Introduction
Over the last three decades, major advances have occurred in the treatment of patients with ST elevation myocardial infarction (STEMI) that have significantly enhanced our knowledge and understanding. A commensurate improvement in outcomes has ensued. Despite this burgeoning knowledge and a multi-pronged investment in both the content and process of STEMI care, important care gaps exist. These include a significant proportion of patients not treated with reperfusion therapy, inadequate patient triage, delayed time to reperfusion, suboptimal utilization of appropriate adjunctive medical therapy, subsequent underutilization of cardiac rehabilitation programs, and failure to undertake lifestyle modifications.
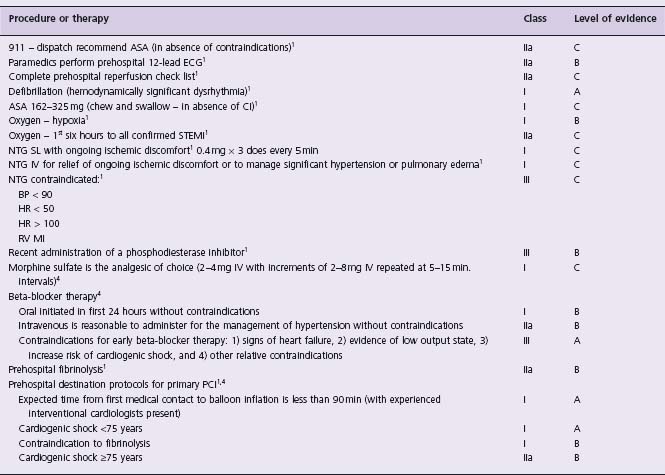
Time to initiation of reperfusion remains a critical factor pivotal to modulating STEMI patient outcomes. Clinical evidence and guidelines have defined key parameters necessary to achieve optimal time to reperfusion once patients establish first medical contact.1–3 In Figure 30.1 the specific temporal segments are outlined and include time from medical presentation to acquisition of the first 12-lead ECG, first ECG until completion of patient assessment and confirmation of diagnosis, and time from diagnosis to reperfusion therapy. Contemporary STEMI guidelines indicate that time from first medical contact to initiation of fibrinolysis should be 30 minutes or less and within 90 minutes to first balloon inflation in the case of mechanical reperfusion,1,2,4
Rich and often unrealized opportunities exist, prior to arrival at hospital, to limit STEMI patient morbidity and mortality by enhancing early management via the prehospital emergency medical system (EMS). The initial early activation of EMS depends upon appropriate recognition of symptoms or circumstances, which must be coupled with timely and appropriate responses from affected individuals, often assisted by family members, friends, co-workers or bystanders. Unfortunately, utilization of EMS remains suboptimal with many STEMI patients presenting to the hospital using personal transportation. Despite dedicated public education strategies, little impact on this behavior has ensued. Advanced prehospital STEMI management which expedites patient assessment, diagnosis, triage, and treatment has been successful in various health systems worldwide, including over two decades of experience in France and Ireland. These prehospital STEMI treatment protocols are most effective when operating within an integrated system-wide regional reperfusion program which includes continuous quality improvement.
The American College of Cardiology (ACC) and American Heart Association (AHA) guidelines, with a current focused update, have encouraged the reduction of total ischemic time to less than two hours.1,2,4 Unfortunately it has been consistently demonstrated that patient delay in seeking medical attention is the major limitation to realizing this goal and time to reperfusion remains suboptimal. Within clinical trials greater than 50% of reperfusion delay occurs prior to first medical contact; an even longer delay is evident within “real-world” registry data.5–8 Addressing patient delay requires understanding the patient’s perception, interpretation, and action as well as the influence of other factors modulating behaviors (Fig. 30.2).
Figure 30.1 Understanding time to treatment: pharmacologic and mechanical reperfusion. Understanding process of care and associated temporal delay required to deliver reperfusion therapy facilitates healthcare providers’ ability to achieve goal times and develop appropriate systematic interventions. Upon arrival in the catheterization laboratory the patient is prepared for the procedure and the interventional cardiologist achieves arterial access and undertakes diagnostic coronary angiography. If the anatomy is consistent with PCI, appropriate equipment is prepared and anticoagulant therapy administered prior to crossing the specific lesion and achieving first balloon inflation; the total process typically requires 30 minutes. Therefore, it is essential that systematic interventions are implemented to expedite activation of the interventional cardiologist and catheterization laboratory personnel as well as patient transportation from the emergency department such that the time from confirmed diagnosis to arrival in the laboratory is abbreviated to 40 minutes or less.
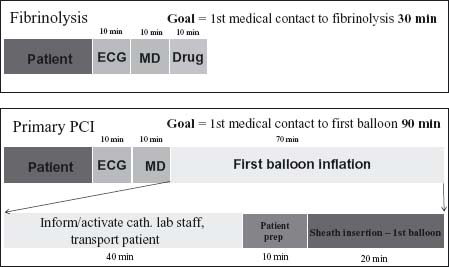
Figure 30.2 Understanding time to reperfusion – patient delay. When a person perceives a novel or recurrent sensation (such as chest pressure) their interpretation is influenced by the severity of the symptom as well as a host of factors influenced by past experience and education. Seeking advice from friends, family, co-workers or bystanders regarding the interpretation of the symptom as well as appropriate action required may occur. Education influences the personal interpretation of symptoms and appropriate action as well as the advice that may be offered from others.
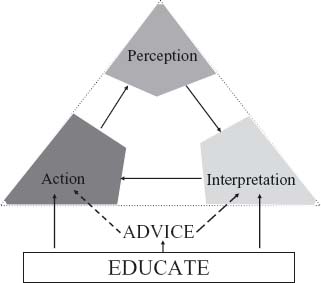
Table 30.1 Demographic factors associated with patient delay
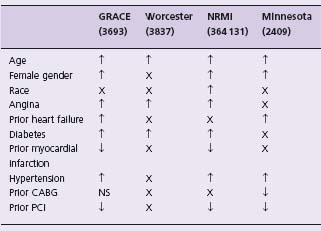
CABG, coronary artery bypass grafting; PCI, percutaneous coronary intervention; ↑, factor associated with increased delay from symptom onset to medical presentation; ↓, factor associated with decreased delay; NS, no significant relationship demonstrated; X, factor not reported.
Table 30.2 Situational factors associated with patient delay
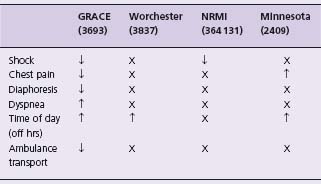
↑, factor associated with increased delay from symptom onset to medical presentation; ↓, factor associated with decreased delay; NS, no significant relationship demonstrated; X, factor not reported.
Specific patient demographic factors have been identified which affect the duration of symptoms prior to seeking medical advice (Table 30.1). Older patients and women have consistently been shown to delay seeking medical attention until later in the course of their symptoms.8–11 Ironically, patients with known past medical diagnoses with increased risk of cardiovascular events have also prolonged delay, including those with prior angina, hypertension, diabetes mellitus, and congestive heart failure.8–11 Patients with prior percutaneous coronary revascularization and prior acute myocardial infarction appear to present after less symptomatic delay.8,9,11
A host of situation-specific factors have also been shown to modulate time from symptom onset to medical presentation (Table 30.2). The most consistent of these are linked to severity of symptoms at presentation, especially those of cardiogenic shock or resuscitated arrhythmia presenting earlier.8,9 Longer delays in presentation also occur outside regular working hours or on weekends and holidays.8,10,11
Psychosocial factors also influence patient delay. These include misinterpretation of symptoms and denial of their importance. Female STEMI patients are known to deny or misinterpret their symptoms since they are conditioned to interpret acute myocardial infarction as a “male” disease.8,9,11–13 There are also significant socioeconomic factors related to the cost of healthcare, particularly activation of the prehospital EMS which has additional associated cost implications in many countries.14
Remarkably, in industrialized nations, only 50% of patients with symptoms suggestive of acute myocardial infarction activate the prehospital EMS. This figure is staggering and tragic considering the evidence indicating that ambulance assistance leads to shortened time to definitive care and diminishes the potential individual patient and population hazards with self-transportation of patients at risk of hemodynamic compromise and dysrhythmia.
Although they are logical, dedicated educational programs that have attempted to increase appropriate utilization of EMS and decrease reperfusion delay through enhanced patient response have typically met with limited success (Table 30.3). Within the United States, the Rapid Early Action for Coronary Treatment (REACT) trial randomized 20 cities, matched for community size and patient demographics, to receive an 18-month educational intervention.15 The premises of this program were that: (1) time to treatment was currently excessive; (2) patient response accounted for the majority of delay; and (3) dedicated community educational intervention would improve knowledge and decrease patient-related delay. Central educational themes were promulgated, aimed at early symptom recognition and rapid response by calling 911 if symptoms suggestive of myocardial ischemia persisted for more than 15 minutes. This interventional strategy focused on: (1) community organizations including health professionals and other leaders; (2) public education to develop general awareness of acute myocardial infarction symptoms, the presence of heart disease in females, and appropriate action through MI survival plans, bystander response, and the importance of calling 911; (3) professional education including focused discussions with physicians, nurses, cardiac rehabilitation, emergency department and ambulance staff through academic detailing, continuing health education events and special seminars; and (4) education of patients with a past history of coronary artery disease or significant cardiovascular disease risk factors. Each community involved in these programs had a local office with two staff to organize events and promote the program. Despite enhancing awareness and increasing utilization of EMS, this intensive educational program, which was associated with an annual cost between $156 000 and $294 000 per 100 000 person community, did not demonstrate a reduction from symptom onset to first medical presentation in STEMI patients.15,16 Paradoxically greater utilization of EMS occurred in patients with symptoms determined to be non-cardiac.
Table 30.3 Systematic review of interventions to reduce delay in patients with suspect AMI
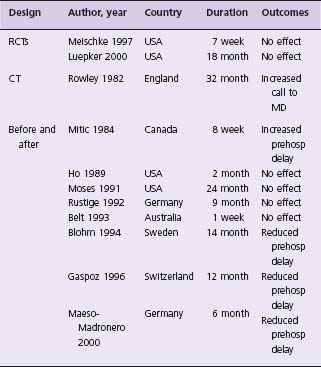
RCTs, randomized controlled trial; CT, controlled trial; Before and after, analysis prior to and following the intervention.66
Although these results are discouraging and highlight the limitation of current educational strategies to reduce patient treatment delay, enhancing awareness of those with established disease or other risks remains a legitimate goal. Future campaigns to shorten patient delay are likely to be more effective if they address psychosocial and behavioral impediments to action, are sustained rather than short term, and focus on those patients and families at highest risk, including those with known coronary heart disease.
Prehospital diagnosis of ST elevation myocardial infarction
During the acute phase of STEMI, patients may experience a diverse range of symptoms varying from classic crushing retrosternal chest discomfort with typical associated symptoms, to isolated dyspnea, syncope, malaise, and neurologic impairment. In elderly patients, females, diabetics, and those taking non-steroidal anti-inflammatory drugs (NSAIDs), symptoms may be subtle or absent and such patients are known to be at increased risk of suffering “silent myocardial infarctions”.17–22 This reality makes recognition of patients with STEMI challenging for frontline medical personnel in emergency departments as well as in the prehospital environment.
EMS programs typically have a system of triage to be implemented at the time of a 911 call, which are based upon key symptoms communicated from patients or their families, including chest discomfort, shortness of breath, syncope, and other indicators of potential myocardial ischemia. In some centers, this involves physician participation to prioritize prehospital response to appropriate patients with mobilization of advance care mobile intensive care units. In other regions where prehospital care is delivered by non-physician paramedical staff, preliminary triage may also be undertaken to facilitate the activation of advanced cardiac life support (ACLS) units capable of delivering advanced prehospital cardiac care.
On arrival at a scene where symptoms compatible with myocardial infarction are recognized or confirmed, rapid completion of a prehospital 12-lead ECG is a key factor in determining diagnosis and guides subsequent therapy. It has been shown that prehospital 12-lead ECGs can be expeditiously completed with reliable lead placement and provide high-quality diagnostic tracings.23,24 Furthermore, provision of a prehospital 12-lead ECG adds little incremental prehospital delay, i.e. a 1–10 minute increase in prehospital on-scene time.24–27
Various approaches to 12-lead ECG interpretation have been employed within the prehospital environment. When an experienced physician is present, onsite interpretation is feasible; if not, opportunities exist for either ECG remote transmission for physician interpretation or computer-assisted interpretation by paramedical staff. Evidence demonstrates that well-trained paramedics can efficiently use the 12-lead ECG to guide early treatment. Although this has been proven effective in a research environment, more widespread implementation carries the potential for over-, under- and inappropriate diagnosis of STEMI, and robust evaluations of the success of such programs are warranted.
Remote prehospital 12-lead ECG interpretation requires appropriate technology at both ends of the transmission, the immediate availability of an experienced physician, and a system of communication between the physician and prehospital paramedics with the attendant liability of system failure at multiple levels. Transmission of all prehospital 12-lead ECGs for remote interpretation is impractical given that only about 5% of such patients, i.e. those identified with symptoms possibly related to myocardial infarction, have confirmed evidence of STEMI.28 Preliminary paramedic ECG interpretation has been effectively employed in several regions for selective transmission of the prehospital 12-lead ECG. In a single-center analysis, greater than 70% of all STEMI patients were correctly identified by prehospital paramedic teams following modest training in STEMI patient identification and 12-lead ECG interpretation.22 Even within the setting of a prehospital fibrinolysis trial, where stringent inclusion and exclusion criteria are employed, paramedic EMS staff correctly identified and enrolled 46% of all STEMI patients.
In conjunction with completion of the prehospital 12-lead ECG, prehospital paramedical staff can effectively and thoroughly complete prehospital reperfusion checklists to determine eligibility for reperfusion. Thereafter, prehospital reperfusion can be administered or patients can be triaged to centers capable of achieving expedited mechanical or pharmacologic reperfusion.
Prehospital management of ST elevation myocardial infarction
In patients with a likely or confirmed diagnosis of STEMI, implementation of contemporary guidelines should be considered prior to hospital arrival to minimize patient distress, morbidity, and mortality, especially those with demonstrated time dependency (Table 30.4)1,2,4 Prehospital EMS teams managing patients with STEMI should be capable of advanced cardiac life support techniques to address hemodynamic and electrical instability as well as respiratory compromise. Synchronized cardioversion, defibrillation or percutaneous pacing can be employed to treat malignant arrhythmias. In the setting of symptomatic hypotension, intravenous fluid resuscitation is standard and intravenous inotropes can be administered when appropriate medical supervision exists.
Oxygen and respiratory support
Supplemental oxygen is administered to patients with oxygen saturation less than 90%. There is experimental evidence that oxygen administration may limit ischemic myocardial injury; therefore even in uncomplicated myocardial infarction this may be an effective strategy.29 It has become ubiquitous to administer oxygen to virtually all patients with symptoms suggestive of myocardial ischemia.
In patients with cardiopulmonary compromise, such as pulmonary edema, severe congestive heart failure, cardiogenic shock or presumed mechanical complications of STEMI, advanced respiratory support may be required. This may include bag, valve and mask with oral airway or endotracheal intubation to provide adequate oxygenation and ventilation.
Analgesia
It is the expectation that patients with STEMI will receive reperfusion therapy although not all will be candidates; continuing pain relief is required in either case. Although retrospective data have raised concerns about potential adverse events from morphine in patients with non-STEMI, this has not been the case with STEMI patients.30 Therefore, administration of morphine sulfate (2–4mg IV with increments of 2–8 mg IV repeated at 5–15 minute intervals) is the analgesic of choice for management of pain associated with STEMI. This should be undertaken judiciously in patients with hemodynamic or respiratory instability.
In the STEMI patient population treated within the EXTRACT TIMI 25 trial, an increased risk of death, reinfarction, heart failure or shock was demonstrated in those taking NSAIDs within seven days of enrollment.31
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree