The aim of the study was to assess the clinical and prognostic impact of early functional mitral regurgitation (FMR) improvement on the outcome of patients with idiopathic dilated cardiomyopathy (IDC). The prevalence and prognostic role of FMR improvement, particularly at early follow-up, in patients with IDC are still unclear. From 1988 to 2009, we enrolled 470 patients with IDC with available FMR data at baseline and after 6 ± 2 months. According to the evolution of FMR, patients were classified into 3 groups: stable absent-mild FMR, early FMR improvement (downgrading from moderate-severe to absent-mild), and persistence/early development of moderate-severe FMR. At baseline, 177 of 470 patients (38%) had moderate-severe FMR. Patients with early FMR improvement had significantly better survival rate—free from heart transplant with respect to those with persistence/early development of moderate-severe FMR (93%, 81%, and 66% vs 91%, 64%, and 52% at 1, 6, and 12 years, respectively; p = 0.044). At 6-month follow-up multivariate analysis, FMR improvement was associated with better prognosis (hazard ratio 0.78, 95% confidence interval [CI] 0.64 to 0.96, p = 0.02); the other independent predictors were male gender, heart failure duration, and early re-evaluation of the New York Heart Association class and left ventricle systolic function. This model provided more accurate risk stratification compared with the baseline model (Net Reclassification Index 80% at 12 months and 41% at 72 months). In conclusion, in a large cohort of patients with IDC receiving optimal medical treatment, early improvement of FMR was frequent (53%) and emerged as a favorable independent prognostic factor with an incremental short- and long-term power compared with the baseline evaluation.
Functional mitral regurgitation (FMR) is a common finding in patients with heart failure and left ventricular (LV) dysfunction and is independently associated with a poor prognosis.
Idiopathic dilated cardiomyopathy (IDC) is a primary myocardial disease characterized by LV dilation and systolic dysfunction without known causes that commonly leads to heart failure.
Improvement of FMR in response to pharmacological therapy and cardiac resynchronization has been previously demonstrated. Frequently, it starts in the early phases of the disease and thereafter in concomitance with favorable LV reverse remodeling. However, the impact of its early reduction on outcome in IDC setting has not been previously investigated. Our aims were (a) to investigate the effect of optimal medical therapy on FMR at early follow-up and (b) to evaluate the impact of early FMR improvement in the prognostic stratification of patients with IDC under optimal medical treatment.
Methods
From January 1988 to December 2009, patients with IDC consecutively enrolled in the Heart Muscle Disease Registry of Trieste with available baseline, and early follow-up (6 ± 2 months) data were included in the study. All patients underwent a structured follow-up (6 months after enrollment and then annually), ending at the time of last contact, death, or urgent heart transplantation. Informed consent was obtained under the institutional review board policies of hospital administration. Information regarding the end points was obtained from the patients, their physician, or the registers of death of the municipalities of residence. The diagnosis of IDC was determined according to the World Health Organization criteria. A complete clinical and laboratory evaluation was performed at baseline and early follow-up. Significant coronary artery disease was excluded with coronary angiography. Until 1996, endomyocardial biopsy was routinely performed to exclude active myocarditis; thereafter, it was reserved to patients with anamnestic or clinical suspicion of active myocarditis. Patients with organic mitral disease, active myocarditis, significant coronary artery disease (stenosis >50% of a major coronary artery), history of severe systemic hypertension (>160/100 mm Hg), excessive alcohol intake (>100 g/d), other severe organic valve diseases, and systemic diseases affecting short-term prognosis were excluded.
After enrollment, if indicated, all patients received angiotensin-converting enzyme inhibitors/angiotensin receptors blockers and β blockers treatment titrated to the higher tolerated dose. Daily dosages were reported as equivalents of enalapril and carvedilol, respectively (enalapril-equivalent dosages: captopril/3.75, ramipril × 4; carvedilol-equivalent dosages: metoprolol/2, bisoprolol × 10), and referred to the end of titration period. In 1998, implantable cardioverter defibrillator was introduced for primary prevention of sudden cardiac death in high-risk patients (persistent LV ejection fraction ≤35% and New York Heart Association [NYHA] function II to III despite optimal medical therapy). Cardiac resynchronization therapy in our center started in 2005 in patients with conventional indications (persistent LV ejection fraction ≤35%, left bundle branch block, and NYHA class ≥2) on optimal medical treatment, according to available evidences.
M-mode, 2-dimensional, and Doppler echocardiographic studies were performed at baseline, after clinical stabilization, and at 6 months follow-up. Systolic and diastolic functions were evaluated according to international guidelines. Specifically, LV volumes and LV ejection fraction were calculated by Simpson’s biplane method, and left atrial size was assessed by end-systolic left atrial area. All measurements were indexed according to body surface area. FMR was assessed using a multiparametric approach: quantification of vena contracta width at Color flow Doppler and the jet area. The assessment of the effective regurgitant orifice area measured by the proximal isovelocity surface area, whenever feasible, has been considered the preferred method for FMR quantification since its evaluation started in our Center in 2008.
FMR was graded as moderate-severe by an effective regurgitant orifice area ≥20 mm 2 and/or a vena contracta width >3 mm or a jet area of at least 4 cm 2 in patients without available effective regurgitant orifice area measurement. All measurements were obtained from the mean of 3 (patients in sinus rhythm) or 5 beats (atrial fibrillation). Early clinical and echocardiographic re-evaluation was performed 6 ± 2 months after enrollment. “FMR improvement” was defined as FMR downgrading from moderate-severe to absent-mild at early follow-up. Primary prognostic outcome measures were death and urgent (status I) heart transplantation.
Summary statistics of clinical and instrumental variables were expressed as mean and SD or count and percentage, as appropriate. For continuous parameters, repeated measures from baseline to 6 months follow-up were compared by means of paired t test or Wilcoxon, and the differences across groups determined by FMR evolution by the analysis of variance or Mann-Whitney test. McNemar test was used to compare repeated binary measures, and the chi-square test was calculated between groups determined by FMR evolution. Univariate and multivariate logistic regression models were estimated to find baseline predictors of early FMR improvement in the subgroup with moderate-severe FMR at baseline. Survival Kaplan-Meier curves according to baseline FMR and FMR evolution were calculated and subsequently compared with the log-rank test. Two Cox models were estimated to evaluate the additive prognostic role of FMR evolution with reference to known predictors of outcome: one including these variables (i.e., gender, duration of heart failure, NYHA class III to IV, LV ejection fraction, and moderate-severe FMR), the second including also NYHA class and LV ejection fraction at early follow-up, plus FMR evolution. Follow-up started at 6 months evaluation. The Net Reclassification Index (continuous version, category less) for survival data was calculated to assess the true discriminatory potential of FMR evolution. To evaluate how long early FMR evolution could add prognostic improvement, Net Reclassification Index values were computed at 12, 24, 48, 72, 96, and 120 months, and confidence intervals were calculated using the bootstrap technique. All results were considered statistically significant when p <0.05. The entire analysis was performed using the SPSS package, version 19 (IBM, Chicago, Illinois), and the R statistical software, version 2.14.1 (R Core Team [2013], R Foundation for Statistical Computing, Vienna, Austria).
Results
Four-hundred seventy patients met inclusion criteria. Baseline characteristics are presented in Table 1 . Overall, patients presented significant LV remodeling at enrollment. Moderate-severe FMR was present in 38% of the study cohort. At the time of referral, 45% and 16% of patients were respectively treated with angiotensin-converting enzyme inhibitors/angiotensin receptors blockers and β blockers. Medical treatment was optimized after first evaluation in most of the patients.
| Baseline (n=470) | Follow-up (n=470) | P | |
|---|---|---|---|
| Age (years) | 45±14 | – | – |
| Male sex | 322 (70 %) | – | – |
| Median Heart Failure Duration (months) | 4.0 (1.0;12.0) | – | – |
| Systolic Blood Pressure (mmHg) | 124±16 | 125±17 | 0.280 |
| Diastolic Blood Pressure (mmHg) | 79±11 | 78±10 | 0.032 |
| Heart rate (bpm) | 78±15 | 69±12 | <0.001 |
| NYHA III-IV | 121 (26%) | 36 (8%) | <0.001 |
| Creatinine (mg/dl) | 1.1±0.2 | 1.1±0.2 | 0.505 |
| Sinus rhythm | 371 (91%) | 420 (91%) | 0.845 |
| Left Bundle Branch Block | 159 (34%) | 126 (31%) | 0.087 |
| Left Ventricular Ejection Fraction (%) | 30±10 | 39±11 | <0.001 |
| Left Ventricular End Diastolic Diameter Index (mm/m 2 ) | 36±17 | 34±6 | 0.001 |
| Left Ventricular End Systolic Diameter Index (mm/m 2 ) | 30±13 | 27±6 | <0.001 |
| Left Ventricular End Diastolic Volume Index (ml/m 2 ) | 101±38 | 89±34 | <0.001 |
| Left Ventricular End Systolic Volume Index (ml/m 2 ) | 73±34 | 57±31 | <0.001 |
| Left Atrial Area Index (cm 2 /m 2 ) | 13.7±4.2 | 12.4±3.7 | <0.001 |
| Moderate-Severe Functional Mitral Regurgitation | 177 (38%) | 110 (23%) | <0.001 |
| Restrictive Filling Pattern | 114 (27%) | 47 (11%) | <0.001 |
| Beta-blockers | 76 (16%) ∗ | 408 (87%) | <0.001 |
| Carvedilol Equivalent Dose (mg/die) | 54±21 | 57±24 | 0.546 |
| Angiotensin Converting Enzyme Inhibitors-Angiotensin Receptor Blockers | 212 (45%) ∗ | 432 (92%) | <0.001 |
| Enalapril Equivalent Dose (mg/die) | 20±10 | 22±11 | 0.478 |
| Aldosterone Receptor Antagonists | Na | 23 (5%) | – |
| Diuretics (%) | 312 (71%) ∗ | 179 (38%) | <0.001 |
| Digitalis (%) | 334 (71%) ∗ | 160 (34%) | <0.001 |
| Implantable Cardioverter-Defibrillator † (%) | 102 (22%) | ||
| Cardiac Resynchronization Therapy † (%) | 38 (8%) |
At early re-evaluation (6 ± 2 months), the overall population improved in terms of symptoms and showed a significant LV reverse remodeling. FMR degree, prevalence of restrictive filling pattern, and also the left atrial size significantly decreased; 16 patients (2% of all patients enrolled in the Heart Muscle Disease Registry in the study period) died within 6 months. As expected, they were characterized by a more compromised clinical and instrumental condition ( Supplementary Table 1 ).
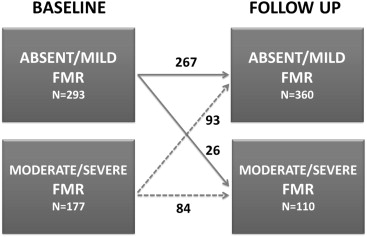
Among the whole population, 267 patients (57%) presented absent-mild FMR both at baseline and early re-evaluation; 93 (20%) improved FMR degree (53% of patients with moderate-severe FMR at enrollment) and 110 (23%) presented moderate-severe FMR at follow-up ( Figure 1 ).
Baseline and follow-up characteristics of patients according to early FMR evolution are listed in Table 2 . At baseline, patients with early improvement of FMR were similar to patients with moderate-severe FMR at 6 months. Conversely, patients with stable absent-mild FMR were probably diagnosed in a more initial stage of the disease, as expressed by the shorter symptoms duration, less advanced functional class, less dilated LV and left atrium, higher LV ejection fraction, and lower prevalence of restrictive filling pattern and left bundle branch block.
| Stable absent- mild FMR (n=267) | Early FMR Improvement (n=93) | Persistence/early development of moderate-severe FMR (n=110) | p ∗ | |
|---|---|---|---|---|
| BASELINE | ||||
| Age (years) | 44±14 | 47±13 | 48±14 | 0.052 |
| Male sex | 200 (75%) | 65 (70%) | 65 (59%) | 0.009 |
| Median Heart Failure Duration (months) | 3.0 (1-10.5) | 3.0 (1-13.7) | 5.0 (2-18) | 0.046 |
| Systolic Blood Pressure (mmHg) | 126±16 | 123±16 | 121±16 | 0.048 |
| Diastolic Blood Pressure (mmHg) | 80±10 | 81±11 | 78±11 | 0.419 |
| Heart Rate (bpm) | 76±14 | 83±16 | 80±16 | 0.001 |
| NYHA III-IV | 45 (18%) | 33 (37%) | 38 (36%) | <0.001 |
| Sinus Rhythm | 209 (92%) | 75 (90%) | 87 (88%) | 0.451 |
| Left Bundle Branch Block | 65 (29%) | 32 (41%) | 39 (40%) | 0.014 |
| Left Ventricular Ejection Fraction (%) | 34±10 | 25±8 | 28±9 | <0.001 |
| Left Ventricular End Diastolic Diameter Index (mm/m 2 ) | 34±5 | 38±5 | 38±7 | <0.001 |
| Left Ventricular End Systolic Diameter Index (mm/m 2 ) | 27±5 | 33±5 | 32±6 | <0.001 |
| Left Ventricular End Diastolic Volume Index (ml/m 2 ) | 89±31 | 118±41 | 117±40 | <0.001 |
| Left Ventricular End Systolic Volume Index (ml/m 2 ) | 60±27 | 91±38 | 86±36 | <0.001 |
| Left Atrial Area Index (cm 2 /m 2 ) | 12.0±3.2 | 15.7±4.2 | 15.9±4.8 | <0.001 |
| Restrictive Filling Pattern | 25 (12%) | 40 (53%) | 39 (43%) | <0.001 |
| Beta-blockers † | 45 (17%) | 15 (16%) | 16 (15%) | 0.206 |
| Carvediolol Equivalent dose (mg/d) | 56±23 | 54±20 | 54±22 | 0.368 |
| ACE-inhibitors/ARBs † | 122 (46%) | 42 (45%) | 46 (42%) | 0.982 |
| Enalapril Equivalent dose (mg/d) | 22±12 | 20±9 | 21±10 | 0.432 |
| Aldosterone Receptor Antagonists † | na | na | Na | – |
| Diuretics † | 136 (51%) | 72 (77%) | 86 (78%) | <0.001 |
| Digitalis † | 141 (53%) | 53 (84%) | 88 (80%) | <0.001 |
| FOLLOW-UP | ||||
| Systolic Blood Pressure (mmHg) | 126±15 | 128±19 | 121±16 | 0.017 |
| Heart Rate (bpm) | 64±10 | 66±14 | 70±14 | <0.001 |
| NYHA III-IV | 8 (3%) | 4 (4%) | 24 (23%) | <0.001 |
| Sinus Rhythm | 211 (94%) | 74 (89%) | 84 (85%) | 0.052 |
| Left Bundle Branch Block | 61 (27%) | 28 (35%) | 37 (37%) | 0.125 |
| Left Ventricular Ejection Fraction (%) | 42±10 | 37±11 | 33±10 | <0.001 |
| Left Ventricular End Diastolic Diameter Index (mm/m 2 ) | 32±5 | 34±7 | 37±6 | <0.001 |
| Left Ventricular End Systolic Diameter Index (mm/m 2 ) | 24±6 | 28±6 | 31±7 | <0.001 |
| Left Ventricular End Diastolic Volume Index (ml/m 2 ) | 79±27 | 92±35 | 112±38 | <0.001 |
| Left Ventricular End Systolic Volume Index (ml/m 2 ) | 47±24 | 61±32 | 78±34 | <0.001 |
| Left Atrial Area Index (cm 2 /m 2 ) | 11.3±2.6 | 12.5±3.4 | 15.1±4.6 | <0.001 |
| Restrictive Filling Pattern | 6 (3%) | 9 (12%) | 27 (29%) | <0.001 |
| Beta-blockers | 238 (89%) | 80 (86%) | 92 (84%) | 0.350 |
| Carvedilol Equivalent Dose (mg/d) | 57±26 | 55±23 | 53±24 | 0.178 |
| ACE-inhibitors/ARBs | 248 (93%) | 85 (91%) | 101 (92%) | 0.655 |
| Enalapril Equivalent Dose (mg/d) | 22±11 | 21±12 | 21±10 | 0.560 |
| Aldosterone Receptor Antagonists | 11 (4%) | 4 (5%) | 5 (5%) | 0.733 |
| Implantable Cardioverter-Defibrillator ‡ | 53 (20%) | 25 (27%) | 24 (22%) | 0.366 |
| Cardiac Resynchronization Therapy ‡ | 17 (6%) | 9 (10%) | 12 (11%) | 0.278 |
Patients with early improvement of FMR had concomitant improvement in clinical status, LV, and left atrial dimensions, such as LV systolic and diastolic functions, particularly if compared with the group with moderate-severe FMR at 6 months ( Figure 2 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


