Other clinical characteristics were not significantly different between patients with versus without EF improvement. In conclusion, more than half of the ICD-eligible patients who underwent CABG improved their EF to >35% after surgery and became ineligible for a primary prevention ICD. EF improvement was unlikely in patients with preoperative EF <25%.
Implantable cardioverter–defibrillator (ICD) therapy for primary prevention of sudden cardiac death (SCD) is not routinely recommended within 90 days of coronary artery bypass grafting (CABG). Instead, it is recommended that patients with preoperative ejection fraction (EF) ≤35% undergo a reassessment of left ventricular (LV) systolic function 90 days after CABG to assess improvement in EF after revascularization. Although it may be reasonable to expect that elimination of ischemia and recovery of hibernating myocardium might improve LV systolic function, the actual evidence that EF improves after CABG and exceeds 35%, obviating implantation of an ICD, is sparse. To address this question, we examined the incidence and predictors of improvement in LV EF to >35% after isolated CABG in patients who were otherwise eligible for primary prevention ICD implantation based on a preoperative EF of ≤35%.
Methods
A total of 2,838 patients underwent isolated CABG at the Minneapolis Veterans Affairs Health Care System from January 1, 2001, to December 31, 2014, and were recorded in our cardiac surgery database. In 375 of these patients, an echocardiogram was performed preoperatively (within 6 months) and postoperatively (within 3 to 24 months) based on clinical indications. Of these 375 patients, we examined 74 patients (20%) who had a preoperative LV EF ≤35%. This study was approved by the Institutional Review Board at the Minneapolis Veterans Affairs Health Care System.
The 2-dimensional echocardiograms were performed by experienced cardiac sonographers and interpreted by board-certified cardiologists experienced in echocardiography. In addition to visual estimation, LV EF was calculated based on the American Society of Echocardiography guidelines for EF quantification. Improvement in LV function was defined as an increase in LV EF to >35% after revascularization.
Continuous and categorical variables are summarized as mean ± SD and frequency (%), respectively. We compared the baseline characteristics of patients with improved postoperative EF (>35%) versus those with unchanged postoperative EF (≤35%) using t test for continuous variables that were normally distributed and Mann–Whitney U test for continuous variables that were non normally distributed. For categorical variables, we used the chi-square test and Fisher’s exact test. We used logistic regression analysis to examine the variables associated with perioperative improvement in EF. We compared the changes in preoperative versus postoperative echocardiographic parameters with paired t test. All p values were 2-sided with a significance of <0.05. Analyses were performed using SPSS, version 19.0 (IBM Corp, Armonk, New York).
Results
Mean age of the 74 patients included in the analysis was 65 ± 9 years. Mean preoperative EF was 28 ± 6% (range 15% to 35%). A total of 63 patients (85%) had a history of myocardial infarction. Patients were on excellent medical therapy for heart failure with reduced EF; with 95% taking a β blocker and 81% taking either an angiotensin-converting enzyme inhibitor or angiotensin-II receptor blocker. Baseline characteristics of the study patients are presented in Table 1 .
| Variable | All patients n=74 | Ejection Fraction | p-value | |
|---|---|---|---|---|
| Improved (>35%) n=38 | Unchanged (≤35%) n= 36 | |||
| Age (years) | 65±9 | 65±9 | 65±9 | 0.97 |
| Men | 100% | 100% | 100% | 1.00 |
| Preoperative left ventricular ejection fraction | 28±6% | 30±5% | 26±7% | <0.005 |
| Prior myocardial infarction | 85% | 82% | 89% | 0.52 |
| Hypertension | 82% | 84% | 81% | 0.77 |
| Diabetes mellitus | 28% | 24% | 33% | 0.36 |
| Atrial fibrillation | 10% | 11% | 8% | 1.00 |
| Chronic kidney disease stage ≥3 | 22% | 16% | 28% | 0.26 |
| Obstructive lung disease | 39% | 40% | 39% | 0.96 |
| Prior stroke | 24% | 21% | 28% | 0.50 |
| Peripheral arterial disease | 45% | 42% | 47% | 0.66 |
| Prior cardiac surgery | 5% | 3% | 8% | 0.35 |
| Laboratory Values | ||||
| Glomerular filtration rate (ml/min/1.73m2) | 86±31 | 92±33 | 80±27 | 0.09 |
| Hemoglobin (g/dL) | 13.6±1.8 | 13.7±1.9 | 13.6±1.7 | 0.97 |
| Perfusion Imaging | ||||
| Infarction | 64% | 61% | 67% | 0.69 |
| Ischemia | 56% | 67% | 40% | 0.21 |
| Viability | 52% | 50% | 54% | 0.86 |
| Medications | ||||
| Beta blocker | 95% | 97% | 94% | 0.62 |
| ACE-inhibitors or Angiotensin receptor blockers | 81% | 89% | 75% | 0.14 |
| Spironolactone | 18% | 14% | 22% | 0.37 |
| Hydralazine and ISDN | 10% | 8% | 11% | 0.71 |
| Digoxin | 20% | 19% | 22% | 0.73 |
| Diuretics | 66% | 60% | 75% | 0.16 |
| Operative Parameters | ||||
| Number of grafts | 2.9±0.8 | 3.0±0.7 | 2.8±0.9 | 0.47 |
| Arterial grafts | 92% | 100% | 83% | 0.01 |
| Complete revascularization | 85% | 90% | 81% | 0.28 |
| Bypass time (minutes) | 123±43 | 123±29 | 124±55 | 0.88 |
| Ischemic time (minutes) | 75±28 | 78±19 | 71±35 | 0.30 |
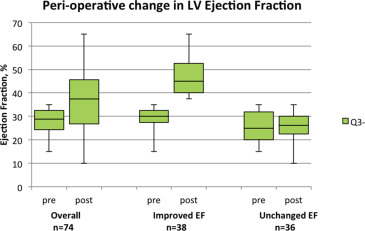
In the overall study population, mean EF improved from 28 ± 6% (range 15% to 35%) preoperatively to 36 ± 12% (range 10% to 65%) postoperatively (p <0.0001; Table 2 ; Figure 1 ). Thirty-eight patients (51%) had postoperative improvement in EF to >35%. In these 38 patients, the mean LV EF increased from 30 ± 5% to 46 ± 8% (p <0.0001; Table 2 ; Figure 1 ). In the other 36 patients (49%), the EF remained unchanged after CABG (26 ± 7% vs 26 ± 7%; p = 0.91).
| Variable | Preoperative ejection fraction | Postoperative ejection fraction | p-value |
|---|---|---|---|
| All patients (n=74) | 28±6% | 36±12% | <0.0001 |
| Ejection fraction improved to >35% (n=38) | 30±5% | 46±8% | <0.0001 |
| Unchanged ejection fraction ≤35% (n=36) | 26±7% | 26±7% | 0.91 |
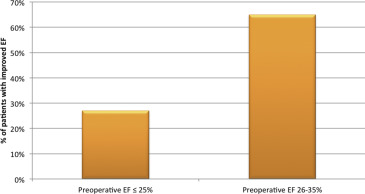
Patients who improved their EF to >35% postoperatively had a higher preoperative EF than those who did not improve their EF to >35% (30 ± 5% vs 26 ± 7%, p <0.005). Improvement in EF to >35% postoperatively was more likely in patients with a preoperative EF of 26% to 35% (n = 48) than those with EF ≤25% (65% vs 27%, p = 0.002; Figure 2 ). Consequently, patients with a preoperative EF of 26% to 35% were 5 times more likely to improve their EF to >35% after CABG (odds ratio 4.95, 95% CI 1.73 to 14.1; p = 0.003) than those with a preoperative EF ≤25%. A total of 44 patients had myocardial perfusion imaging or viability study. Infarct, ischemia, viability, and other clinical characteristics were not significantly different between patients with versus without improvement in EF after CABG ( Table 1 ).