Sudden cardiovascular events account for approximately 45% to 50% of all duty-related deaths among firefighters and a disproportionate number of these fatalities occur after strenuous fire suppression activities. The purpose of this study was to evaluate the effect of acute and chronic aspirin supplementation on hemostatic function before and after live firefighting activities in older firefighters. A double-blind, crossover design included 4 treatments: a 2-week aspirin/placebo treatment (“chronic”) and a single prefirefighting aspirin/placebo treatment (“acute”). Hemostatic function was assessed in 24 male firefighters (mean age = 48.2 ± 5.9 years) immediately before and after 18 minutes of live-fire firefighting activity. An acute bout of firefighting activity significantly decreased platelet aggregation time and decreased activated partial thromboplastin time. Compared with placebo, acute aspirin supplementation resulted in a significant increase in epinephrine closure time, which was further augmented by chronic supplementation. Aspirin supplementation had no effect on coagulatory or fibrinolytic factors. Our findings suggest that an acute bout of firefighting leads to increased coagulatory potential in older firefighters. In conclusion, aspirin supplementation had an antiplatelet effect that decreased platelet aggregability at rest and after an acute bout of firefighting compared with placebo.
Sudden cardiac events are the leading cause of line of duty death among US firefighters, accounting for approximately 45% of line of duty deaths each year. In addition to cardiac fatalities, 600 to 1,000 firefighters suffer nonfatal cardiac events in the line of duty each year. Firefighting activity increases the relative risk of sudden cardiac events 10 to 100 times that of nonemergency station duty. Firefighting may serve as a trigger for sudden cardiac events due to multiple stressors, including strenuous muscular work, emotional/psychological stress, and environmental factors. Advancing age (>45 years), increases the risk of cardiac events during firefighting. Firefighting results in increased body temperature and near-maximal heart rates and leads to a decreased stroke volume, evidence of impaired diastolic function, and increased vascular stiffness. Recent work has also shown that acute firefighting leads to increased platelet aggregability and increased coagulatory potential. However, there are few published data regarding the effect of aspirin on hemostatic balance and a paucity of data on coagulatory responses in older firefighters (>40 years) and firefighters with cardiovascular disease risk factors. The purpose of this study was to determine the effects of acute and chronic aspirin (81 mg) supplementation on hemostatic responses to firefighting activity in firefighters aged >40 years. We hypothesized that both acute and chronic aspirin supplementation would have an antiplatelet effect at rest and that aspirin supplementation would partially offset the procoagulatory changes that occur with firefighting activity.
Methods
Firefighters between the ages of 40 and 60 years were recruited from fire departments across the state of Illinois. Participants were excluded if they had hypertension or heart failure; had any contraindications to aspirin therapy; were currently taking nonsteroidal anti-inflammatory steroids, clopidogrel, or warfarin; or were currently taking aspirin based on physician’s recommendation. All participants received a medical evaluation consistent with National Fire Protection Agency 1582 Standard on Comprehensive Occupational Medical Program for Fire Departments before participation in the study.
This study used a randomized, placebo-controlled, double-blind crossover design to investigate the effects of aspirin administration (acute and chronic) on hemostatic balance of firefighters before and after short-term firefighting activities. Subjects were initially assigned to 1 of 2 conditions: acute aspirin (81 mg enteric aspirin 60 minutes before firefighting) or acute placebo supplementation with a 14- to 60-day washout period between trials. Subjects participated in both conditions; however, the order in which they participated in each was randomized, with the washout period between trials. Subjects then completed the chronic supplementation arm (81 mg/day of enteric aspirin for 14 days or placebo for 14 days) of the study, with aspirin and placebo being applied in random order. Hence, all subjects completed 4 trials: acute aspirin, acute placebo, chronic aspirin, and chronic placebo. Trials were separated by 17.7 ± 7.7 days for the acute protocol and 27.5 ± 3.3 days for the chronic protocol. This study was approved by the University of Illinois Institutional Review Board. All participants signed an informed consent document before participation. The study was registered at ClinicalTrials.gov ( NCT01276691 ).
Subjects reported for testing after a standard meal: Ensure Original Shake (220 cal; 6 g [9%] fat, 33 g [11%] carbohydrates, 10 g [20%] protein), Clif Bar (240 cal; 5 g [8%] fat, 43 g [14%] carbohydrates, 9 g [18%] protein). This meal was ingested with the acute supplement 60 minutes before the trial. All trials were completed at approximately the same time of day to control for diurnal variations in measurements. Participants were instructed to report for testing well hydrated.
For each trial, participants performed prescribed live firefighting drills wearing full personal protective equipment and self-contained breathing apparatus (weight ∼20 kg), in a training structure that contained live fires. The firefighting drills lasted 18 minutes and consisted of 9 2-minute periods of alternating rest and work. The work cycles included stair climbing, simulated forcible entry, a simulated search, and simulated hose advance. Throughout the firefighting drills, trained personnel controlled the temperature in the training structure by adding small fuel packages to the fire sets sequentially and controlling the ventilation conditions in the room. The temperatures at 1.2 m above the floor were maintained at roughly 70°C to 82°C, and the floor temperatures were maintained at approximately 35°C to 41°C.
All participants received a medical evaluation before participation. During this evaluation, cardiovascular risk factors were evaluated and maximal oxygen consumption (expressed in metabolic equivalents) was estimated using a treadmill protocol that required participants to achieve 85% of age-predicted maximal heart rate. Descriptive characteristics were obtained before participating in firefighting drills. Height was measured (to the nearest 0.01 m) using a stadiometer, and body mass was measured (to the nearest 0.5 kg) using a digital beam balance platform. Body mass index was calculated as the body mass in kilograms divided by the height in meters squared. Body temperature was measured continuously throughout the protocol using a monitor and a silicone-coated gastrointestinal core temperature capsule (Mini Mitter, VitalSense; Philips Respironics, Bend, Oregon). Participants swallowed a small disposable core temperature sensor capsule 6 to 12 hours before the study was conducted. Heart rate was measured using a heart rate monitor (Vantage XL; Polar Electro, Inc., Lake Success, New York).
Venous samples were drawn before and after firefighting activity from the antecubital vein using a 21-gauge needle by a trained phlebotomist. Platelet count was assessed at a local clinic from venous whole blood as part of a complete blood count analysis, using the electrical impedance method (with an instrument such as the COULTER LH 700 Series; Beckman Coulter, Inc., Fullerton, California). Platelet function was assessed by epinephrine (EPI)-induced and adenosine 5′-diphosphate (ADP)–induced platelet aggregability using a platelet function analyzer (PFA-100; Dade Behring, Deerfield, Illinois). Blood samples were collected in a Vacutainer containing 3.2% sodium citrate, maintained at room temperature and analyzed within 2 hours of collection. Blood was pipetted (800 μl) into the disposable cartridges and then aspirated under high shear rates (5,000 to 6,000 second −1 ) through an aperture cut into the membrane coated with collagen and ADP and a membrane coated with collagen and EPI. Time to occlusion was reported.
Blood samples were collected in tubes containing 3.2% sodium citrate for measurements of all coagulation and fibrinolytic factors, except for the assessment of tissue plasminogen activator (t-PA) activity, for which samples were drawn into Stabilyte tubes (Biopool, Wicklow, Ireland). All samples were centrifuged at 2,300 rpm for 25 minutes at 4°C with the plasma removed and placed into aliquots and stored at −70°C for later analysis. All coagulatory and fibrinolytic variables from all subjects were batch processed at a contracted clinical laboratory (LabCorp). Fibrinogen was analyzed through the Clauss method within 14 days of blood collection and preparation. Plasminogen activator inhibitor (PAI-1) activity and antigen and t-PA antigen were analyzed using an enzyme-linked immunosorbent method. t-PA antigen activity was analyzed in duplicate using a chromogenic technique. Activated partial thromboplastin time (aPTT) was analyzed using clotting time comparisons with similarly treated plasma controls.
Statistical analyses were performed using STATA statistical software (Release 13; StataCorp LP, College Station, Texas). All tests of significance used 2-tailed alpha = 0.05. Tests of statistical assumptions preceded hypotheses testing, and appropriate statistical adjustments were made to correct for violations. Given the completely within-subjects experimental design, with all subjects participating in all conditions, and repeated observations before and after firefighting, we analyzed our study outcomes using mixed-effects linear regression methods (commonly referred to as hierarchical linear models or multilevel model methods). These are recent extensions to repeated-measures analysis of variance and have the added advantage of the ability to incorporate missing data and/or heterogeneous effects among subjects. We did experience occasional missing observations in this experiment although heterogeneous effect terms (i.e., random slopes) were not necessary for any of our outcomes. Therefore, we evaluated the effects of a drug intervention (aspirin vs placebo), supplementation timeframe (acute vs chronic), and firefighting activities (prefirefighting vs postfirefighting) in fully factorialized mixed-effects models with fixed beta coefficients evaluating the main effects and interactions among these terms, and random intercepts to incorporate the within-subjects experimental design. Data are presented as mean ± standard error in figures and mean ± SD or frequency in text and tables.
Results
The average participant age was 48.2 ± 5.9 years. Total mean cholesterol was in the borderline high range; mean low-density lipoprotein cholesterol was in the borderline high range; and mean high-density lipoprotein cholesterol was in the average range. Table 1 presents descriptive characteristics of study participants, whereas Table 2 provides cardiovascular disease risk factor distributions of participants. Nine of the firefighters were obese based on body mass index standards.
| Variable | Mean±SD | Range |
|---|---|---|
| Age (years) | 48.2±5.9 | 40–59 |
| Height (m) | 1.83±5.8 | 1.73–1.96 |
| Weight (kg) | 94.3±13.8 | 72.7–118.2 |
| Body mass index (kg·m -2 ) | 28.2±3.5 | 21.4–36.6 |
| Waist circumference (cm) | 100±11 | 83–123 |
| Systolic blood pressure (mmHg) (n=20) | 127±12 | 106–154 |
| Diastolic blood pressure (mmHg) (n=20) | 81± 9 | 62–94 |
| Resting heart rate (bpm) (n=20) | 70±10 | 57–96 |
| Maximal oxygen uptake (metabolic equivalents) (n=22) | 11.8±2.7 | 7–17.7 |
| Total cholesterol (mg·dL -1 ) (n=22) | 201±36 | 109–287 |
| Low-density lipoprotein cholesterol (mg·dL -1 ) (n=21) | 129±34 | 52–206 |
| High-density lipoprotein cholesterol (mg·dL -1 ) (n=21) | 47±12 | 30–77 |
| Risk Factor | Frequency ( n (%)) |
|---|---|
| Body mass index (kg·m -2 ) ∗ | |
| 18.5−24.9 | 5 (22%) |
| 25.0−29.9 | 9 (39%) |
| ≥ 30 | 9 (39%) |
| Total cholesterol (mg·dL -1 ) (n=22) † | |
| < 200 | 11 (50%) |
| 200−239 | 9 (41%) |
| ≥ 240 | 2 (9%) |
| Low density lipoprotein (mg·dL -1 ) (n=21) † | |
| < 100 | 4 (19%) |
| 100−129 | 6 (29%) |
| 130−159 | 7 (33%) |
| 160−189 | 3 (14%) |
| ≥ 190 | 1 (5%) |
| High density lipoprotein (mg·dL -1 ) (n=21) † | |
| < 40 | 8 (38%) |
| 40−59 | 10 (48%) |
| ≥ 60 | 3 (14%) |
| Physical activity ‡ | |
| Does not meet physical activity guidelines | 18 (78%) |
| Meets/Exceeds physical activity guidelines | 5 (22%) |
| Smoker | 3 (13%) |
| Family history of cardiovascular disease (n=22) § | 1 (5%) |
∗ Classification based on established categories.
† Classification based on established criteria.
‡ Physical activity guidelines: 30 to 60 minutes/day (150 minutes/week) of purposeful moderate exercise, or 20 to 60 minutes/day (75 minutes/week) of vigorous exercise, or a combination of moderate and vigorous exercise.
§ Immediate family member died of cardiovascular incident before 45(men)/55(women).
Firefighting activity resulted in a significant increase in heart rate, reaching a mean peak heart rate of 172 ± 12 beats/min during the firefighting evolution (p <0.001). Firefighting activity also resulted in a significant increase (1.08 ± 0.38°C) in core body temperature (p <0.001). In addition, we observed a small (0.21 ± 0.37°C) but significantly higher core body temperature during the acute supplementation phase of the study compared with the chronic supplementation (p <0.01). Although not reaching traditional levels of statistical significance (p <0.06), we detected a slightly greater increase in core temperature after firefighting with chronic aspirin supplementation (+1.12 ± 0.29°C) compared with acute aspirin supplementation (+0.89 ± 0.25°C).
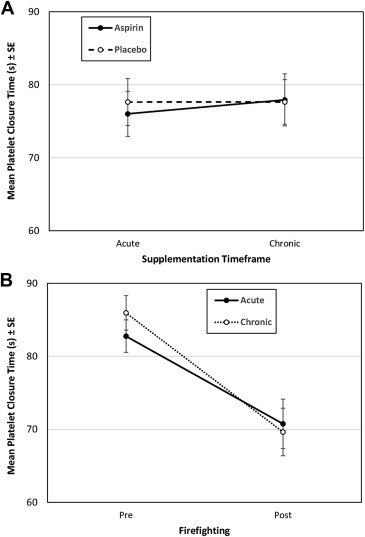
Platelet closure time after firefighting was significantly faster for blood stimulated with ADP (p <0.001) and EPI (p <0.001). ADP closure time decreased after firefighting but was not affected by drug intervention or supplementation timeframe, nor were there any significant interactions ( Figure 1 ). However, in addition to the firefighting main effect, EPI closure time was also significantly affected by drug intervention (p <0.001) and supplementation timeframe (p <0.001) with an increased closure time for the aspirin intervention (vs placebo) and for the chronic timeframe (vs acute; Figure 2 ). In addition, we observed a significant supplementation by drug interaction on EPI closure time (p <0.001), whereby the mean EPI closure time was much higher with aspirin relative to placebo in chronic supplementation conditions, relative to virtually no difference between aspirin and placebo in the acute supplement conditions.